Radiological case: Bicuspid aortic valve with ascending aortic aneurysm
Images




Prepared by Jarrod Yates, DO, and John Salanitri, MD, FRANZCR, Department of Radiology, Evanston Northwestern Hospital, Evanston, IL.
CASE SUMMARY
A 63-year-old man with known aortic stenosis and increasing fatigue on exercise was evaluated prior to undergoing aortic valve replacement. Echocardiography revealed critical aortic stenosis with a valve area of 0.77 cm 2 , a mean transvalvular gradient of 55 mm Hg, and a peak forward velocity of 4.9 m/sec (not shown). Cardiac catheterization confirmed the presence of severe aortic stenosis and was suggestive of an ascending aortic aneurysm with a diameter of 6 cm (not shown). The left main coronary artery could not be cannulated and was thought to be absent. Mild 3-vessel atherosclerotic coronary artery disease was present. Thoracic aortic computed tomography angiography (CTA) was requested to determine the true aneurysm size prior to operative intervention.
IMAGING FINDINGS
As the patient was in sinus rhythm with a heart rate of 65 bpm, an electrocardiographic (ECG)-gated thoracic aortic CTA was performed on a 64-slice MDCT (LightSpeed VCT 64-slice scanner, GE Healthcare, Waukesha, WI). The entire chest was scanned with 0.625-mm slices in a 9second breath-hold using 90 mL of contrast injected at 5 mL/sec. A single data set was reconstructed in the mid-diastolic phase (75% R-R interval) and was analyzed on an advanced workstation (AWS 4.2, GE Healthcare), with multiplanar reformats, volume rendering, and vessel analysis performed.
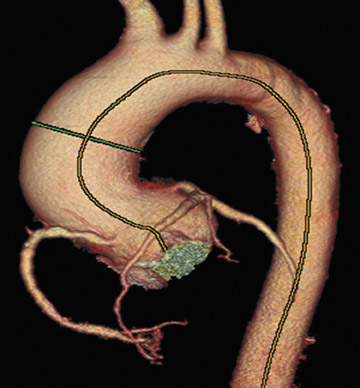
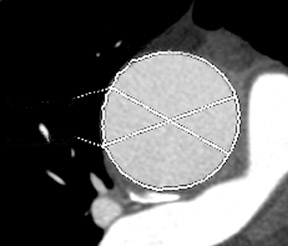
A fusiform aneurysm of the ascending aorta that measured 4.8 cm in maximum diameter was identified with no evidence of dissection, significant mural thrombus, or coarctation (Figure 1). The aortic valve was found to have a bicuspid configuration with heavy calcification of both annulus and cusp margins (Figure 2).
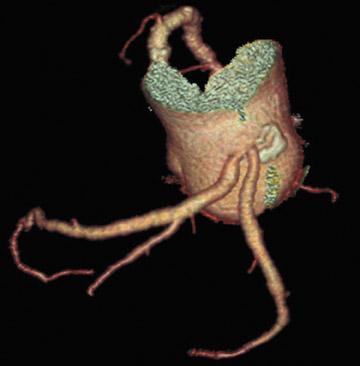
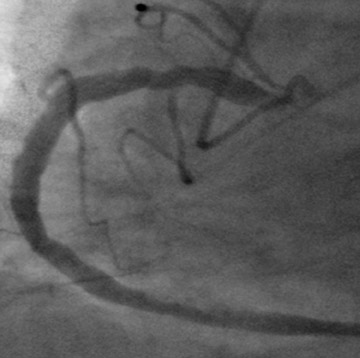
The absence of the left main coronary artery was confirmed along with mild ostial stenoses of both the left anterior descending and left circumflex coronary arteries, which had separate origins from the left sinus of Valsalva (Figure 3A). The right coronary artery was found to have mild mixed-density plaque in its proximal and mid portions with no severe focal stenosis identified (Figure 3B and C).
Subsequent surgery confirmed the bicuspid aortic valve, which was replaced along the ascending aorta. Bypass grafts were placed to the right coronary and left anterior descending arteries. The patient made an uneventful recovery.
DIAGNOSES
Calcific aortic stenosis, bicuspid aortic valve, ascending aortic aneurysm, absent left main coronary artery, and coronary artery atherosclerotic disease
DISCUSSION
Bicuspid aortic valve occurs in 0.5% to 2% of the general population and is the most common cause of congenital aortic stenosis, with degenerative calcification commencing in the fourth decade of life. Bicuspid aortic valves have a male preponderance and may be associated with aortic arch coarctation, atresia, or interruptions as well as hypoplastic heart syndrome. The identification of aortic valve calcifications implies a severe degree of stenosis with a pressure gradient >50 mm Hg. Dilatation of the ascending aorta, which may be aneurysmal (>4 cm diameter), is attributed to jet phenomena caused by the narrowed valve orifice; however, the degree of aortic dilatation does not correlate with the severity of the valvular stenosis. 1 The use of ECG-gated CT can help to determine the valve morphology, accurately measure the valve annulus diameter, and assess the severity of the degree of valve leaflet calcification. 2
Non-ECG-gated helical thoracic CT has long been used to diagnose thoracic aortic pathology including aneurysm, dissection, and coarctation. Pseudodissection artifacts due to aortic motion during the cardiac cycle are well recognized, simulating the appearance of an ascending aortic dissection. 3,4 The use of ECG-gating during image acquisition eliminates this artifact and permits more accurate measurement of the aneurysm and aortic valve annulus diameter, as the images are motion-free. This obviously has important significance for preoperative planning.
The absence of the left main coronary artery with separate ostia for the left anterior descending and left circumflex arteries is an uncommon coronary artery anomaly with an incidence of 0.4% in a series of 20,332 consecutive coronary angiograms. 5 This anomaly is not associated with an increased incidence of congenital heart disease, nor is there an increased incidence of coronary artery disease. Knowledge of this anomaly is important prior to aortic valve replacement, as both vessels may need selective bypass grafting.
In many published series, ECG-gated coronary CTA has been shown to have high sensitivity and specificity for the detection and grading of coronary artery stenoses, particularly in noncalcified vessel segments, with increasing accuracy with more sophisticated multidetector scanners (ie, 16- or 64-slice CT). 6 With the improving temporal resolution of ECG-gated coronary CTA, gated functional analysis of the moving aortic valve leaflets may be possible, in a manner similar to cine magnetic resonance imaging.
CONCLUSION
With the use of high-performance workstation analysis, ECG-gated contrast-enhanced thoracic aortic CTA accurately measured the diameter of the ascending aortic aneurysm secondary to an identified heavily calcified bicuspid aortic valve. The absence of the left main coronary artery was elegantly visualized along with multivessel coronary artery disease, which was not considered to be hemodynamically significant. In the future, ECG-gated CTA may become the first-line investigation required prior to aortic valve replacement, since it provides evaluation of the aortic valve, thoracic aorta, and coronary arteries in a single, minimally invasive examination.
Related Articles
Citation
Radiological case: Bicuspid aortic valve with ascending aortic aneurysm. Appl Radiol.
November 12, 2007