Best Practices for 68Ga-PSMA-11 PET Imaging: Dose Optimization From Real-World Insights
Images
Prostate-specific membrane antigen (PSMA) positron emission tomography (PET) imaging using68Ga-PSMA-11 is an integral tool for the detection and management of prostate cancer, particularly for patients with suspected metastasis who are candidates for initial staging, with suspected biochemical recurrence, and with metastatic castration-resistant prostate cancer who are candidates for PSMA-directed radioligand therapy.1-4
The clinical efficacy and safety of dosing patients with 3 to 7 mCi, as per US prescribing information, is well established.1,4,5 We present best practices for dosing based on foundational principles of nuclear medicine and extensive real-world experience from our high-volume site where we utilize a standard dose of 6 to 7 mCi as best practice.
In PET imaging, the final image quality is fundamentally tied to the number of detected coincidence events, which is influenced positively by higher radiotracer dose and longer scan times and negatively by larger patient body habitus and older PET scanner technology.6-8 Higher injected doses result in greater positron emissions, leading to increased count statistics and, theoretically, improved image quality; however, this relationship is not linear and exhibits a peak at moderate dose levels.7 Longer scan time may also improve image quality by increasing coincidence events; however, it often negatively impacts patient comfort and overall experience.7 Conversely, larger body habitus often lead to greater photon attenuation and scatter, which can reduce image quality if not accounted for.8 Additionally, older PET scanner technology may have impaired count-rate capabilities, producing images with high noise, and have a short axial field of view, limiting detection sensitivity and image resolution.9-12 In a retrospective analysis of 856 patients with biochemically recurrent prostate cancer who underwent68Ga-PSMA-11 PET, detection rates were 10% higher with the newer PET system (76%) compared to an older model (66%).9 Notably, over 50% of PET scanners in the US were installed prior to 2014.13,14
For reasons discussed above, many physicians and sites have started to follow a best practice of dosing patients within the 6 to 7 mCi range, with over 1,000 patients having received a 6 to 7 mCi dose of68Ga-PSMA-11 to date.15 Our site experi- ence further supports this best practice. We present a series of case images taken on a Siemens Biograph mCT-S (40) 3R PET/ CT scanner (scanner introduced to the US market in 2009) from patients across a wide array of body habitus (body mass index [BMI] range, 25 to >40 kg/m2) and several with micrometastatic disease.
These real-world cases are intended to support clinicians with practical insights and rationale for establishing this best practice, which further augments the flibility and optimal imaging allotted with68Ga-PSMA-11 PET.
Patient #1
A 67-year-old male with a BMI >25 kg/m2 underwent robot-assisted laparoscopic prostatectomy (RALP) for clinically localized prostate adenocarcinoma. Final pathology revealed pT3aN0M0 disease with a Gleason score of 4+3=7 and a preoperative prostate-specific antigen (PSA) level of 6.85 ng/mL. Postoperatively, the patient exhibited a persistently detectable PSA level of 0.25 ng/mL. A year later,68Ga-PSMA-11 PET/CT (7.0 mCi; 54-minute uptake; 2 minutes/bed for 10 beds; total scan time 20 minutes) demonstrated radiotracer uptake in pelvic lymph nodes, consistent with regional metastatic involvement (Figure 1). The patient is scheduled to undergo salvage radiation therapy in conjunction with androgen deprivation therapy (ADT), including relugolix and apalutamide.
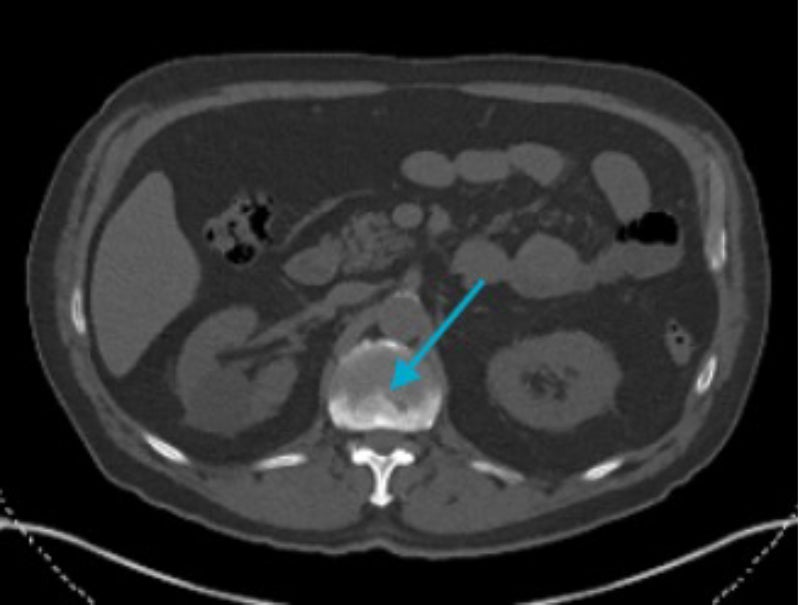
Patient #2
A 73-year-old male with a BMI of 27.8 kg/m2 and a history of unfavorable intermediate-risk prostate adenocarcinoma (clinical stage cT1c, PSA 5.4 ng/ mL, Gleason score 3+4=7) underwent definitive external beam radiation therapy with concurrent ADT. Despite initial biochemical response, 4 years later, the patient’s PSA increased from 0.05 ng/mL to 0.31 ng/mL while on apalutamide and degarelix; thus,68Ga-PSMA-11 PET/CT (6.9 mCi; 76-minute uptake; 2.5 minutes/bed for 10 beds; total scan time 25 minutes) was conducted and demonstrated radio-tracer uptake localized to the prostate, suggestive of intraprostatic recurrence (Figure 2). The patient’s current management plan includes salvage stereotactic body radiation therapy (SBRT) to the prostate and a change in systemic therapy.
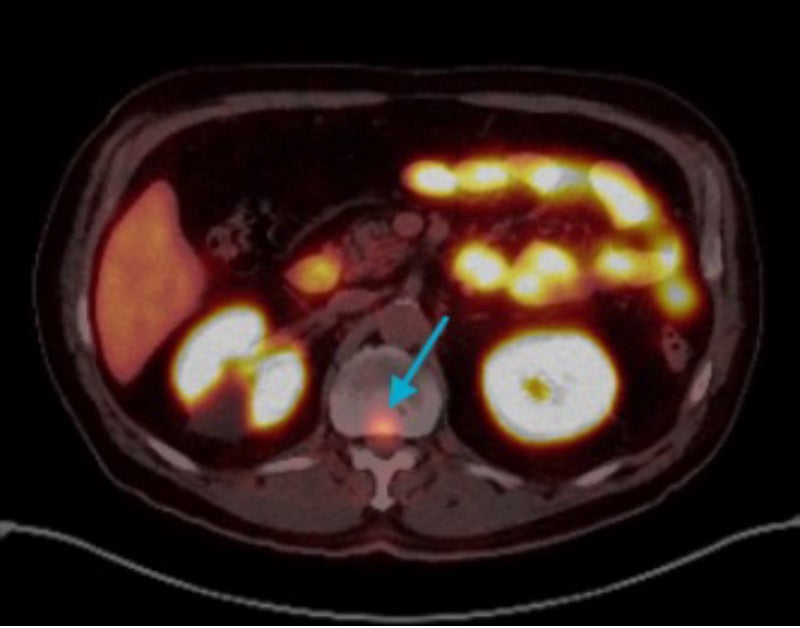
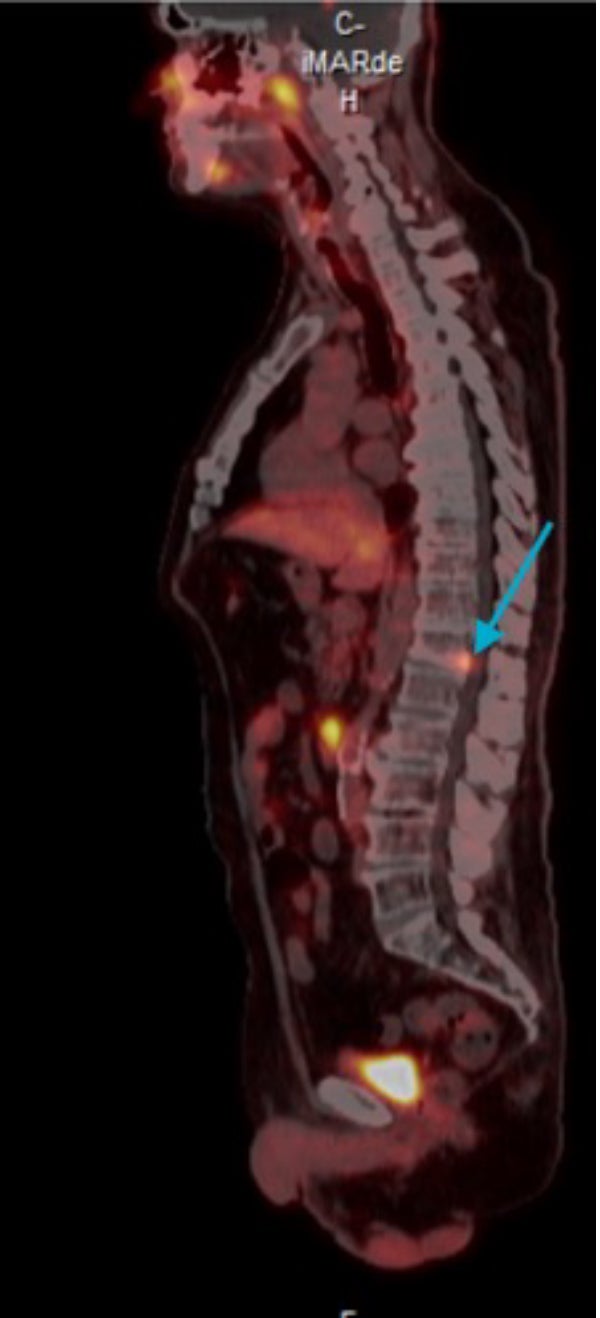
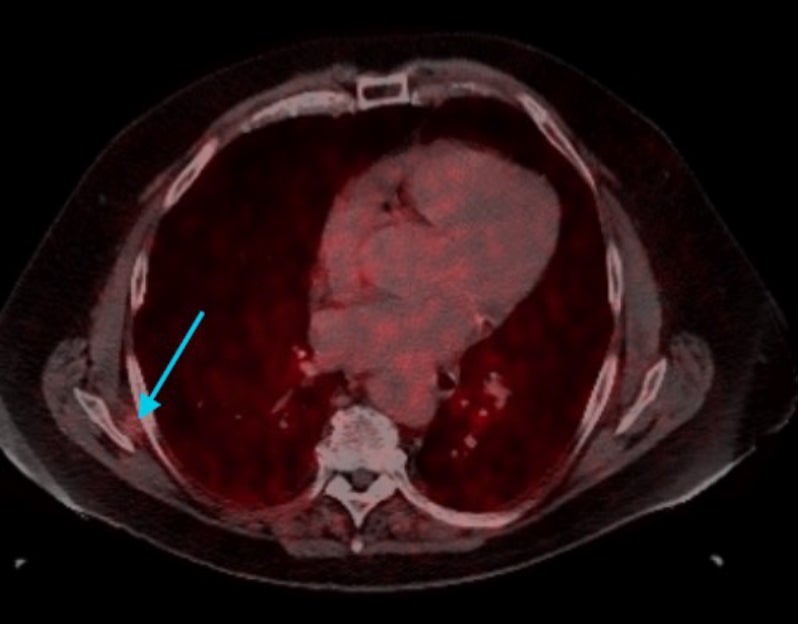
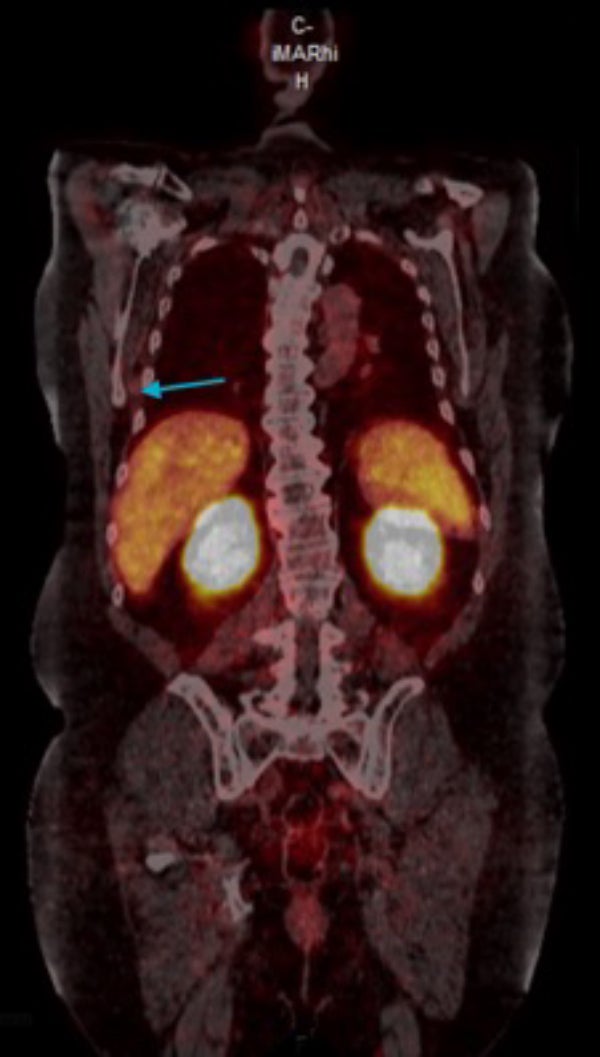
Patient #3
A 75-year-old male with a BMI of >30 kg/m2 and a history of high-risk prostate adenocarcinoma underwent RALP. Final pathology revealed pT3aN1 disease with a preoperative PSA of 7.4 ng/mL, Gleason score 4+4=8, positive lymph nodes, lymphovascular invasion, and positive surgical margins. Following biochemical recurrence, the patient was initiated on ADT.68Ga-PSMA-11 PET/CT imaging demonstrated radio-tracer uptake in both the prostate bed and spleen. He subsequently completed radiation therapy to both sites. Most recently, the patient’s PSA, previously undetectable, increased to 0.19 ng/mL. Repeat68Ga-PSMA-11 PET/CT (6.9 mCi; 54-minute uptake; 2.5 minutes/bed for 10 beds; total scan time 25 minutes) identified a new site of uptake at the T12 vertebral level (Figure 3). The current management plan includes SBRT to the T12 lesion.
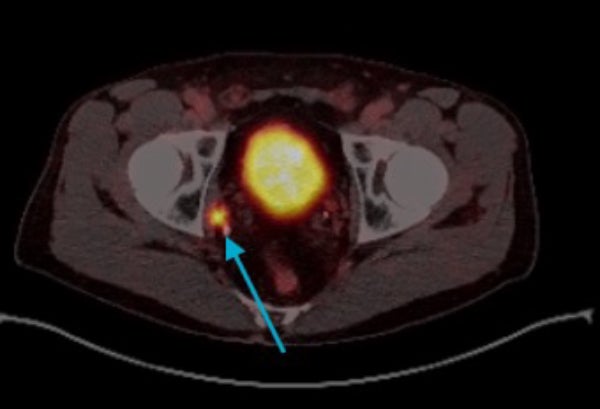
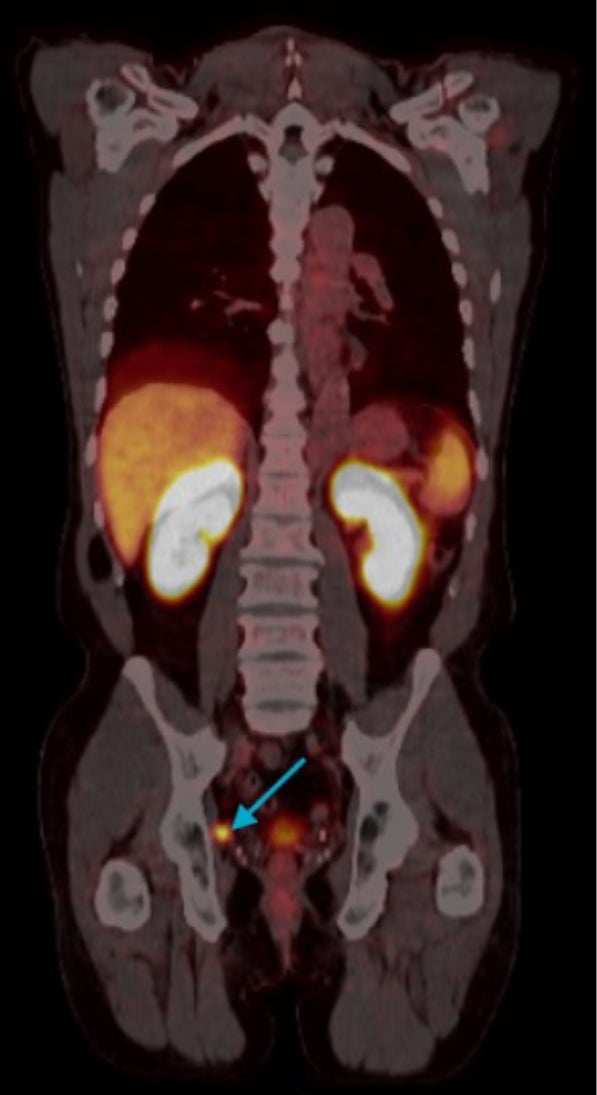
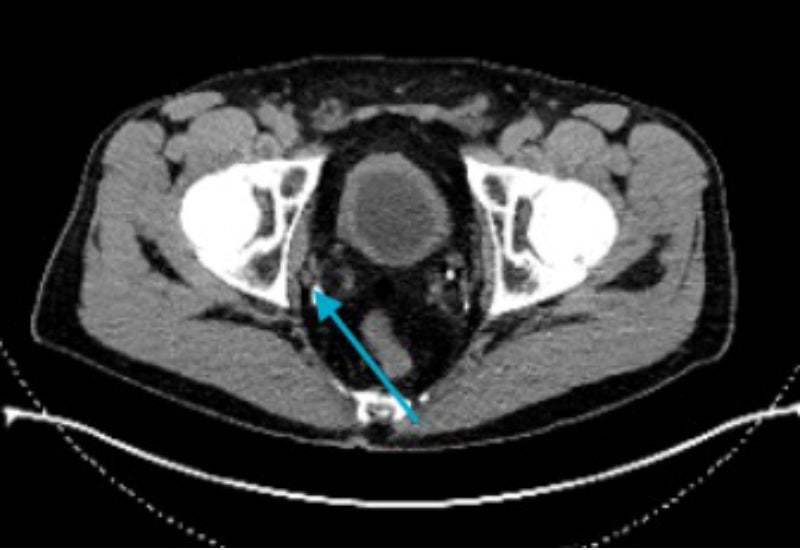
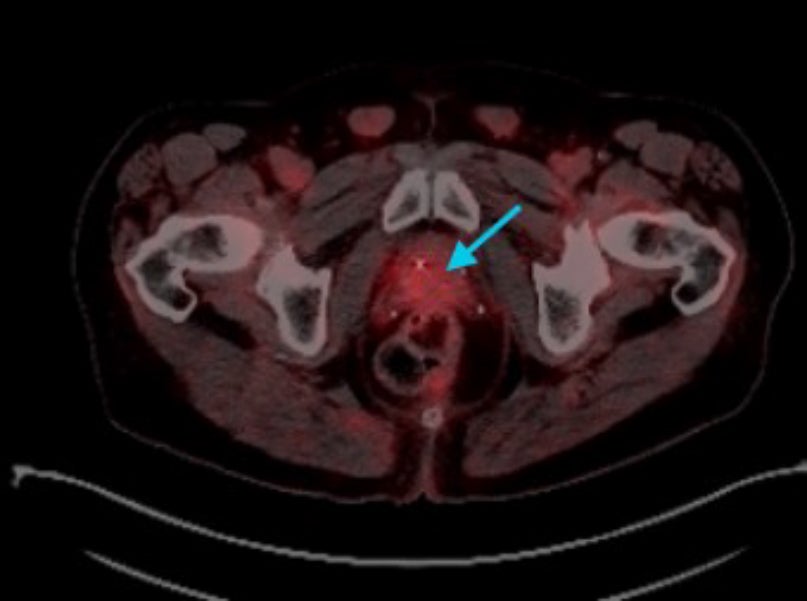
Patient #4
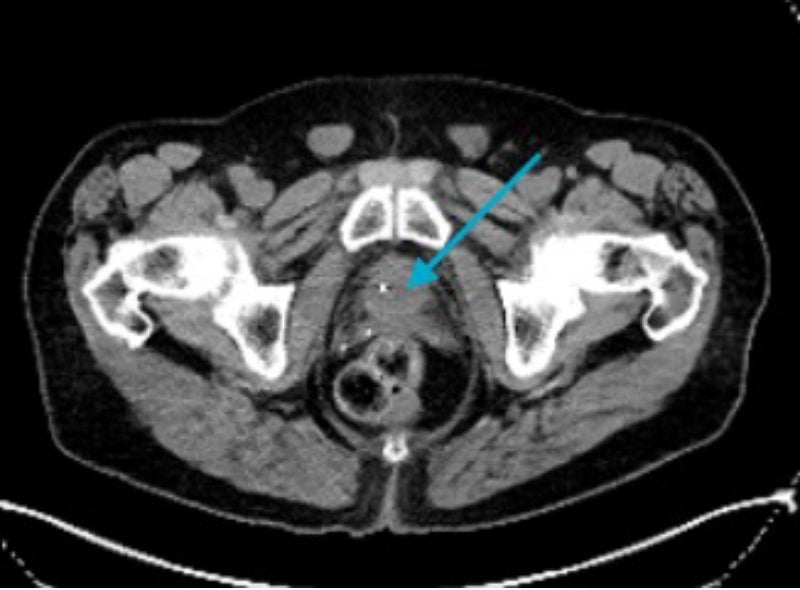
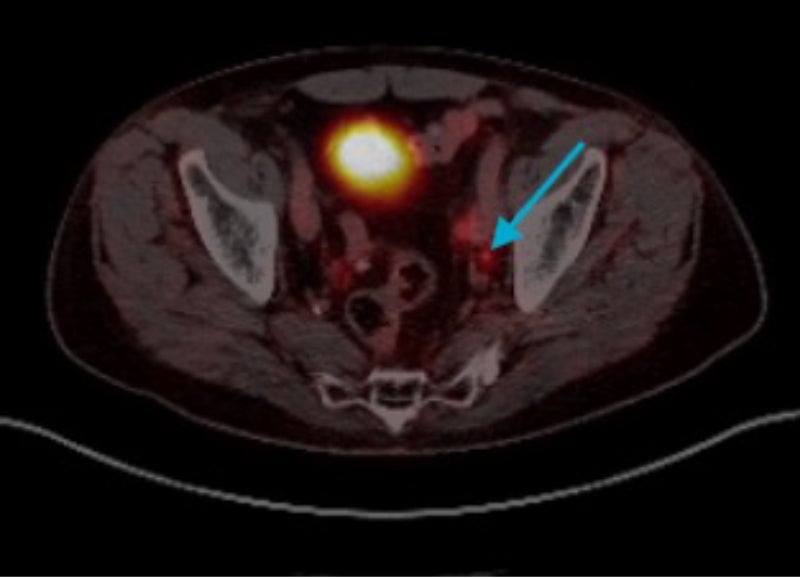
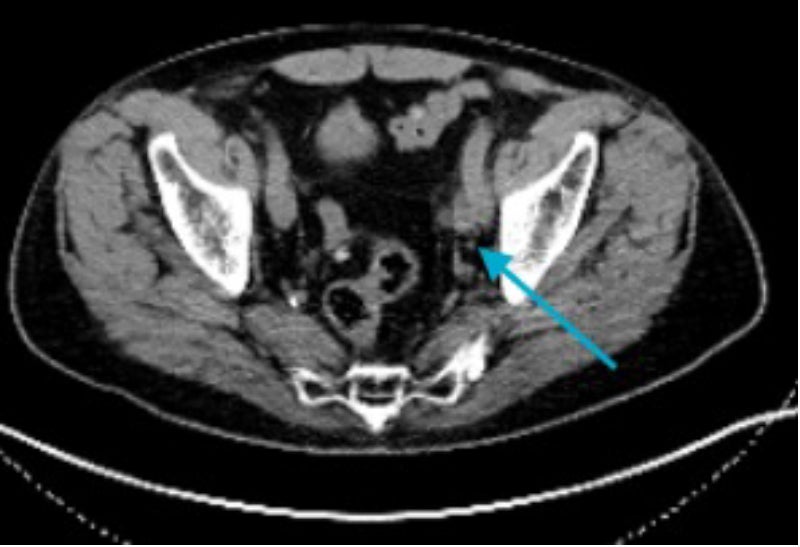
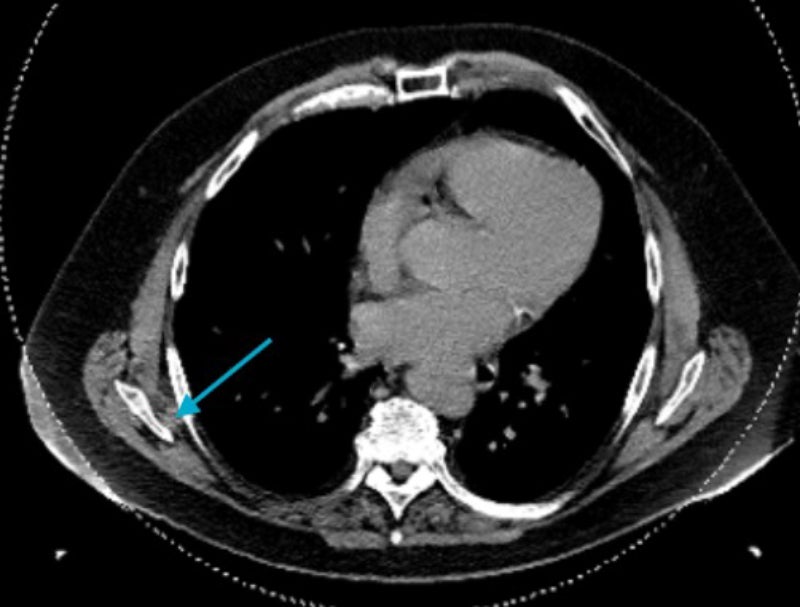
A 77-year-old male with a BMI of 28.1 kg/m2 and a history of high-risk prostate adenocarcinoma (clinical stage cT4N0M0, PSA 13.3 ng/mL, Gleason score 4+5=9) was initially treated with ADT and EBRT. He later developed locoregional recurrence involving the prostate gland and a single pelvic lymph node. Management included SBRT to the involved node in combination with continued ADT and the addition of darolutamide, with EBRT completed thereafter. Subsequently, his PSA, previously undetectable, increased to 0.05 ng/mL.
Ga-PSMA-11 PET/CT (7.0 mCi; 65-minute uptake; 2.5 minutes/bed for 9 beds; total scan time 22.5 minutes) revealed new radiotracer uptake in a left external iliac lymph node (Figure 4). The current management plan includes a change in systemic therapy.
Patient #5
A 70-year-old male with a BMI of 40 kg/m2 and a history of prostate adenocarcinoma (pathologic stage pT2cN0, Gleason score 3+4=7) underwent RALP. He subsequently received salvage EBRT with ADT for biochemical recurrence. Five years later, he developed oligometastatic disease involving the T11 spine, which was treated with SBRT. His PSA has remained undetectable for over a year.
The patient recently expressed interest in initiating testosterone supplementation. A precautionary68Ga-PSMA-11 PET/CT (7.0 mCi; 56-minute uptake; 3.0 minutes/bed for 10 beds; total scan time 30 minutes) was performed, revealing radiotracer uptake in the right sixth rib (Figure 5). The current management plan includes SBRT to the identified site.
Conclusion
Our case series highlights the clinical feasibility and diagnostic value of the best practice of administering 6 to 7 mCi of68Ga-PSMA-11 to patients. We demonstrate high image quality on 16-year-old scanner technology in patients with low PSA levels and across a range of BMIs (25 to >40 kg/m2). These real-world examples not only illustrate the flexibility of this dosing strategy across diverse body habitus but also highlights its potential to augment detection efficacy and impact clinical decision making.
Importantly, the increased administered activity appears to contribute to improved image quality by increasing number of coincidence counts,7 which allows for the possibility to shorten scan duration and enhance patient comfort and overall experience. This has meaningful implications for clinical workflow efficiency, particularly in settings utilizing older PET technology where scan time and image resolution are often constrained.9-12 By following the best practice of a 6 to 7 mCi dosing strategy for68Ga-PSMA-11, institutions may achieve both clinical and cost-saving benefits.
References
- Illuccix (kit for the preparation of gallium Ga68 gozetotide injection) prescribing information. Telix Pharmaceuticals; 2024.
- Bryce AH, Agarwal N, Beltran H, et al. Implementing evidence-based strategies for men with biochemically recurrent and advanced prostate cancer: Consensus recommendations from the US Prostate Cancer Conference 2024. Cancer. Jan 1 2025;131(1):e35612. doi:10.1002/cncr.35612
- EAU Guidelines. Edn. presented at the EAU Annual Congress Madrid 2025. ISBN 978-94-92671-29-5. 2025.
- Gozellix (kit for the preparation of gallium Ga68 gozetotide injection) prescribing information. Telix Pharmaceuticals; 2025.
- Purysko AS, Abreu AL, Lin DW, Punnen S. Not all prostate-specific membrane antigen imaging agents are created equal: diagnostic accuracy of Ga-68 PSMA-11 PET/CT for initial and recurrent prostate cancer. Applied Radiology. 2024.
- Moses WW. Fundamental Limits of Spatial Reso- lution in PET. Nucl Instrum Methods Phys Res A. Aug 21 2011;648 Supplement 1:S236-s240. doi:10.1016/j. nima.2010.11.092
- Karakatsanis NA, Fokou E, Tsoumpas C. Dosage optimization in positron emission tomography: state-of-the-art methods and future prospects. Am J Nucl Med Mol Imaging. 2015;5(5):527-47.
- Rajapakse CS, Chang G. Impact of body habitus on radiologic interpretations. Acad Radiol. Jan 2014;21(1):1-2. doi:10.1016/j.acra.2013.10.006
- Ataya M, Bahler CD, Koch M, et al. Can the sensitivity of prostate cancer with68Ga-PSMA PET/ CT improve with newer higher resolution PET-CT cameras? J Urol. 2025;213(5S):e1098.
- Chen W, Li Y, Li Z, et al. Advantages and Challenges of Total-Body PET/CT at a Tertiary Cancer Center: Insights from Sun Yat-sen University Cancer Center. J Nucl Med. May 6 2024;65(Suppl 1):54S-63S. doi:10.2967/jnumed.123.266948
- Vaquero JJ, Kinahan P. Positron Emission Tomography: Current Challenges and Opportu- nities for Technological Advances in Clinical and Preclinical Imaging Systems. Annu Rev Biomed Eng. 2015;17:385-414. doi:10.1146/annurev-bio-eng-071114-040723
- Surti S, Pantel AR, Karp JS. Total body PET: Why, how, what for? TRPMS. 2020;4(3):283-292. doi:10.1109/TRPMS.2020.2985403
- Feder J. Medical equipment continues to age in the Unites States. Radiology Oncology Systems. Accessed 6 Feb, 2025. https://www.oncologysystems. com/blog/medical-equipment-continues-to-age-in- the-united-states/
- Young L. IMV: PET/CT drivers PET scan volume to new heights. AuntMinnie.com. Accessed 6 Feb, 2025. https://www.auntminnie.com/clinical-news/ molecular-imaging/article/15623310/imv-pet-ct- drives-pet-scan-volume-to-new-heights
- Data from: Data on File. 6-7 mCi orders.2025.
Citation
Best Practices for 68Ga-PSMA-11 PET Imaging: Dose Optimization From Real-World Insights. Appl Radiol.
July 16, 2025