Primary epiploic appendagitis
Images

Summary
Case 1: A 41-year-old man presented with sharp pain localized to the left upper quadrant for 1 day. The pain was exacerbated by movement and lifting. The patient complained of mild anorexia, but denied nausea, vomiting, change in bowel habits, melena, or weight loss. On physical exam he was moderately tender to palpation in the left upper quadrant. His white blood cell count, hemoglobin, and hematocrit were normal. The patient was discharged after being scheduled for an outpatient computer tomography (CT) scan.
He returned 2 days later with persistent pain. Physical exam again revealed moderate tenderness to palpation in the left upper abdomen. The patient was given an analgesic and a CT scan of the abdomen and pelvis was performed.
Case 2: A 40-year-old woman presented with constant right lower quadrant abdominal pain of 4 days’ duration. The pain was associated with nausea and exacerbated by coughing and movement. She denied fever, vomiting, or change in bowel habits. On physical exam she was moderately tender to palpation in the right lower quadrant. Her WBC was 10,100. A CT scan of the abdomen and pelvis was performed.
Imaging Findings
Case 1: A contrast-enhanced abdominal/pelvic CT scan demonstrates a 1.7-cm, oval-shaped fatty mass with peripheral ring enhancement projecting anteriorly from the descending colon (Figure 1). Surrounding inflammatory changes are present in the pericolonic fat. No peritoneal wall thickening, bowel wall thickening, or mass effect is seen.
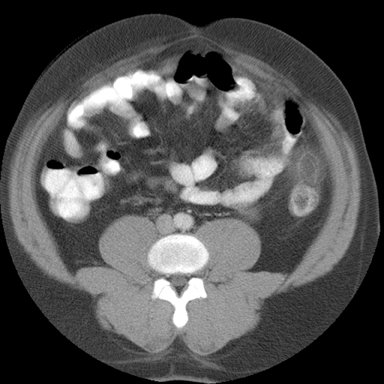
Case 2: A contrast-enhanced abdominal/pelvic CT scan shows 2.7-cm × 2-cm ovoid fatty mass with a 2-mm hyperattenuating ring and a central area of hyperattenuation projecting from the ascending colon (Figure 2). Inflammation of the surrounding fat and peritoneal wall thickening are present. The bowel wall is minimally thickened. No significant mass effect is seen on the adjacent bowel. The remainder of the scan did not demonstrate any other abnormalities.
Diagnoses
Primary epiploic appendagitis
Discussion
The appendices epiploicae are lobular pedunculated subserosal fatty masses projecting from the anterior and posterolateral walls of the ascending and descending colon. A single row projects from the transverse colon. They are numerous (typically 100), 2 cm to 5 cm in length, and most prominent along the descending and sigmoid colon. Epiploicae 15 cm in length have been reported.1 Epiploic appendagitis has a predominance for the cecum and sigmoid colon.1,2 The epiploicae are susceptible to torsion and spontaneous venous thrombosis, particularly after vigorous exertion. Presentation is typically sudden focal abdominal pain that increases with cough and stretching. Vomiting and changes in bowel habits typically are not associated complaints. The patient’s temperature and WBC count may be slightly elevated.3,4 Symptoms usually persist for 3-7 days.3 Conditions that enlarge the peritoneal cavity, such as obesity, ascites, recent pregnancy or abdominal surgery, may make the epiploicae more susceptible to torsion.1
Normal appendices epiploicae are not visualized on routine CT examinations unless there is contrast material present, such as ascites or blood.1 Epiploic appendagitis has a characteristic CT appearance described as an oval fatty mass measuring 1-4 cm in diameter of increased attenuation relative to normal fat. The defining characteristics are a hyperattenuating ring 1-3 mm thick associated with periappendageal inflammatory changes. The hyperattenuating ring is thickened visceral peritoneal lining. The center of the fatty mass may contain a linear or rounded area of hyperattenuation due to thrombosed vessels, hemorrhagic necrosis, apposition of two adjacent appendices, or septal fibrosis. Mass effect on the adjacent bowel wall and peritoneal or bowel wall thickening may also be present.3-5
Follow-up CT scans demonstrate a decrease in size of the lesions with a change in shape to irregular, oval, or rounded. Changes in the attenuation of the involved epiploicae vary from decreasing attenuation to increasing attenuation. Periappendageal fat stranding and adjacent bowel-wall changes typically resolve with healing.4,5 CT findings may persist for more than 19 weeks.4
Primary epiploic appendagitis’ clinical presentation and CT appearance are similar to that of segmental omental infarction (SOI). Segmental omental infarction can be differentiated from epiploic appendagitis by its heterogeneous appearance, medial location with respect to the ascending and descending bowel, and lack of peripheral enhancement. SOI is also larger and causes greater mass effect on the adjacent bowel.3,6,7 Since both are treated conservatively, differentiation is of no clinical consequence.6,7
Differential diagnosis should also include secondary epiploic appendagitis, diverticulitis, appendicitis, and cholecystitis. Secondary epiploic appendagitis is caused by inflammation of adjacent organs, most commonly due to diverticulitis.1,5 Primary epiploic appendagitis can only be diagnosed when findings for diverticulitis and appendicitis are absent.6,7
Conclusion
Epiploic appendagitis, once thought to be a rare condition, is now more commonly diagnosed with the routine use of CT scans in the evaluation of abdominal pain. It has a characteristic CT appearance of an oval-shaped fatty mass of increased attenuation surrounded by an enhancing ring and periappendigeal fat stranding. Since epiploic appendagitis is treated conservatively, its diagnosis can prevent unnecessary surgical procedures.
References
- Ghahremani G, White E, Hoff F, et al. Appendices epiploicae of the colon: Radiologic and pathologic features. Radiographics. 1992;12:59-77.
- Lynn T, Dockerty M. A clinicopathologic study of the epiploic appendages. Surg Gynecol and Obstet. 1956;103:423-433.
- Rioux M, Langis P. Primary epiploic appendagitis: Clinical, US, and CT findings in 14 cases. Radiology. 1994;191:523-526.
- Rao P, Wittenberg J, Lawrason J. Primary epiploic appendagitis: Evolutionary changes in CT appearance. Radiology. 1997;204:713-717.
- Sirvanci M, Tekelioglu M, Duran C, et al. Primary epiploic appendagitis CT manifestations. J Clin Imaging. 2000;24:357-361.
- van Breda Vriesman A, de Mol van Otterloo A, Puylaert J. Epiploic appendagitis and omental infarction. Eur J Surg. 2001;167:723-727.
- Mcclure M, Khalili K, Sarrazin J, Hanbidge A. Radiological features of epiploic appendagitis and segmental omental infarction. Clin Radiol. 2001;56:819-827.
Related Articles
Citation
. Primary epiploic appendagitis. Appl Radiol.
February 1, 2013