Metastatic Castrate-Resistant Prostate Cancer (mCRPC)
Images

By: R. Jeffrey Karnes, MD, FACS; Mohamed E. Ahmed, MBBCh
Brought to you by Telix.
CASE SUMMARY
A 69-year-old man presented with a persistent rising prostate specific antigen (PSA) of 15.8 ng/mL in September 2019. The patient’s previous PSA readings were 11.4 ng/mL in November 2018 and 12.9 ng/mL in May 2019.
The patient had a known history of prostate cancer and was treated initially with Radical Retropubic Prostatectomy (RRP) for Gleason 3 + 4 = 7. The patient subsequently experienced biochemical recurrences and was treated with salvage external beam radiation therapy, intermittent hormone therapy with leuprolide, and 3 cycles of Provenge.
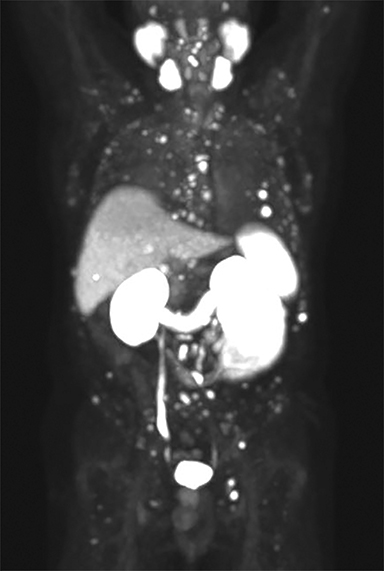
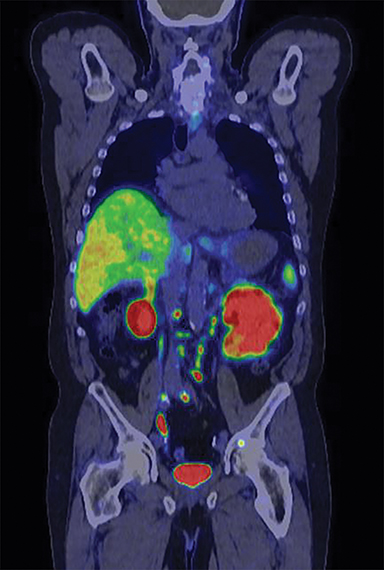
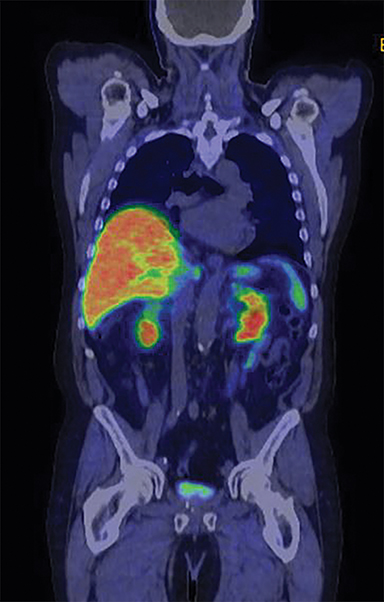
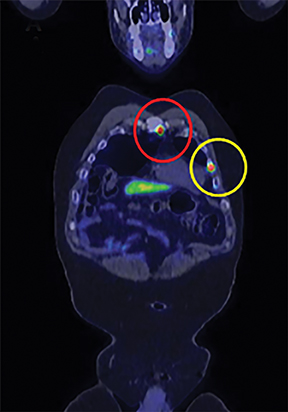
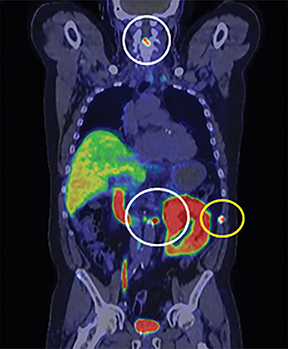
In early 2017, the patient developed castrate-resistant prostate cancer and was started on abiraterone with prednisone. In November 2018, the patient experienced disease relapse in the iliac bones bilaterally on his choline PET/CT scan with a PSA of 11.4 ng/mL After detailed discussion of his treatment options, the patient opted to change to enzalutamide. In May 2019, the patient underwent repeat evaluation with C-11 choline PET/CT scan and MRI abdomen and pelvis; both imaging showed no dramatic lesions that have been identified associated with the current state of prostate cancer on this individual. As such, the patient was offered to undergo extensive radiographic evaluation with PSMA-PET scan, C-11 choline PET scan and MRI abdomen and pelvis on his subsequent follow-up visit. Surprisingly, while MRI and choline PET scan once again revealed very little evidence of metastatic recurrence of prostate cancer, PSMA PET scan showed innumerable intense PSMA positive metastases throughout the axial and appendicular skeleton (Figure 1). Subsequently, the patient underwent treatment with 6 cycles of docetaxel plus carboplatin, to which he responded very favorably. In June 2020, the patient’s PSA decreased markedly to 3.4 ng/mL with only 2 or 3 skeletal lesions on his PSMA-PET scan.
IMAGING FINDINGS
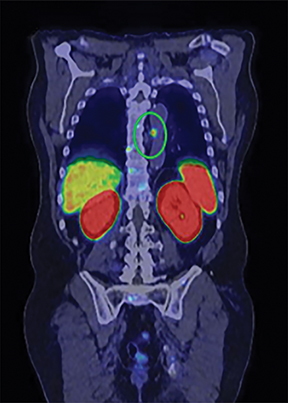
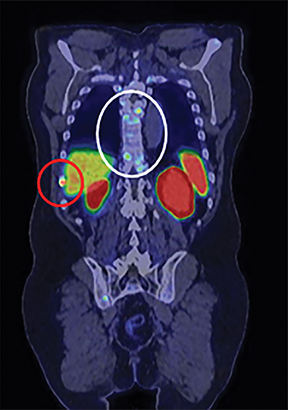
The patient underwent Ga 68 PSMA PET/CT scan with CT fusion imaging for attenuation correction and anatomic co-registration only, with imaging beginning approximately 60 minutes after radiotracer injection. Ga 68 PSMA PET/CT scan revealed innumerable PSMA-avid metastatic lesions throughout the axial and appendicular skeleton, including the sternum, ribs, and spine (Figure 2). There were also multiple tiny, bilateral common iliac and retroperitoneal lymph nodes concerning for metastatic disease. Additionally, there was a solitary aortoesophageal PSMA-avid lymph node. Notably, there was no definitive evidence of PSMA-avid locally recurrent disease within the prostatectomy bed.
DIAGNOSIS
Metastatic Castrate-Resistant Prostate Cancer (mCRPC)
DISCUSSION
Despite advances in treatment and management, prostate cancer is the second-most common cause of cancer deaths in men, ranking only behind lung cancer. Approximately 192,000 new prostate cancer cases, and nearly 33,000 deaths are expected in 2020.1 While primary prostate cancer has an indolent nature, most patients will eventually develop castration-resistant prostate cancer, which accounts for the majority of prostate cancer deaths.2 In contrast to restaging of primary localized disease, restaging of mCRPC requires more advanced radiographic evaluation C-11 choline PET/CT, and/or PSMA PET/CT. Mitchell et al reported better sensitivity to disease relapse after primary treatment in patients with low PSA level with C-11 choline PET/CT scan than with conventional imaging, with an optimum PSA level of ≥ 2.0 ng/mL. Additionally, current reports suggest better sensitivity with PSMA PET/CT with the ability to detect disease relapse at very low levels of PSA at 0.2 – 0.5 ng/mL3
We noted in our case, however, a clear discrepancy between both scans despite a high PSA level of 15.8 ng/ml. This could be explained in part by the patient’s extensive history of systemic treatment, including Provenge and novel androgen receptor inhibitors. It has been reported that treatment with novel androgen receptor inhibitors could result in a treatment-induced lineage crisis and cellular plasticity.4
Beltran et al described treatment-induced neuroendocrine disease in mCRPC patients undergoing treatment with abiraterone.5 Therefore, patients with advanced mCRPC may require meticulous evaluation with the multi-imaging modality to detect disease relapse and receive individualized treatment plans based on location of their disease relapse.
CONCLUSION
Ga 68 PSMA PET/CT scan constitutes the most advanced imaging modality for prostate cancer among all currently available scans, even in cases of extremely low PSA levels (0.2ng/mL). The use of Ga 68 PSMA PET/CT scanning to evaluate CRPC patients would constitute an invaluable advance in prostate cancer diagnosis and management.
REFERENCES
- Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2020; 70: 7-30. doi:10.3322/caac.21590
- Denmeade SR, Isaacs, JT. A history of prostate cancer treatment. Nat Rev Cancer. 2002; 2: 389-396. doi:10.1038/nrc801
- Pfister D, Bolla, M, Briganti A, Carroll P, Cozzarini C, et al. Early salvage radiotherapy following radical prostatectomy. Eur Urol. 2014: 65: 1034-1043. doi:10.1016/j.eururo.2013.08.013
- Davies, AH, Beltran H, Zoubeidi A. Cellular plasticity and the neuroendocrine phenotype in prostate cancer. Nat Rev Urol. 2018; 15: 271-286. doi:10.1038/nrurol.2018.22
- Beltran H, Tagawa ST, Park K, MacDonald T, Milowsky MI. Challenges in recognizing treatment-related neuroendocrine prostate cancer. J Clin Oncol. 2012; 30: e386-389. doi:10.1200/jco.2011.41.5166
Related Articles
Citation
Metastatic Castrate-Resistant Prostate Cancer (mCRPC). Appl Radiol.
January 19, 2021