MRI in acute spinal trauma
Images










Dr. Hollingshead
is a Neuroradiology Fellow and
Dr. Castillo
is a Professor, Department of Radiology, University of North
Carolina, Chapel Hill, NC.
Some of this article was originally presented as an electronic
exhibit at RSNA 2006: Hollingshead MC, Castellano F, Pulnik J,
Castillo M. MRI of ligamentous and soft tissue injury in the
cervical spine. Electronic exhibit at the RSNA 92nd Scientific
Assembly and Annual Meeting, November 2006; Chicago, IL.
Magnetic resonance imaging (MRI) allows the radiologist to directly evaluate all of the soft tissues of the spine, including the ligaments, cord, disks, and vasculature. Thus, it can be crucial in the evaluation of the trauma patient with ligamentous injury and possible instability. While radiographs and computed tomography (CT) may suggest soft tissue injury, MRI allows for direct visualization and confirmation. This article will review the use of MRI in acute spinal trauma. Recognition of soft tissue injuries helps guide patient management and surgery, results in changes in management, and influences prognosis.
Protocols
At our institution, patients with significant trauma undergo evaluation of the cervical spine with screening CT using reconstructed 2-mm axial images (acquired at 0.6 mm) with coronal and sagittal reformations. MRI is obtained in patients whose CT scans show a potentially unstable injury, obtunded patients who cannot localize symptoms, and those with neurologic symptoms. Our protocol includes sagittal T1-weighted (T1W), T2-weighted (T2W), and short-tau inversion-recovery (STIR) sequences (3 mm thick), as well as an axial T2*-weighted (T2*W) sequence (3 mm thick) without contrast. For the evaluation of thoracic or lumbar spinal trauma, an evaluation begins with plain films. CT imaging consists of 2-mm axial reconstructed images with coronal and sagittal reformations, often all obtained from the raw data acquired during an evaluation of the thorax and/or abdomen. Our MRI protocol includes sagittal T1W, T2W, and STIR sequences (4 mm thick), as well as axial T1W, T2W, and T2*W sequences (4 mm thick) without contrast.
Normal ligaments and identification of injury
MRI allows direct visualization of some of the ligaments that support the craniocervical junction. Ligaments are generally linear, low-signal-intensity structures. The anterior atlantoaxial membrane extends from the axis, C2, to the atlas, C1. 1 The anterior atlanto-occipital membrane extends from C1 to the clivus. 1 The apical dental ligament extends from the superior tip of the dens to the clivus. 2 Posteriorly, the tectorial membrane originates on C2 and extends to the clivus. Deep to the tectorial membrane is the transverse ligament, which inserts on the internal surface of the lateral masses of C1. The alar ligaments are also deep to the tectorial membrane.
The major subaxial ligaments include the anterior and posterior longitudinal ligaments and the posterior ligamentous complex (PLC). The anterior longitudinal ligament (ALL) is a low-signal, linear structure along the anterior portion of the vertebral body cortex and disks. The ALL adheres to the midportion of the vertebral body and blends with the annulus over the disks. 3 The posterior longitudinal ligament (PLL) is a low-signal, linear structure along the posterior portion of the vertebral body and the disks. It is best seen on T2W images because of adjacent bright cerebrospinal fluid of the spinal canal. 3 The PLC, which includes the interspinous ligaments, ligamentum flavum, and facet joint capsular ligaments, is not as well defined on MRI as the ALL or PLL. 4,5
An advantage of MRI is its ability to accurately identify a ligamentous injury. 4,6,7 An area of discontinuity indicates a disruption (Figure 1). However, the ligament can also be "stripped" away from its underlying structure, which is indicated by separation from those structures. This is exhibited as increased T2 and STIR signal deep to the ligament. "Thinning" or "stretching" of the ligament may indicate injury as well (Figure 2). Because the PLC is not as well defined as other ligaments, one can identify injury as increased T2 or STIR signal within the complex (Figure 3). 3
Ligamentous injury and instability
The definition of spinal instability remains controversial. Broadly speaking, an injury should be considered unstable when there is the possibility of further skeletal or neurologic injury without stabilization. 6,8-10 The clinician needs to identify unstable injuries in order to perform appropriate, timely intervention. 6,8-10 MRI can contribute by directly visualizing injured ligaments. However, because of a lack of large studies with surgical or pathological correlation, it is not known to what degree MRI may overestimate the degree of damage. 11
Traditionally, in the subaxial cervical spine, one can attempt to identify unstable injuries by using specific measurements on plain films. Daffner et al 9 described 5 radiographic signs that are suggestive of instability: displacement of a vertebral body by 2 mm, widening between the spinal laminae by 2 mm, abnormalities involving the facets, injury involving the posterior portion of the vertebral body, and an increased interpediculate width of 2 mm.
Denis developed the "3-column model of the spine" for evaluation for thoracolumbar spine instability. 8,12 The anterior column of the spine consists of the ALL and anterior two thirds of the disks and vertebral bodies. The middle column includes the PLL and posterior one third of the disks and vertebral bodies. The posterior column includes everything dorsal to the middle column. Instability is indicated by injury to the middle column and one other column. This model has also been applied to the subaxial cervical spine.
"Clearance" of the cervical spine
The role of MRI in the "clearance" of the cervical spine, particularly in obtunded patients, continues to be debated. 13-15 The goal is to identify an isolated ligamentous injury of the cervical spine that is not suspected on plain film or CT. Chiu et al 16 evaluated 14,577 patients who experienced blunt trauma. There was an overall incidence of ligamentous injury without evidence of fracture of 0.6%. Of the "unreliable patients," a total of 14 of 2605 patients (0.5%) had a ligamentous injury without associated fracture. MRI was not used in this study.
Studies have shown that cervical spine CT may be effective in excluding significant ligamentous injuries. Hogan et al 14 examined 366 obtunded trauma patients. CT had a negative predictive value for ligamentous injury of 98.9% and a negative predictive value of 100% for unstable injuries. Schuster et al 15 reported their experience with 12 obtunded patients who could move all 4 extremities and had a negative CT. Cervical spine MRI was negative in all of these patients. However, another study examined 150 patients admitted to the intensive care unit after blunt trauma. Of 108 patients with normal radiographs, MRI showed an extradural soft tissue injury or ligamentous injury in 27. 17
In a recent comprehensive review, Ackland et al 13 evaluated the literature on this topic, including some of the studies above. They suggest that MRI should be used in screening obtunded patients who are at high risk of cervical spine injury but temper that recommendation with a comment on the lack of and need for prospective studies. 13
Spinal cord injury
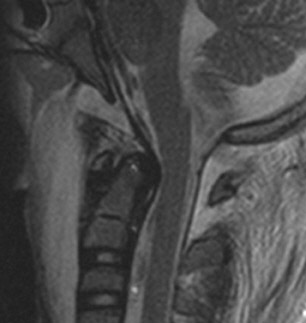
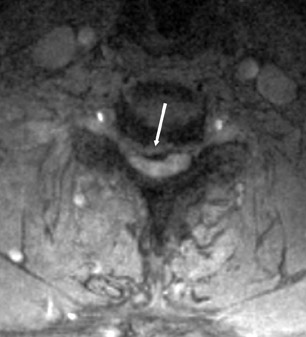
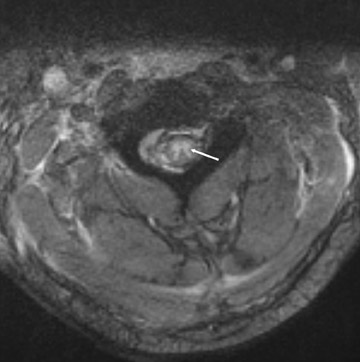
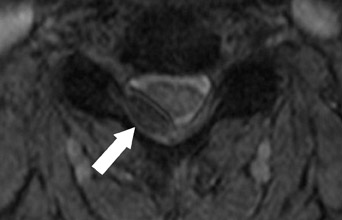
MRI allows the evaluation of the spinal cord. The cord may be directly damaged by a traumatic event or by impingement because of an associated injury, such as a herniated disk (Figures 4 and 5). 18 MRI can identify the level of cord injury and the associated soft tissue injuries. Because of this, it can assist in operative planning.
Injury to the cord is revealed by the presence of high T2 signal, which indicates edema or contusion, as well as by signal changes that are indicative of hemorrhage or cord infarct (Figures 6 and 7). The presence of intramedullary hemorrhage and longer segments of edema are more often associated with complete spinal cord injuries and a worse prognosis. 18,19 In 1999, Shepard et al 20 found that MR results did not add much in terms of prognostic implications when compared with clinical predictors, but confirmed that the presence of hemorrhage was associated with a worse prognosis. An earlier study had concluded that MRI complemented and improved the ability to predict outcome after spinal cord injury. 19
Spinal cord injury without radiographic abnormality (SCIWORA) has been seen in approximately 34.8% of pediatric patients with spinal cord injury, though the reported incidence varies widely. 21 These patients have persistent neurologic complaints despite negative radiographs or CT. 21 Until about age 9, a child's spine is hyper-mobile when compared with the adult spine, which allows for cord damage at the time of injury without residual radiographic evidence. 21 MRI allows visualization of the cord injury and can aid in predicting outcome. 21
Vertebral artery injury
Vertebral artery injury is associated with cervical spine injury, particularly when the trauma is severe. 22,23 Although angiography remains the gold standard, evaluation with magnetic resonance angiography (MRA) has been advocated as a noninvasive study. 22-25 In a study of 319 patients with significant cervical spine trauma (including 261 fractures, 24 bilateral facet dislocations, 22 unilateral facet dislocation, and 12 cases of SCIWORA), 52 patients had a vertebral artery injury diagnosed by MRA. 24 In another study, 83 of 632 patients with fracture, dislocation, or neurologic symptoms related to a cervical cord injury had an acute vertebral artery injury identified with MRA. 22 One study identified 4 cases of vertebral artery injury in 12 patients with a fracture involving the foramen transversarium. 25 Types of injuries associated with vertebral artery injury are fracture-dislocations, fractures of the foramen transversarium, interfacetal dislocations, and injuries involving sites of exit and entry of the vertebral artery into the foramen transversarium in the upper and lower portions of the cervical spine (Figure 8). 22-25
Vertebral artery injuries may be diagnosed on initial routine sequences, but additional MRA sequences can be performed for further or initial evaluation. In particular, an axial T1W sequence is useful for evaluating dissection. 23 While patients may present with posterior circulation symptoms, most patients are asymptomatic. The risk of stroke is increased with bilateral injury. 25
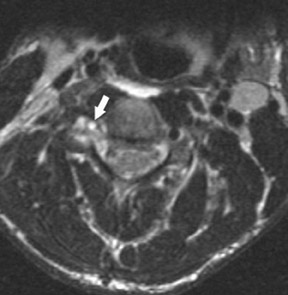
Extramedullary hemorrhage
Extramedullary hemorrhage can be identified with MRI (Figure 9). Posttraumatic epidural hematomas, which are thought to be venous in origin, most often involve the cervical or thoracic spine. 26,27 Usually, they are dorsal to the thecal sac, as the PLL is firmly adherent to the dura anteriorly. 26,27 Subdural hematomas are most often ventral to the cord. 26 These collections can be clinically significant if there is cord compression. 26,27 MRI can provide an early diagnosis, which would lead to prompt treatment; however, depending on the signal characteristics of the hemorrhage, a diagnosis can sometimes be difficult (Figure 10). 26,27
Specific types of cervical spine injury
Discussion of injuries to the cervical spine can be divided into the craniocervical junction and the subaxial cervical spine. Atlantooccipital dislocation can be obvious on plain film or CT, but dissociation can be more difficult to identify (Figure 2). 1 The mechanism of injury involves distraction and may involve flexion or extension. 12 These injuries are severe and unstable; the diagnosis must be made immediately. 28 Though most often fatal, patients now survive more frequently. 29 This may be because of more rapid emergency response, improved life-support measures at the scene, and earlier diagnosis because of improvements in imaging. 29 Identification of atlanto-occipital dislocation can be difficult in children because of their lack of complete ossification, but MRI can reveal the ligamentous injuries directly. 2 Signs of brain- stem injury should alert the clinician to consider the diagnosis. 28,29
A similar mechanism of injury leads to atlantoaxial distraction. (Figure 7) MRI can show injuries that involve the articular capsules, tectorial membrane, and other atlantoaxial ligaments. 2
Injuries of the subaxial spine are classified based on the mechanism of injury. Hyperextension injuries usually involve either a rear impact motor vehicle collision or a direct blow to the face. 30 Usually, the lower cervical spine is involved. 31 These injuries can be ligamentous rather than osseous and can be difficult to diagnose on plain films. 30 The prevertebral soft tissues and ALL are initially injured with progression of injury posteriorly, with increasing severity leading to dislocation. 30-33 Disk injuries include avulsion from the endplate or herniation. 30 With more severe injury, particularly in patients with hyperextension dislocation, cord injury may manifest as central cord syndrome (Figure 1). 30,32,34 This involves weakness of the upper limbs greater than the lower limbs in conjunction with bladder dysfunction and sensory deficits. 30,33,34 In two thirds of patients, an avulsion fragment, longer in transverse dimension, is identified along the anterior-inferior vertebral body. 33
Flexion injuries of the cervical spine range from mild strains to fracture dislocation injuries. The posterior ligaments are usually injured (Figure 3). Bilateral interfacetal dislocation is due to an extensive injury to the musculature and ligaments from flexion and distraction (Figure 11). 5 The anterior and middle columns are usually involved. 3 While the PLL was traditionally thought to be completely disrupted, Carrino et al 35 reported that the PLL was intact in 60% (18 of 30) of patients with bilateral interfacetal dislocation. However, they acknowledge that despite the fibers being visibly intact on MRI, the ligaments are most likely injured and thinned as well as mechanically weakened, possibly because of partial tears from stretching. 35 These injuries are unstable and surgery is required, but the urgency and approach are based on the degree of neurological injury and associated factors such as disk herniation. 36 Unilateral interfacetal dislocation involves flexion, rotation, and distraction. 5
Progressive flexion forces can cause a large fracture of the anterior portion of the cervical vertebral body with retropulsion of the posterior portion of the vertebral body into the spinal canal leading to the "flexion teardrop injury" (Figure 5). 37 The radiographic appearance can be deceptive, as only the fracture may be recognized. 37 However, this is an unstable injury with a high incidence of spinal cord injury. Surgical intervention is required, but the best approach is controversial. 37
Thoracolumbar trauma
The thoracic spine is stabilized by the ribs, leading to less frequent injury unless the trauma is severe. 38 The lower thoracic and lumbar spine is more mobile, which leads to an increased risk of injury. 38 Types of thoracolumbar injury include wedge compression, burst, fracture dislocation, and flexion-distraction (Figure 6). 38 MRI allows visualization of the associated ligamentous and spinal cord injuries.
Vaccaro et al 39 have recently developed a new classification system for thoracolumbar injuries. The classification is based on 3 components: radiographic appearance of injury, status of the PLC, and neurologic symptoms. 39 Many factors are involved in surgical planning, but the status of the PLC and neurologic symptoms are key. 39 Since MRI provides information regarding the status of the soft tissues, it is useful in operative planning and in identifying stability via this classification. The morphologic types of injury include compression, translational/rotational, and distraction. A grading system is applied to determine the severity of the injury. 39
One type of flexion-distraction injury in the thoracolumbar spine is the Chance fracture. Classically, there is a horizontal fracture involving the pedicles that may extend into the vertebral body, but variants of this injury can be purely ligamentous, involving only the facets and disk. 40 Burst fractures can have a similar appearance on plain film, but MRI allows for the examination of the posterior column and PLC to appropriately diagnose the injury (Figure 12). 40
Conclusion
MRI allows the radiologist to directly evaluate the soft tissues of the spine and is, therefore, crucial in the evaluation of the patient with ligamentous injury and, thus, instability. Recognition of soft tissue injuries impacts patient management and outcome.