Localized Prostate Cancer Recurrence
Images
By: R. Jeffrey Karnes, MD, FACS; Mohamed E. Ahmed, MBBCh
Brought to you by Telix.
CASE SUMMARY
A 70-year-old man presented with persistent rising prostate specific antigen (PSA) of 3.2ng/mL in July 2020. The patient was post retropubic radical prostatectomy (RRP) for Gleason 3+4=7 in 2006. Subsequently, the patient experienced biochemical recurrences for which he received salvage external beam radiation therapy to the prostate bed in 2007, cryotherapy to the vesicourethral anastomosis in 2015, and external beam radiation therapy to the pelvic lymph nodes in 2016, followed by hormone therapy for approximately one year. In February 2019, the patient’s PSA level started to rise to detectable levels at 0.45ng/mL, reaching 1.1ng/mL in July 2019.
A PET/MR scan revealed increased uptake in a perirectal lymph node. In September 2019, the patient underwent MRI-guided cryoablation of this perirectal lymph node. Interestingly, despite treatment, the PSA continued to rise to 2.3 ng/mL in March 2020, and to 3.2 ng/mL in July 2020.
The patient underwent evaluation with MRI of the abdomen and pelvis, C-11 choline PET/CT scan, and Ga-68 PSMA PET/CT scan.
IMAGING FINDINGS
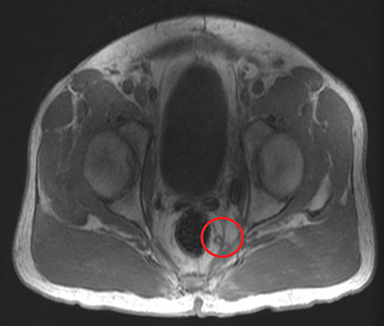
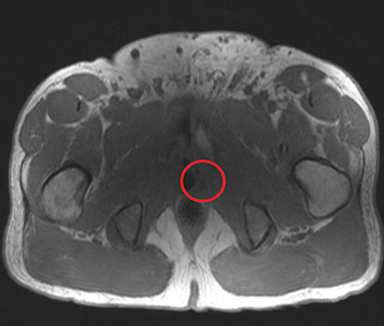
MRI of the abdomen and pelvis revealed a post-ablation defect in the left posterolateral aspect of the vesicourethral anastomosis. However, there was prominent increased signal that could not exclude recurrent tumor in this region. In addition, there was increased activity around the ablated left perirectal lymph node. There were multiple tiny lymph nodes worrisome for nodal metastases within the perirectal and presacral regions. Additionally, there was a 3-mm right internal iliac chain lymph node also worrisome for metastatic involvement.
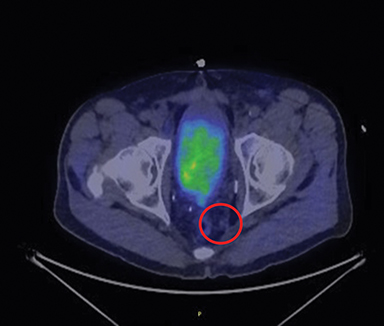
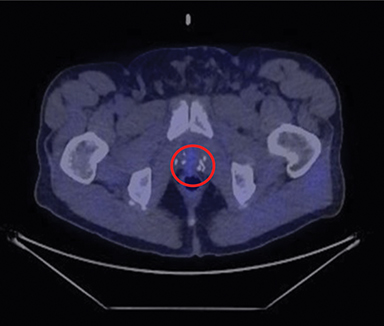
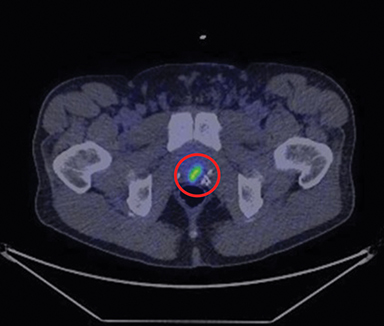
C-11 choline PET/CT scan revealed a left presacral soft tissue nodule with trace choline uptake. There was no definite choline uptake above background activity along the vesicourethral anastomosis; however, the area was partially obscured by physiologic activity of urine. There was no other choline-avid lymphadenopathy or osseous or visceral metastases.
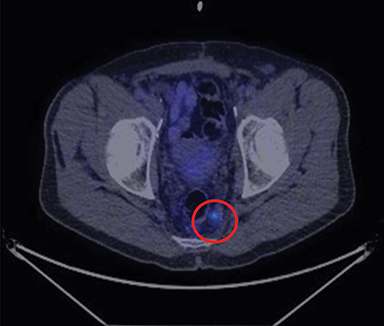
Ga-68 PSMA PET/CT scan, in comparison, revealed multiple small posterior and left lateral perirectal tracer-avid lymph nodes or soft tissue nodules. There was also another tracer-avid anterior right perirectal soft tissue nodule or lymph node abutting the posterior aspect of the bladder just to the right of midline. In addition, there was intense tracer uptake at the vesicourethral anastomosis as well as minimal tracer activity in a right internal iliac lymph node. There were no tracer-avid bone lesions.
Of interest, both the MRI and C-11 choline PET/CT scan were suspicious for local recurrence as well as perirectal nodal recurrence, however, these lesions were very obvious on Ga-68 PSMA PET/CT scan.
DIAGNOSIS
Localized prostate cancer recurrence
FOLLOW-UP
The patient re-initiated treatment with Lupron hormone therapy of three months’ duration. The patient responded very well to the treatment and the PSA decreased rapidly to undetectable levels <0.10ng/mL in one month.
DISCUSSION
Prostate cancer accounts for nearly 33,000 deaths annually, representing the second-most common cause of cancer death among men, ranking only behind lung cancer.1 While primary prostate cancer can be managed with radical prostatectomy or radiation therapy, 40% of patients will experience disease relapse.2 Recurrent prostate cancer requires personalized management that depends on the location of disease relapse. In 2013, the US Food and Drug Administration approved C-11 choline PET/CT scanning for detecting prostate cancer relapse after primary treatment failure, with an optimum PSA level of ≥ 2.0ng/mL.3 Despite the higher sensitivity of the C-11 choline PET/CT scan to disease recurrence compared with conventional imaging, Ga-68 PSMA PET/CT has demonstrated significantly higher sensitivity than C-11 choline PET/CT. In a systematic review and meta-analysis, Eyben et al reported that Ga-68 PSMA PET/CT was able to detect the location of disease relapse after primary radical prostatectomy in half of patients with PSA levels between 0.5 and 1 ng/mL, and in up to 75% of patients with PSA >1 ng/mL.4,5 Some recent reports suggest that Ga-68 PSMA PET/CT can detect disease recurrence at PSA levels <0.5 ng/mL.6,7
This report demonstrates the significant difference in sensitivity between MRI abdomen/pelvis, C-11 choline PET/CT, and Ga-68 PSMA PET/CT in detecting prostate cancer relapse. The higher sensitivity of Ga-68 PSMA PET/CT allows it to detect disease relapse at very small volumes of <8 mm.8 Despite the fact that Ga-68 PSMA PET/CT is not yet approved by the FDA for this indication, Afaq et al reported that PSMA PET/CT has a significant impact on disease management, with overall changes in 39-76% of cases.8 The high performance of PSMA PET/CT represents the future of prostate cancer diagnosis and management.
CONCLUSION
This report confirms the important clinical consideration of the high sensitivity of Ga-68 PSMA PET/CT in determining disease recurrence after initial treatment failure, particularly in patients with very low PSA levels.
REFERENCES
- Siegel RL, Miller KD, Jemal A. Cancer Statistics 2020. CA Cancer J Clin. 2020; 70: 7-30. doi:10.3322/caac.21590
- Mullins JK, Feng Z, Trock BJ, Epstein JI, Walsh PC, Loeb S. The impact of anatomical radical retropubic prostatectomy on cancer control: the 30-year anniversary. J Urol. 2012; 188: 2219-2224. doi:10.1016/j.juro.2012.08.028
- Mitchell CR, Lowe VJ, Rangel LJ, Hung JC, Kwon ED, et al. Operational characteristics of (11)c-choline positron emission tomography/computerized tomography for prostate cancer with biochemical recurrence after initial treatment. J Urol 2013: 189: 1308-1313. doi:10.1016/j.juro.2012.10.069
- von Eyben FE, Picchio M, von Eyben R, Rhee H, Bauman G. (68)Ga-Labeled Prostate-specific Membrane Antigen Ligand Positron Emission Tomography/Computed Tomography for Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol Focus. 2018; 4: 686-693. doi:10.1016/j.euf.2016.11.002
- von Eyben FE, Baumann GS, Baum RP. PSMA diagnostics and treatments of prostate cancer become mature. Clin Transl Imaging. 2018; 6:145-148. doi:10.1007/s40336-018-0270-2
- Eissa A, Elsherbiny A, Coelho RF, Rassweiler J, Davis JW, et al. The role of 68Ga-PSMA PET/CT scan in biochemical recurrence after primary treatment for prostate cancer: a systematic review of the literature. Minerva Urol Nefrol. 2018; 70: 462-478. doi:10.23736/s0393-2249.18.03081-3
- Pfister D, Bolla M, Briganti A, Carroll P, Cozzarini C, et al. Early salvage radiotherapy following radical prostatectomy. Eur Urol. 2014; 65: 1034-1043. doi:10.1016/j.eururo.2013.08.013
- Afaq A, Bomanji J. Prostate-specific membrane antigen positron emission tomography in the management of recurrent prostate cancer. Br Med Bull. 2018; 128: 37-48. doi:10.1093/bmb/ldy032
Related Articles
Citation
RJ K, ME A.Localized Prostate Cancer Recurrence. Appl Radiol. 2021; (2):32-33.
March 11, 2021