MRI of the foot
Images









Dr. Ali and Dr. Chen are Fellows in Musculoskeletal Radiology, RadNet Management, Los Angeles, CA. Dr. Crues is the Medical Director of RadNet Management, and a Volunteer Clinical Professor of Medicine, University of California-San Diego School of Medicine, San Diego, CA.
In an article published in the August 2006 issue of this journal, the authors reviewed magnetic resonance imaging (MRI) of the ankle. This article will present a review of the use of MRI in the evaluation of the foot, detailing bone and cartilage abnormalities as well as sinus tarsi pathology. The discussion will address the evaluation of the foot in hindfoot, midfoot, and forefoot subsections.
Foot MRI technique
Depending on the clinical question, MRI of the foot should be tailored to a hindfoot, midfoot, or forefoot examination. For hind- and mid-foot, a 12- to 14-cm field of view is applied. For the forefoot, a 10- to 12-cm field of view is used to image the smaller peripheral joints in detail.
Positioning
Similar to the ankle, the foot is placed in a neutral position for high-field-strength scanners and in approximately 30˚plantar flexion for extremity scanners.
Pulse sequences
The pulse sequences for the mid- and forefoot are T1-weighted (T1W) in the coronal and axial planes, short tau inversion recovery (STIR) in the coronal and sagittal or axial planes, and T2-weighted (T2W) in the coronal plane.
For the evaluation of a mass or the diabetic foot, we add T1W sequences before and after intravenous (IV) contrast (gadolinium chelate) administration. On low-field-strength scanners, these are performed without fat saturation; on high-field-strength scanners, fat saturation is applied. Precontrast fat-suppressed images are essential to avoid the pitfall of pseudoenhancement of a mass on fat-saturated postcontrast images when compared with the non- fat-suppressed precontrast images. This is because of a narrow dynamic range of the contrast display on the fat-saturated images when compared with those without fat saturation.
Bone and cartilage abnormalities
Trauma
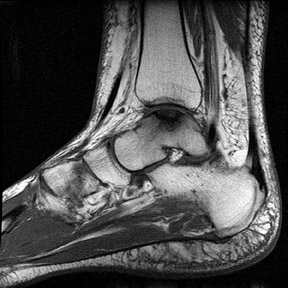
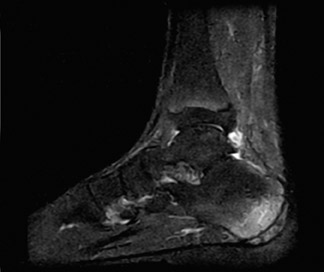
The talus is a relatively common site for osteochondral injury (Figure 1). The middle third (in the sagittal plane) of the lateral border and the posterior third of the medial border of the talar dome are the common locations. 1 In our anecdotal experience, the middle third of the medial talar margin is a more common site than the posterior third. The MRI classification of osteochondral injuries was presented by Hepple et al 2 and stages the talar injuries according to the severity of the injury and the degree of the osteochondral fragment instability. 2,3 Fluid between the osteochondral fragment and the underlying bone, displacement of the fragment, and a fragment size >1 cm are signs of an unstable osteochondral fragment. Unstable or necrotic osteochondral fragments are treated surgically with drilling and curettage. Conservative treatment is preferred when the overlying cartilage is intact and the fragment is stable. 4
Talar neck fractures can lead to avascular necrosis (AVN) of the proximal fragment. Stress fractures can occur in the talus but are less common than calcaneal stress injuries.
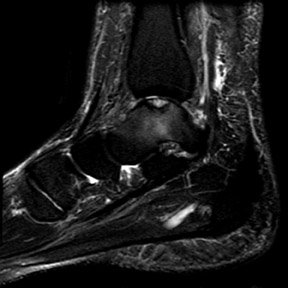
Calcaneus stress fractures can have a diffuse or ill-defined geographic marrow edema pattern (Figure 2). A low-signal fracture line, usually in a vertical orientation, may be visible. Complex calcaneal fractures secondary to a vertical fall mechanism are best evaluated with computed tomography (CT). 4
Congenital
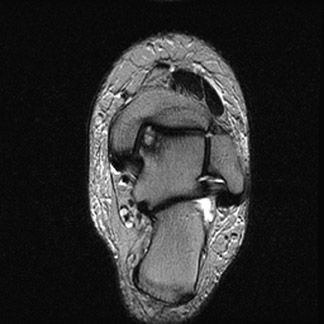
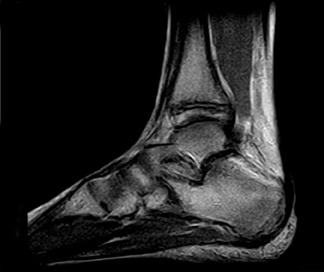
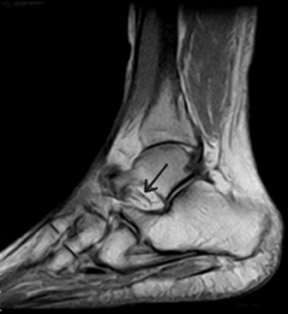
Coalition of the middle talocalcaneal joint is second only to calcaneonavicular coalition. Osseous, fibro-osseous, fibrous, and fibrocartilaginous forms have been described. MRI findings include a direct bony connection or (in the case of nonosseous coalition) irregularity and eburnation of the articulating surfaces and visualization of low-signal fibrous bridging. Medial downsloping of the sustentaculum tali articulating surface (Figure 3) instead of the normal lateral slope and presence of a dorsal talar spur (not to be confused with the physiologic, more proximal dorsal spur at the capsular insertion) are useful ancillary findings. 5,6 Calcaneonavicular coalition (Figure 4) is the most common of the tarsal coalitions. 5,6 As with other sites, it can be osseous or nonosseous. An elongated anterior process of the calcaneus (anteater nose sign) may be present.
Neoplastic
Some of the more common masses in the calcaneus include lipomas, solitary bone cysts, and chondroblastomas. Lipomas have characteristic fat signal. They can have central calcification or cystic focus that appears as signal void or fluid signal, respectively (Figure 5). Bone cysts in calcaneus are more common in the older age group (>20 years). They have fluid signal and are located in the calcaneus body more inferiorly as compared with the chondroblastomas. Chondroblastomas are more common in men in their second or third decade. They occur in a subarticular location and have high signal on T2W images and low signal on T1W images because of their cartilaginous nature. Low-signal foci of chondroid calcifications and linear low- signal septations may be present.
Miscellaneous pathology
Navicular osteochondrosis (Köhler's disease) is seen in younger patients (3 to 7 years of age). Fragmentation and low signal on T1W and T2W images are seen. 7 It must not be confused with the fragmented appearance of nonunited ossification centers. In adults, AVN secondary to trauma can occur (Muller-Weiss disease). 8 There is collapse and low signal of the bone on all pulse sequences. Bony changes seen with subtalar instability and inflammatory arthropathies are discussed with sinus tarsi pathology.
Sinus tarsi pathology
The sinus tarsi contain 3 ligaments extending from the talus to the calcaneus. The lateral-most is the continuation of the inferior extensor retinaculum. The cervical ligament has a striated appearance. It extends from the talar neck to the body of the calcaneus in an oblique anteroposterior direction, providing stability to the subtalar joint. The interosseous ligament is the most medial of the 3. It extends from the talus to the calcaneus in an oblique mediolateral direction (Figure 6). The ligaments limit the inversion of the hindfoot and play an important role in maintaining the stability of the subtalar joint. The sinus tarsi is predominantly filled with fat and also contains blood vessels and nerve endings. 9,10
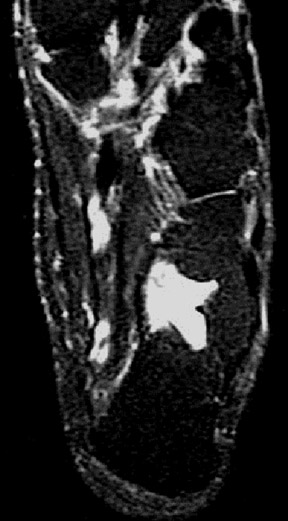
The ligaments can be torn secondary to acute trauma or more commonly by chronic recurrent microtrauma. This can lead to subtalar instability with resulting degenerative changes in the joint. Articular surface irregularity and subchondral sclerosis with or without subchondral edema can be seen. Posterior talocalcaneal facet is involved to a greater degree. Normal fat signal in the sinus tarsi is replaced with edema or fluid signal. There is associated nonvisualization of the torn sinus tarsi ligaments (Figure 7).
Ankle, subtalar, and tarsal joints can be affected by inflammatory arthropathies (Figure 7), such as Reiter's disease, or crystal deposition disease, such as gout. MRI can reveal inflamed synovium in addition to the bony erosions and edema. Masses, such as ganglion cysts and lipomas, can occur and lead to pain from compression of nerve endings. 9,10
Hindfoot pathology
Plantar fasciitis is most pronounced within 2 to 3 cm of the calcaneal attachment. It manifests as a smooth thickening (>4 mm) of the plantar fascia, with adjacent subcutaneous edema. Edema may also be seen in the calcaneus at the insertion site of the plantar fascia (Figure 8). It is associated with a plantar calcaneal spur in approximately 50% of cases.
Tears of the plantar fascia occur most commonly in the midportion of the fascia. This is more distal to the typical location of plantar fasciitis (Figure 9). They can be partial or complete. Trauma is the usual etiology. Discontinuity and waviness of the fascial cords with adjacent soft tissue edema are seen on the MRI. 11
Plantar fibromatosis is nodular fibrous proliferation of the plantar fascia. The appearance can vary from a well-circumscribed low-signal lesion on all pulse sequences to a locally invasive lesion with ill-defined borders and intermediate signal (Figure 10). This is a difficult lesion to treat because of its tendency to recur following local resection. 11-13 Differential diagnoses include soft tissue masses (such as giant cell tumor) and sarcomatous neoplasm (such as synovial sarcoma and fibrosarcoma). A well-circumscribed appearance and homogenous low-signal characteristics suggest fibromatosis. 14-16
Osseous abnormalities of the hindfoot were discussed earlier.
Midfoot pathology
Trauma
A traumatic tear of the Lisfranc ligament (a short bandlike ligament that extends from the plantar anterolateral corner of the medial cuneiform to the plantar posteromedial corner of the base of the second metatarsal) is an important injury (Figure 11). 17 It can lead to instability and progressive disorganization of the Lisfranc joint. Additionally, there can be loss of the medial longitudinal arch. The rupture of the ligament fibers is more common than is the avulsion fracture at the bony attachments. 17-19 It is an important diagnosis, since early internal fixation may give the ligament a chance to heal and can help to avoid the need for future arthrodesis. Even with early intervention, the success rate is <50%.
The tarsal bones are a common site of trabecular stress injury. Marrow edema with a lack of a clear fracture line is present.
The flexor hallucis longus (FHL) tendon is prone to tendinosis and tears at the knot of Henry. The mechanism is chronic repetitive friction with the flexor digitorum longus (FDL) tendon from activities like jogging. 20 This is analogous to the intersection syndrome between the first and second extensor compartment tendons in the wrist. The medial plantar nerve branches can get entrapped between the knot of Henry and the abductor hallucis muscle, leading to first and second toe plantar dysesthesias.
Neoplastic
Synovial sarcoma is a malignant neoplasm with predilection for the foot. It is predominantly seen in patients between the ages of 15 and 40 years. It is an aggressive neoplasm with a posttreatment 5-year survival rate of approximately 55%. 21,22 Local recurrence and pulmonary and bone metastasis are common. On MRI, it appears as a well-defined mass with a heterogeneous low signal on T1W images. On T2W images, it has a heterogeneous high signal (Figure 12). Cystic areas are common. Fluid-fluid levels can be present in close to 20% of cases. Foci of calcifications can lead to areas of low signal on T2W images. Heterogeneous enhancement is seen with IV contrast ad-ministration. It usually displaces the adjacent structures rather than invading them. Sometimes a small size, slow growth, and well-circumscribed appearance can lead to an erroneous diagnosis of a benign mass. 23 Other soft tissue neoplasm, benign and malignant primary bony neoplasm, and, less commonly, metastasis can all involve the midfoot.
Arthropathy
The Lisfranc and Chopart (intertarsal) joints are commonly disrupted in neuropathic arthropathy (Charcot joint). Rapid destruction of the joints and bones is the rule if protective measures are not taken early in the process. Therefore, early detection of neuropathic changes is very important. Signs on MRI include tear of the Lisfranc ligament and edema in the tarsal and metatarsal bones adjacent to the joints. Loss of normal bony relationship and articular and osseous destruction are advanced findings (Figure 13). 24-26
A common clinical question is the differentiation between osteomyelitis and a neuropathic joint. Certain findings (such as the presence of more focal involvement of the bones, skin ulcers, sinus tracts, and abscess) are more suggestive of infection (Figure 14). In early neuropathic joint, the signal abnormalities are centered on the joint. However, a clear distinction between infection and neuropathic changes is not always possible with imaging.
The midfoot is often involved in arthropathies such as gout and rheumatoid arthritis. The findings on MRI include erosions, bone marrow edema, and synovitis. In the absence of a correlative history, these can be confused with osteomyelitis. Degenerative changes in the midfoot can be seen with altered mechanics or can be posttraumatic.
Forefoot pathology
Trauma
"Turf toe" refers to a capsuloligamentous injury of the metatarsophalangeal (MTP) joint of the first toe. The mechanism of injury includes anterior thrust of the metatarsal head in a hyperextended joint with a relatively fixed great toe. This is common in sports played on synthetic turf, like football, hence the name turf toe. There is stretching and tearing of the plantar capsule and tearing of the plantar plate. The plantar plate is a fibrocartilaginous structure that extends from the metatarsal neck to the base of the proximal phalanx. It reinforces the plantar capsule and also attaches the hallux sesamoid bones to the base of the proximal phalanx (Figure 15). Discontinuity of the plantar plate and focal edema and fluid is seen. Associated proximal displacement of the hallux sesamoids may be seen. 27,28
Collateral ligament tears are also more common in the great toe. Varus or valgus force is the usual etiology. Edema and discontinuity of the medial or lateral collateral ligaments is present (Figure 16). The MTP collateral ligament tear is more common than that of the interphalangeal joints. 29
Hallux sesamoids can be involved with fractures, AVN, and sesamoiditis secondary to inflammatory arthropathies or osteomyelitis. The medial sesamoid is more commonly involved with trauma, and lateral sesamoid tends to get AVN. Replacement of the normal marrow fat signal with edema signal can be seen. Freiberg's infraction of the metatarsal heads is characterized by fissuring, osteonecrosis, and eventual collapse of the subchondral bone (Figure 17). The second and third metatarsal heads are most commonly affected. 27 Repetitive microtrauma and vascular compromise are the most popular theories of the etiology. It is more common in young women and may be secondary to the wearing of high heels. In its acute stage, there is a marrow edema pattern. In its chronic phase, there is deformity of the metatarsal head and associated degenerative arthritis.
"March fracture" is a stress fracture of the metatarsal neck. 27 The name comes from its common occurrence in military recruits. It is predominantly seen with activities that place excessive stress on the metatarsals, such as ballet dancing and gymnastics. Marrow edema and adjacent soft tissue edema are seen in early stages. Periosteal thickening is present in the subacute stage as a healing response.
Neoplastic
Pressure lesions are fibrofatty lesions that occur in the subcutaneous fat. These typically develop at the load-bearing bony prominences, including the plantar aspects of the first and fifth metatarsal heads or below the calcaneal tuberosity. These lesions are of low signal on T1W images and of variable signal (intermediate-to-high signal) on T2W images. They can have fat in the interstices. Sometimes they can develop central cystic changes. They generally lack the well-defined morphology of a mass, and their appearance is that of an ill-defined fibrotic tissue (Figure 18). The characteristic location and interspersed fat in the lesion favor the diagnosis and help differentiate it from a neoplasm. 24
Morton neuroma is a focal perineural fibrosis of the plantar interdigital nerves. It is not a true neuroma. The most common location is the third and fourth web spaces between the plantar aspects of the metatarsal heads. 30-32 It is more common in women, and, once again, the wearing of high heels is implicated as a causative factor. Other etiologic possibilities include the compression of the nerves by the intermetatarsal ligament or a distended intermetatarsal bursa. Pain in the web space with or without radiation to the toes is the usual presenting symptom. These are small lesions that are nearly isointense to the muscles on T1W images, are intermediate to high in signal on T2W images, and can be isointense to fat (Figure 19). Fat-suppressed IV contrast-enhanced T1W images give the highest lesion conspicuity because of intense lesion enhancement. It can be a mobile lesion and can change positions in the intermetatarsal space. 32
A giant cell tumor of the tendon sheath is a relatively common benign lesion. It is a focal form of extra-articular pigmented villonodular synovitis. It is low in signal on T1W images and is low-to-intermediate signal on T2W images (Figure 20).
Other masses, such as foreign body granulomas, ganglion cysts, and malignant neoplasms (like synovial sarcomas or metastasis) can all occur in the forefoot location.
Arthropathy
The MTP joint of the great toe is the characteristic location for gout. Monoarticular involvement is common but not the rule. Gouty tophi cause characteristic erosions with punched-out, overhanging edges of the periarticular bones. They also occur at extra-articular locations with associated osseous erosions. Tophi have low signal intensity on T1W images and low-to-intermediate signal intensity on T2W images (Figure 21). 33 Variable enhancement is seen with IV contrast administration. Septic arthritis should always be considered in the differential diagnosis of monoarthritis. Rheumatoid arthritis and Reiter's disease are other common arthropathies in the forefoot. Osteoarthritis commonly involves the first MTP joint as well.
Conclusion
MRI is the imaging modality of choice for evaluation of musculoskeletal pathology, including the soft tissue and osseous trauma, neoplasms, and inflammatory pathology. Compared with CT, MR provides a superior contrast resolution and exquisite detail of soft tissue structures. It also surpasses CT in the evaluation of trabecular bone injury. The strengths of MRI in evaluating various foot pathologies have been briefly reviewed in this article.