Comparison of magnetic resonance angiography and computed tomographic angiography
Images










Dr. Gor is Chief Resident in Diagnostic Radiology at New Jersey Medical School, Newark, NJ. He completed medical education from Seth G.S. Medical College/King Edward Memorial Hospital, Mumbai, India and preliminary medicine internship at the University of Tennessee at Memphis in June 2000. He will start a Fellowship in Neuroradiology at University of Pennsylvania, Philadelphia, PA, in July 2004.
Traditionally, time of flight (TOF) and phase contrast (PC) magnetic resonance angiography (MRA) have been used to study arteries and veins. In TOF MRA, a gradient pulse is repeatedly applied to a slice/slab (two-dimensional [2D]/three-dimensional [3D]) of tissue. The signal from the stationary tissue decreases and becomes more saturated with each pulse. The moving blood brings unsaturated protons into the tissue slice, which generates a high signal intensity. The contrast in TOF imaging is thus provided by suppressing the stationary tissue signal intensity in conjunction with the high signal intensity from moving blood. 1 In PC MRA, the applied gradient imparts a phase shift to the inflowing protons proportional to their velocity. Two data sets are acquired with opposite sensitization resulting in opposite phase for moving protons and indentical phase for the stationary protons. On subtraction of the data sets, signal from stationary protons is eliminated and just the moving protons are seen. Information about the quantity and direction of flow is obtained. 2
In TOF MRA, if the vessel is oriented horizontally within the selected slice, the gradients that suppress the stationary tissue also suppress the signal from moving blood. This leads to a decrease in signal due to saturation. In PC MRA, turbulent flow leads to intravoxel dephasing of protons resulting in a decrease in signal that is also responsible for overestimation of a stenosis. Appropriate velocity encoding is vital for correct interpretation. These techniques have largely been replaced by contrast-enhanced MRA (CE-MRA), which uses a 3D spoiled gradient-echo sequence with intravenously administered gadolinium (Gd). Gadolinium reduces the T1 relaxation of blood significantly, so as to produce a very high signal from the blood compared with that from surrounding tissue. 3,4 The timing of image acquisition is of paramount importance to image the artery without significant venous signal contamination. Various commercial methods like SmartPrep (GE Medical systems, Waukesha, WI), CareBolus (Siemens Medical Systems, Iselin, NJ), and BolusTrak (Phillips Medical Systems, Bothell, WA) are available to automatically determine the optimal imaging time. Administering a test bolus followed by MR fluoroscopic imaging to observe the time of maximum arterial concentration is often very helpful.
K-space contains the spatial frequencies of the signal obtained from a tissue slice. These spatial frequencies are converted to an image by inverse Fourier transformation. The center of the k-space contains the contrast information. Hence, the center of the k-space should be acquired at the peak arterial concentration of Gd. Two such alternate k-space schemes are centric phase ordering and elliptical centric-phase ordering. 5 For each, data can be processed to view maximum intensity projection (MIP) images, multiplanar reformations (MPR), or 3D surface projection images.
In single-detector computed tomography (SDCT), a fan-shaped beam traverses the patient and is detected by a single row of detectors. The information at the edges of the beam is lost, resulting in poor resolution along the z-axis. The pitch is equal to table feed per rotation divided by slice thickness. Increasing the scan speed or the area of coverage necessitates increase in pitch. This results in degradation of the z-axis resolution because noncontiguous images are obtained. 6 Multiple rows of detectors were added in the Z direction to solve this problem. The detectors at the periphery are now able to detect data at the edge of the fan beam, thereby improving spatial resolution along the z-axis. In this method of imaging, a contrast bolus is administered through a peripheral vein, and scanning is commenced during the arterial phase. As with CE-MRA, commercial products that optimize the timing of the scan are available. MIP images, MPR images, and volume-rendered images, are used for analysis. With 16-channel multidetector CT (MDCT), volumetric data are obtained with near-isotropic resolution 7 (resolution equal in all planes), which is very important to visualize small vessels, and produce excellent reformations. The capability for near-isotropic imaging is responsible for the superior spatial resolution of CT over MR imaging. MDCT has faster acquisitions, covers a larger area, and significantly reduces the amount of injected iodinated contrast necessary as compared with single-detector CT. 8,9 The single breath- hold acquisition eliminates artifacts due to respiratory excursion and body movement, giving a superior image quality.
Clinical applications: Computed tomography angiography and magnetic resonance angiography
Intracranial and extracranial carotid arteries
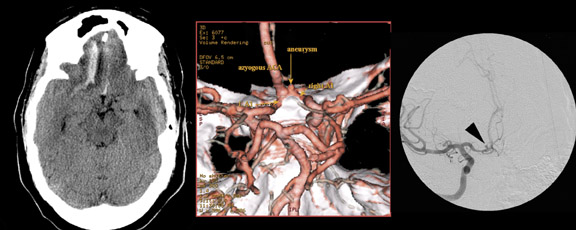
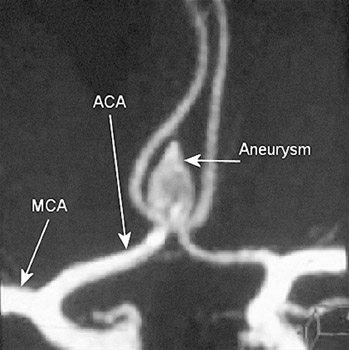
The prime indications for imaging the intracranial vasculature are for the detection and treatment planning of aneurysms and the evaluation of specific clinical situations related to steno-occlusive disease. Autopsy studies indicate that aneurysms <5 mm in diameter are unlikely to rupture. 10 This dimension is usually the cutoff for treating asymptomatic aneurysms. 11-13 CT angiography (CTA) and MRA combined have the potential to replace catheter angiography for diagnosis (Figures 1 and 2). A thin-section (1.25 mm/2.5 mm), contrast-enhanced MDCTA is performed with 3D volu-metric and MIP reformations. Traditionally, 2D/3D TOF had been the MR imaging technique. Currently, 3D TOF CE-MRA and time-resolved CE-MRA are preferred. 3D TOF CE-MRA has improved spatial resolution, less saturation effects and intravoxel dephasing, and better evaluation of aneurysm lumen. With this technique, imaging is not significantly affected by the presence of hemorrhage. The high signal from the stationary tissue due to T1 contamination artifact of blood is eliminated by subtraction of the pre-enhancement volume from the contrast-enhanced time frame. 14
MDCTA and MRA reliably detect aneurysms >=3 mm in diameter. 15 Several reports confirm their sensitivity and specificity as being similar to catheter angiography. 16-18 MDCTA better defines the anatomic configuration and surroundings of the aneurysm and has the advantage of showing the relationship of the aneurysm to bone, which is necessary for surgical planning. 19 The entire scan can be completed in 30 seconds, minimizing motion artifacts. Aneurysms in the cavernous sinus and skull base can be difficult to detect by MDCTA. MRA is better suited for their evaluation. 20 The postprocessing of CTA mandates the time and attention of a skilled operator. In addition to general advantages, CE-MRA on a 3T magnet with fast gradient techniques provides an especially accurate depiction of cerebral aneurysms. 21
Three-dimensional TOF (noncontrast at 1T) MRA has a sensitivity and specificity of 92% and 91%, respectively, for detecting intracranial stenosis exceeding 50% of the width of the vessel lumen. 22 CTA has a sensitivity and specificity of 100% and 99%, respectively, for the same degree of stenosis. MRA has a tendency to overestimate the extent of stenosis; however, calcification in the arterial wall can eventuate in a nondiagnostic study by CTA. A limitation of MRA is that it cannot be performed in claustrophobic patients or in patients with pacemakers, certain implants, or aneurysm clips. Sixteen-channel MDCT has the potential to reduce artifacts due to surgical clips and calcification (this requires further verification).
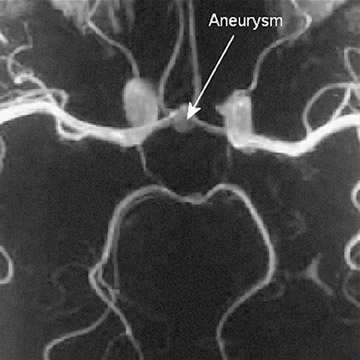
Atherosclerosis is the most frequent indication to image the
extracranial carotid arteries. Endarterectomy has been shown to be
beneficial in patients with a stenosis of greater than 70%.
23-25
Investigators from the Asymptomatic Carotid Artery Study
25
have suggested that asymptomatic patients with a stenosis of 60%
can benefit from endarterectomy by reducing stroke risk. MDCTA and
CE-MRA
are accurate and reliable methods of detecting carotid stenosis
(Figure 3). Recently, Linera et al
26
reported that the sensitivity and specificity of CE-MRA in
detecting carotid stenosis of greater than 70% to be 97.1% and
95.2%, respectively. In the same study the sensitivity and
specificity of CTA were quoted to be 74.3% and 97.6%, respectively.
The results of CTA in this study may be suboptimal, as a
single-detector CT was used to perform the CTA. Sensitivity and
specificity for MDCTA are typically close to 100%.
27-29
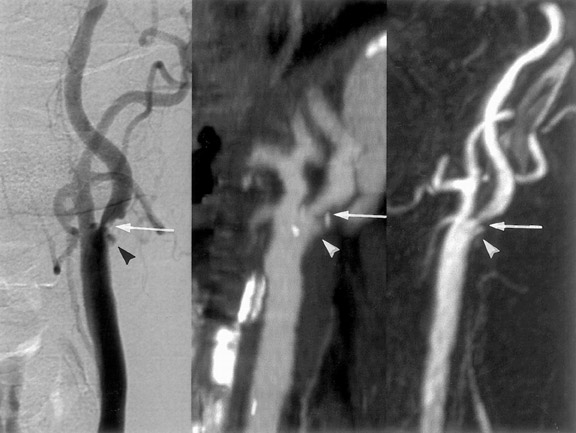
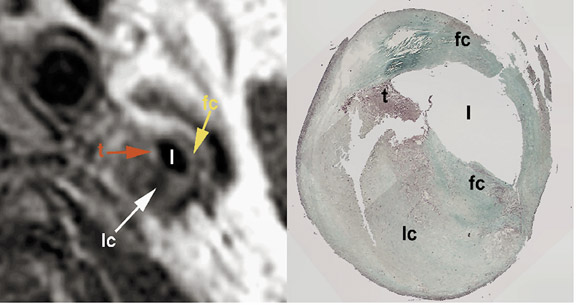
Besides discerning the degree and length of stenosis, plaque
irregularity, ulceration, and characterization (in terms of lipid,
thrombus and calcification) can be done with both techniques.
30
MDCTA has been shown to be slightly superior to MRA for detecting
plaque irregularities, whereas plaque ulceration, which is a
frequent precursor of emboli, is better seen with MRA. It has been
suggested that plaque characterization by MRA may be used in
treatment planning of atherosclerotic disease
31,32
(Figure 4). One must be aware of pitfalls of each technique. Vessel
wall calcification limits the accuracy of MDCTA. Overestimation of
stenosis can occur with CE-MRA.
33
Coronary arteries
In the year 2000, 1.32 million in-patient diagnostic coronary angiographic examinations were performed in the United States. 34 The number of diagnostic examinations exceeded those performed as a part of coronary angioplasty or stent placement. 34 There is a need and a great potential to image the coronary arteries noninvasively so as to avoid the risks associated with catheter angiograms and to minimize exposure to ionizing radiation.
MDCTA of the coronary arteries is performed after intravenous injection of 80 to 120 mL of contrast medium at the rate of 3 to 5 mL/sec followed by a saline bolus chase. Spiral scanning using 8 or 16 slices is performed with a digital electrocardiography (EKG) and oversampling of scan projections. 35,36 This allows retrospective EKG gating, creating images in the same phase of the cardiac cycle.
Currently, 3D segmented k-space gradient-echo/echoplanar MRA is performed with the navigator respiratory compensation technique. A 30-mm slab with overlapping 20 slices of 3-mm thickness is obtained. The process takes only 10 to 12 minutes per 3D acquisition. 37
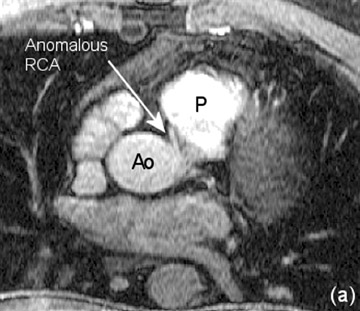
Applications: Coronary vascular anomalies-- Both CE-MRA and MDCTA have been shown to be equivalent to catheter angiography for the detection of coronary vascular anomalies. Due to enhanced temporal resolution of CE-MRA, it has the ability to visualize the anatomic path taken by the contrast (Personal communication, Martin Prince, MD, PhD, Weill Medical College of Cornell University, New York, New York, July 2003). CE-MRA could be used primarily to detect vascular anomalies and to evaluate cases deemed equivocal by other modalities (Figure 5).
Applications: Detection of bypass graft stenosis-- Engelmann et al 38 have reported contrast-enhanced 3D gradient- echo technique to have a sensitivity of 92% and a specificity of 85% for the detection of graft stenosis. The use of 2D spin-echo and gradient-echo techniques allows the visualization of flow in 2 successive slices to correlate with patency, while flow in 1 slice is equivocal, and no flow indicates occlusion. 37 The sensitivity and specificity of MDCTA for graft stenosis are 97% and 89%, respectively, slightly higher than those reported for the current CE-MRA technique. 39
Applications: Detection of native vessel stenosis-- In a recent multicenter study, Kim et al 40 have reported a sensitivity of 88% to 100%, and a specificity of 44% to 88% for the detection of significant (>50%) native coronary stenosis. Several recent studies have determined the sensitivity and specificity of MDCTA to range from 85% to 89% and 76% to 99%, respectively. 41-44 MDCTA can now reveal near-isotropic resolution of at least 0.6 mm, allowing visualization of the distal small coronary branches (Figure 6). A calcium score can be obtained. A low calcium score has a high negative predictive value for coronary artery disease (CAD). 45 Retrospective EKG gating also allows functional information such as left ventricular ejection fraction and anatomic detail such as left ventricular wall thickness to be obtained from the same acquisition; however, this is best evaluated by MR imaging. With the latest improvement in spatial resolution coupled with better techniques to suppress motion and the potentially confounding influence of epicardial fat, MRA can serve as a "one-stop" examination in the detection of CAD. 46
Coronary artery disease is a major health problem causing significant morbidity in the expanding elderly population. A test to detect CAD should be noninvasive, reliable, safe (does not involve ionizing radiation), and inexpensive. Coronary MRA has some of these virtues. A meta-analysis was performed to investigate the efficacy of MRA compared with catheter angiography in the detection of significant coronary artery stenosis.
A Medline search was performed with the key words "coronary MR angiography." English language studies from 1993 to 2003 comparing current MRA technique (3D gradient or echo- planar imaging) with catheter angiography were selected. After excluding 2D MR techniques, 20 studies were identified. Strict inclusion criteria based on recommendations of Oxman et al 47 were applied (Table 1).
Nine studies (Table 2), met the criteria, and 11 studies were excluded (Table 3). For each study, 2 * 2 tables (true positive, true negative * false positive, false negative) were constructed. Based on the number of coronary segments evaluated, overall sensitivity and specificity of coronary MRA for the detection of significant stenosis were calculated. The meta-analysis was limited, as only two variables (sensitivity and specificity) were evaluated. Due to the small number of studies that met the inclusion criteria, other variables, such as the effect of sample size on sensitivity and specificity, could not be evaluated.
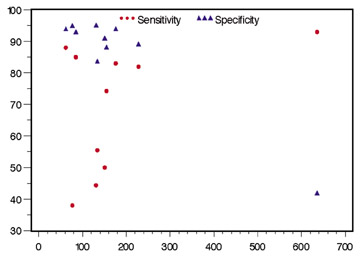
The study by Kim et al
40
had the maximum number of coronary segments evaluated, more than
all other studies combined. The total visible segments varied from
62 to 636, the sensitivity ranged from 44% to 93%, and the
specificity ranged from 42% to 95% (Figure 7). There was a high
level of interobserver variability for the determination of
sensitivity of coronary MRA for significant stenosis. The
specificity was near constant. The overall sensitivity and
specificity of coronary MRA in the detection
of significant stenosis were 83% and 82%, respectively.
MRA holds promise to be a safe, noninvasive, and an efficient test in evaluating the coronary arteries. Technical advancements, such as faster imaging sequences, and prospective double-blinded studies are needed to evaluate the full extent of its clinical usefulness.
Pulmonary artery
The most frequent indication to image the pulmonary arteries is pulmonary embolism (PE). Conventional angiography is not possible in up to 20% of patients due to its invasiveness, associated sporadic mortality, and morbidity. 67 CTA and MRA are faster, less invasive, and associated with a smaller number of complications. 67,68 MDCTA and MRA have similar efficacy in diagnosis of main, lobar, and segmental pulmonary artery emboli (Figures 8 and 9). Oudkerk et al 69 report a sensitivity of 84% for segmental, and 100% for main and lobar arteries when using CE-MRA with a specificity of 98%, when compared with catheter angiography. Studies using helical CT have quoted sensitivity and specificity of 90% for diagnosis of pulmonary embolism. 70 The advantage of MDCTA is fast imaging and wide availability. The disadvantage is that in a patient population with a high risk of PE, it is not performed in up to 12% due to renal failure. 71 In 1% to 10% of patients, CTA is suboptimal for radiologic evaluation. 72,73
The drawback of CE-MRA is long imaging time. For good-quality images, breath-holding for at least 10 to 15 seconds for each lung acquisition is necessary, 69 which may not be possible in patients with dyspnea. Haage et al 74 report a detection rate of emboli of 97.7% by using real-time MRA without breath-holding in animal studies. Initial reports of protocols to image the pulmonary arteries in <4 seconds 75 have also been described and are very promising, but lack prospective confirmation. The advantage of CE-MRA is simultaneous evaluation of lung ventilation and perfusion in the same examination. 76,77 In patients with PE and negative compression duplex ultrasonography (CDUS), MR venography shows thrombus in pelvic veins in up to one-third of the patients. 78 This is done during the same examination, and avoids exposure to radiation and iodinated contrast as compared with methods for CT venography. Recent experimental studies show CE-MRA to be superior to CTA in diagnosis of subsegmental pulmonary emboli 79 ; however, the management of patients with isolated subsegmental PE is controversial. At present, MDCTA is widely employed; however, CE-MRA has the same efficiency and more advantages than MDCTA.
Imaging of the aorta
Aortic dissection-- Acute aortic dissection is a cardiovascular emergency with a preadmission mortality of 21%. 80 The role of imaging is to recognize the dissection, reveal the entry point, display branch vessel involvement and demonstrate aortic regurgitation and hemopericardium. In the ascending aorta, intramural hematoma (wall thickening >7 mm due to hemorrhage in the vessel wall, in the absence of an intimal flap) is a precursor to dissection. Its presence is associated with rapid progression to dissection. 81
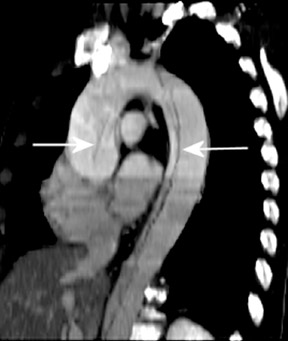
MDCTA is a rapid imaging tool to detect dissections. The sensitivity/specificity of CTA has improved from 94%/87% 82 to 100%/100% 83,84 as CT technology has evolved from single-detector to MDCT (Figure 10). Because of high spatial resolution, CTA is considered superior to MRA and transesophageal echocardiography (TEE) in identifying branch vessel involvement. 83 Both CTA and MRA are more accurate than TEE for determining the distal extent of a dissection (Figure 11). However, CTA cannot detect aortic regurgitation, which is often the cause of death. 85
In a large retrospective study, evaluating the current imaging modalities for the detection of dissection, Moore et al 86 have reported a sensitivity and specificity of 100% using MRA; a sensitivity of 93% for CT; 87% using TEE; and 88% using catheter angiography. An additional feature of MRA is accurate diagnosis of aortic regurgitation, which affects prognosis. 85 Intramural hematoma, branch extension, and hemopericardium are also reliably imaged by MRA. The choice between MDCTA and MRA is governed by availability and physician preference and experience with the modality. A large retrospective review showed that most patients with aortic dissection get imaged by at least 2 modalities, 86 this rationale is questionable with the use of MRA.
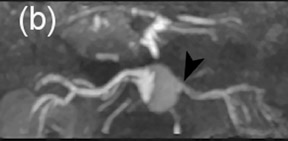
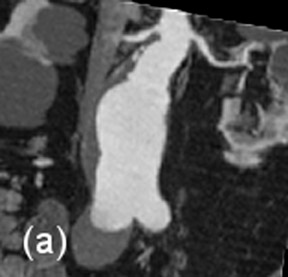
Aortic aneurysms-- Abdominal aortic aneurysm is defined as enlargement of its arterial diameter by >=50% of its normal caliber (>=3 cm in diameter). 87 Abdominal aortic aneurysms are increasingly being treated by the endovascular approach. 88 Criteria for endovascular repair includes the following: 1) infrarenal neck diameter of <3 cm; 2) minimum distance of 1.5 cm between the renal artery origin and the aneurysm; 3) absence of extensive mural thrombus; and 4) if the aneurysm is not too large or does not have a very wide neck. 89 The use of automated volume-rendering software for CTA and MRA has made both modalities equally efficient in preoperative evaluation (Figure 12). 90 Because MRA does not use radiation or nephrotoxic contrast agents, prospective studies have advocated CE-MRA as the sole imaging modality for preoperative planning. 89,91 Engellau et al 92 have reported that measurement of aneurysm length is more accurate on CE-MRAMIP images than by conventional angiography, probably due to inherent magnification in conventional angiographic images.
Imaging is valuable in postprocedure evaluation. It can document proper stent placement, moniter stability of aneurysm size, and diagnose complications like stent migration, stenosis, and endoleaks. The advantage of CTA is its usefulness in the presence of multiple surgical clips adjacent to the aneurysm and when stainless steel stents and stent-grafts have been used, as these would cause significant artifacts on MR imaging. MR imaging with steel stents is contraindicated, 93 though nitinol can be safely imaged.
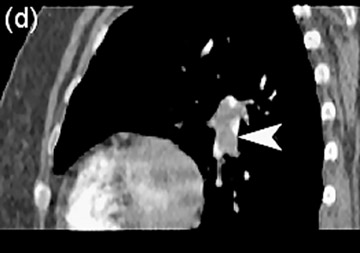
Endoleaks are classified into four types. Type I are small leaks adjacent to the proximal or distal end of the prosthesis. The type II endoleak is reopacification of the aneurysm sac by vessels arising from the lumbar arteries or inferior mesenteric artery. Type III endoleaks are due to fracture of the struts of the graft. Type IV leaks are due to porosity of stent material, and are very rare. In evaluating type I endoleaks, CE-MRA and CTA have equal efficacy. For type II endoleaks CE-MRA has a sensitivity of 94%, as opposed to 50% by CTA (Figure 13). 94 Due to excellent temporal resolution, CE-MRA is suggested to be the procedure of choice in evaluating all type II endoleaks. 93,94 MRA and CTA also help in detecting type III endoleaks.
Renal arteries
Renal artery stenosis (RAS) is the cause of hypertension in 1% to 5% of patients. 95 Atherosclerosis is the most common cause (60% to 70%) and usually affects proximal renal arteries. Patients with atherosclerotic renal artery stenosis often progress to renal failure if untreated. 96 Fibromuscular dysplasia (FMD) is the second most common cause (30% to 40%) of renovascular hypertension with a more diffuse involvement of the vessel.
Imaging is used to detect, grade, and evaluate hemodynamic significance of the stenosis; provide a road map for interventional procedures; and can help assess the functional status of the affected kidney.
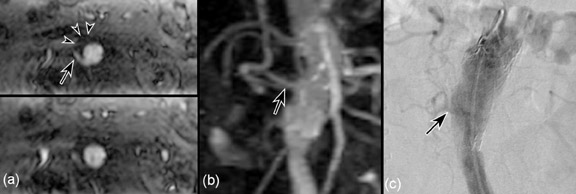
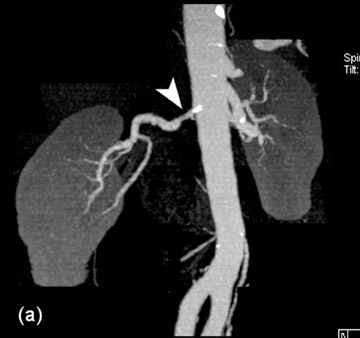
Typical 16-channel MDCT evaluation has a slice thickness of 1 mm with reconstruction at 0.5 mm, providing 500 images in 7 seconds after intravenous administration of 80 mL of iodinated contrast material. 97 The sensitivity and specificity of CTA in the detection of hemodynamically significant RAS in the main renal artery are 100% and 97%, respectively (Figure 14). 98 The advantages of MDCTA include fast imaging, better spatial resolution, depiction of smaller vessels, and better efficacy in detecting RAS due to FMD. It can be easily standardized, does not necessitate a higher level of technical ability, and is less expensive. The disadvantages are in the use of ionizing radiation and iodinated contrast, which may be a limiting factor for its use in patients with compromised renal function. CTA provides limited functional information as compared with MRA, and temporal evaluation using CTA is not possible without increasing the radiation dose.
MRA can serve as a comprehensive examination in assessing RAS as it allows simultaneous assessment of anatomic and functional information. Generally, CE-MRA tends to overestimate the stenosis, 99 though to a much lesser extent as compared with 3D TOF. Additional sequences can be used to avoid this pitfall. Three-dimensional PC MRA detects a signal void to show a significant stenosis, provided an appropriate velocity encoding value is chosen depending on the patient's age and cardiac status. Wasser et al 100 reported equal efficacy of 3D PC MRA and catheter angiography for the detection of hemodynamically significant stenosis, when compared with pressure measurements.
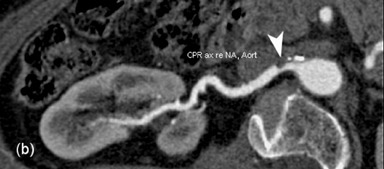
Cine PC technique looks at the temporal pattern of blood flow in a vessel. Velocity measurements are plotted in relation to time. The acquisition is prospectively or retrospectively ECG-gated. Multiple 2D images are obtained at the same location perpendicular to the long axis of the artery. As stenosis develops, changes in vascular resistance alter the shape of the curve correlating with the degree of stenosis. Cardiac-gated PC flow measurements have a sensitivity of 100% and a specificity of 93% for significant stenosis when compared with catheter angiography 101 (Figure 15). A perfusion deficit must be shown to assess the hemodynamic significance of a stenosis. A technique known as extra-slice spin-tagging perfusion-weighted imaging 102 shows asymmetric perfusion of the kidneys in cases of unilateral renal artery stenosis. 103 Examination time and spatial resolution are crucial factors in comparing CTA and MRA. Weiger et al 104 have reported considerable improvement in temporal and/or spatial resolution of MRA when using sensitivity encoding. Gadolinium has been shown to be safe in patients with compromised renal function. 105
Lower extremity arteries
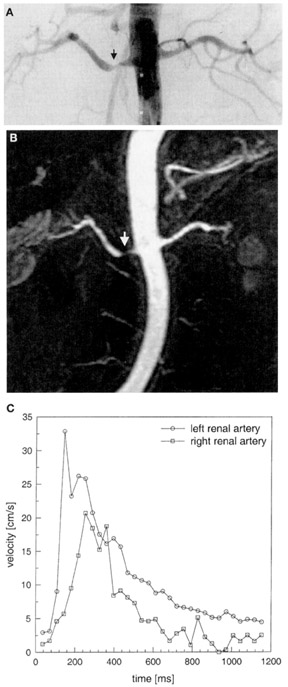
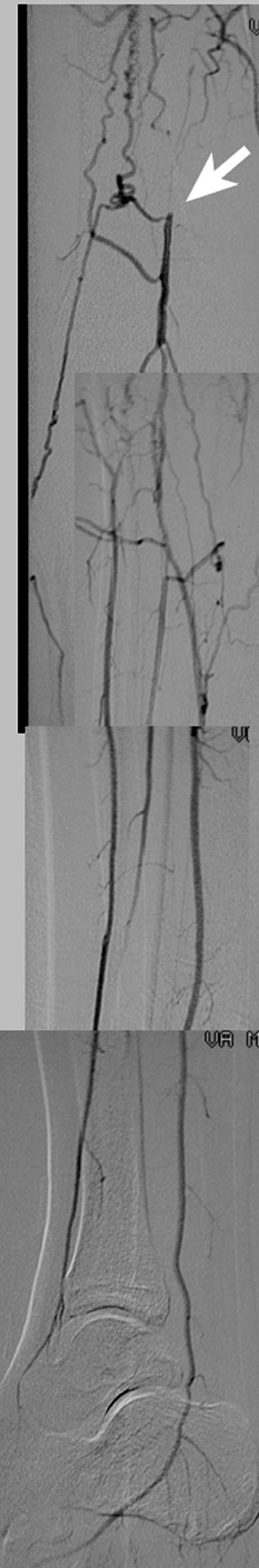
Peripheral vascular occlusive disease (PVOD) is a major health problem, with an annual incidence of 4.5% to 8.0% 106 in men 55 years and older. The role of imaging in PVOD is to establish the diagnosis, provide a preoperative roadmap for the vascular surgeon or the interventionalist, and evaluate the grafts to determine the presence and extent of collateral circulation. An MDCTA is performed with an injection of 120 mL of iodinated contrast at the rate of 4 mL/sec. Anatomic coverage from the celiac artery to the toes is obtained in a single acquisition with a total examination time of 10 minutes. A 3-station (abdominal aorta to toes in 3 acquisitions) bolus-chase CE-MRA is performed with intravenous administration of 40 mL of Gd. Upper and middle stations are acquired coronally, and the last station in either coronal or sagittal planes. 107 Phase encoding is reverse linear, linear, and elliptically centered for each station, respectively.
The sensitivity of MDCTA for the occlusion of femoropopliteal, popliteal, and tibial arteries is 100%, 100%, and 94%, respectively. The specificities are 100%, 99%, and 98%, respectively. 108 For stenosis >75%, the overall sensitivity is reported to be 92.2% with a specificity of 96.8%. 109 Thus MDCTA is a fast, noninvasive, and accurate method for evaluating PVOD. The whole- body radiation dose is 3.9 times reduced as compared with that of digital subtraction angiography, 110 and the contrast requirements are less. The drawbacks of MDCTA include limited function of the MIP software in distal anterior tibial and peroneal vessels, and inadequate imaging of the vessels in the presence of dense mural calcification. MDCTA is thus limited when evaluating for a distal bypass if proximal narrowing is present. 111 A distal bypass done secondary to trauma can be evaluated (Figure 16). The postprocessing of CTA data is time consuming. Up to 45% of patients who have PVOD also have renal artery stenosis 112 and compromised renal function, and a contrast load may precipitate renal failure.
The accuracy of MRA in proximal lower extremities has improved as the technique advanced from 2D TOF to CE-MRA. The specific challenge for CE-MRA is to obtain good spatial resolution at proximal stations, and yet scan fast enough to image the entire lower extremity without significant venous contamination. Cellulitis and osteomyelitis reduce the arterial-venous transit time, leading to venous contamination. 113 CE-MRA can visualize stents adequately; however, it can miss stent stenosis in the absence of secondary signs such as collateral vessels. Time-resolved CE-MRA and parallel imaging have given reduced scan times with subcentimeter spatial resolution. The sensitivity for femoral, popliteal, and anterior tibial vessel occlusion (>70% stenosis) is reported as 96.2%, 96.9%, and 95.5%, respectively. The specificities are 98%, 96.4%, and 91.8%, respectively (Figure 17). 114 Improving spatial resolution, obtaining faster imaging, and avoiding ionizing radiation and nephrotoxic iodinated contrast makes CE-MRA the examination of choice for imaging the distal vasculature.
The future
A prototype four-dimensional (4D) CT with 256 detectors is under development. A 4D image is a 3D image with the additional dimension of time. This CT could allow 0.5 mm true isotropic voxel data to be acquired much faster than the present 16-channel MDCT. MR imaging is rapidly advancing. The future holds clinical imaging at magnet strengths >3T, MR microscopy, complete functional assessment of organ systems, 3D whole-body high resolution imaging with 16-channel phase array coils 115 (multidetector MR), advanced MR-guided interventional procedures, new MRA contrast agents, and use of higher concentration gadolinium.
Related Articles
Citation
Comparison of magnetic resonance angiography and computed tomographic angiography. Appl Radiol.
February 2, 2004