Colocolic intussusception with lipoma as the leading point
Images
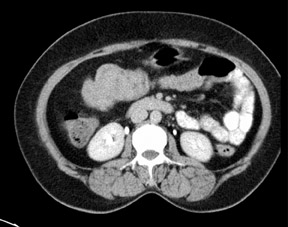


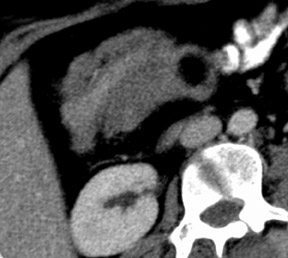


Colocolic intussusception in the hepatic flexure and proximal transverse colon with a 2.5 cm lipoma.
Findings
CT (Figures 1-4) revealed the classic “bowel within bowel” configuration with intervening mesenteric vessels in the region of the proximal transverse colon (right hypochondrium of the patient) over a segment of approximately 8 cm with a 2.5 cm rounded fat density lesion at its apex (Hounsfield unit values of -60 to -130). The intervening bowel layers showed normal wall enhancement. There was no dilatation of the proximal bowel. The solid abdominal organs were normal. There was no ascitis.
Corresponding ultrasound images (Figures 5 and 6) showed the classical pseudokidney appearance of intussusception and a rounded echogenic lipoma at the apex. The bowel was prepared prior to surgery and a supraumbilical laparotomy was performed. The intussusception was reduced and the involved segment at the hepatic flexure was resected. Biopsy of the resected segment revealed a lipoma of the hepatic flexure.
Discussion
Intussusception can be classified according to location or underlying etiology. It occurs either in the small bowel or the colon. The underlying etiology is neoplastic (benign or malignant), non-neoplastic or idiopathic. About 80% to 90% of intussusceptions in adults are secondary to an underlying pathology, with approximately 65% due to benign or malignant neoplasm. Non-neoplastic processes constitute 15% to 25% of cases, while idiopathic or primary intussusceptions account for about 10%. Intussusception arises in the small bowel in two-thirds of cases.1,2
Lipomas are the second most common benign tumors of the colon after adenomas. These tumors are composed of well-defined adipose tissue with a clearly demarcated fibrous support structure. They have a submucous location in 90% of cases. Lipomas can be located anywhere along the digestive tract but they are most common in the colon. Within the colon, 50% are found in the caecum and ascending colon. The occurrence of distal-colon lipoma is rare. Sigmoid lipoma is extremely rare.3
Intussusception can be confidently diagnosed on CT because of its virtually pathognomonic appearance. It appears as a complex soft-tissue mass, consisting of the outer intussuscipiens and the central intussusceptum. There is often an eccentric area of fat density within the mass representing the intussuscepted mesenteric fat, and the mesenteric vessels are often visible within it. A rim of orally administered contrast medium is sometimes seen encircling the intussusceptum, representing coating of the opposing walls of the intussusceptum and the intussuscipiens. The intussusception will appear as a sausage-shaped mass when the CT beam is parallel to its longitudinal axis, but will appear as a “target” mass when the beam is perpendicular to the longitudinal axis of the intussusception. While the appearance of intussusception is characteristic on CT, its etiology cannot usually be established. Exceptions are lipoma, a long intestinal tube and known abdominal metastatic disease. A lipoma serving as a lead point is identified as a mass of fat density that does not contain blood vessels. Mesenteric fat entrapped in an intussusception also has fat density but has blood vessels coursing through it, and can thus be distinguished from lipoma.4
Warshauer and Lee found that intussusceptions seen on CT that had a neoplastic lead point were significantly longer and had a significantly larger diameter than non-neoplastic ones.5 They also found proximal dilatation of the small bowel to be significantly more common in intussusceptions with a neoplastic lead point.
The bowel loops proximal to the intussusception are usually of normal calibre and are occasionally dilated, since intussusception in adults only rarely presents as intestinal obstruction.6 Although intussusception in adults may be diagnosed by many other imaging modalities, including barium enema, upper gastrointestinal series and ultrasound, CT is clearly superior. In contrast to ultrasound, CT is not affected by the presence of gas in the bowel and will clearly demonstrate the intussusception, whether in the small bowel or in the colon. Additional valuable information such as the presence of metastatic disease or lymphadenopathy is readily obtained by CT and may point to an underlying pathology.
Ultrasound imaging of this condition demonstrates several unique appearances: on a transverse section one can see a “doughnut” shape and on a longitiudinal section one can see a “bull’s eye” confirguation, and a pseudokidney finding is also typical.
CT findings also permit a presurgical evaluation of the degree of vascular involvement caused by intussusception. The presence of gas within the intussusceptum suggests perforation or gangrene, indicating the need for an emergency operation.
In this patient, spiral CT showed a lipoma situated in the proximal transverse colon, causing colocolic intussusception. The CT study helped to determine the viability of the intussuscepted loop prior to surgery, thus reducing the extent of surgical treatment and only the tumor was removed. Multiplanar reconstructed spiral CT, allowed examination of the intussusception and lipoma from various angles.
Conclusion
CT is a valuable tool in cases of intussusception due to colonic lipoma. The most important factor for establishing the diagnosis is awareness of the possibility of intussusception occurring in an adult patient with abdominal symptoms, CT is then the examination of choice.
- Agha FP. Intussusception in adults.AJR Am J Roentgenol. 1986;146:527-531.
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94.
- Zeebregts CJ, Geraedts AA, Blaauwgeers JL, Hoitsma HF. Intussusception of the sigmoid colon because of an intramuscular lipoma. Dis Colon Rectum.1995:38:891-892.
- Gayer G, Zissin R, Apter S, et al. Pictorial review: Adult intussusception-A CT diagnosis. Br J Radiol. 2002;75:185-190.
- Warshauer DM, Lee JK. Adult intussusception detected at CT or MR imaging: Clinical imaging correlation. Radiology. 1999;212: 853-860. 6 Gayer G, Apter S, Hofmann C, et al. Intussusception in adults: CT diagnosis. Clin Radiol. 1998;53:53-57.