Imaging of cystic liver lesions in the adult
Images






Dr. Power is a Consultant Radiologist and Dr. Bent is Specialist Registrar in Radiology, Department of Medical Imaging, Royal London Hospital, Whitechapel, London UK. Dr. Chan is a Consultant Radiologist, London Independent Hospital, London UK.
This material in this article was presented in educational exhibit form at the Radiological Society of North America Meeting, December 2004.
Cystic liver lesions in adults can have a number of etiologies, including congenital, neoplastic, and infectious conditions, as well as trauma and miscellaneous entities. While most such cystic lesions are benign and are frequently clinically irrelevant, the radiologist must be able to recognize key imaging features to enable the diagnosis of the more clinically important lesions. Features to assess include lesion size, the presence and thickness of a wall or any internal septations or mural nodules, the presence of either internal or mural calcification, and the pattern of enhancement following intravenous contrast. The importance of the clinical history in these patients cannot be overstated.
Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can act in a complementary fashion to optimize lesion characterization. Ultrasound can reveal internal septations, mural nodules, and debris in a lesion. CT can show wall or septal calcification, while the signal characteristics of the cyst content on MRI may define its contents, for example, if it is hemorrhagic. MRI is the best imaging modality for detecting wall enhancement. Knowledge of the imaging features of the most common types of cystic liver lesions should enable an accurate diagnosis to be made and should potentially avoid the need for cyst aspiration or needle biopsy.
Congenital cystic lesions
Simple cysts
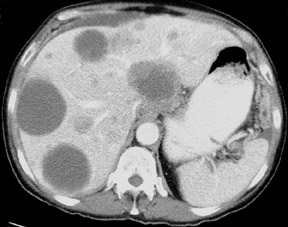
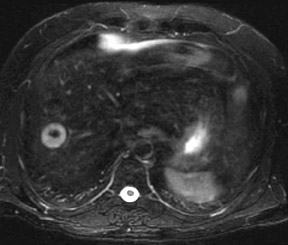
Simple cysts are the most common type of cystic liver lesion and are seen in approximately 2.5% of the population 1 ; they are developmental, arising from a defect in bile duct formation. On ultrasound, they are anechoic with posterior acoustic enhancement, while on CT they are of fluid attenuation (Figure 1). On MRI, they are of homogenously low signal intensity (SI) on T1-weighted (T1W) imaging and high SI on T2-weighted (T2W) imaging. An increase in the echo time (TE) will cause an increase in the SI on T2W MRI, which is useful in discriminating cysts from metastatic deposits. There is no discernible wall and no discernable enhancement following the administration of either iodinated contrast or gadolinium. Rim calcification is rare but may occur. Possible complications include infection, rupture, torsion, hemorrhage, and malignant transformation. But these complications are all rare, especially the latter, though adenocarcinoma developing in a simple cyst has been reported. 2 Complications may alter the imaging appearances; eg, intracyst hemorrhage can cause increased SI on T1W MRI as well as possible wall thickening and the development of fluid-fluid levels. 3 Infection may give rise to intracyst debris and septations, which are best seen with ultrasound. 4 Cysts may be solitary or multiple, though if >10 cysts are present, the possibility of polycystic liver disease should be considered. 5
Autosomal dominant polycystic liver disease
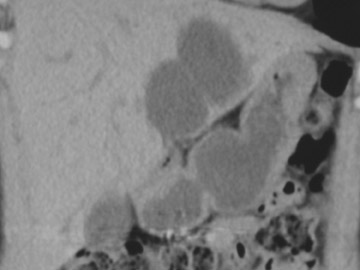
Autosomal dominant polycystic liver disease is part of the spectrum of fibro-polycystic liver diseases that are caused by congenital bile duct malformation, including bile duct hamartoma, Caroli's disease, congenital hepatic fibrosis, and choledochal cyst. 6 It is frequently seen in association with adult polycystic kidney disease (Figure 2), although it can occur in the absence of renal cysts. The cysts are identical-both radiologically and histologically-to simple cysts. 4 Multiple cysts can cause painful hepatomegaly, a frequent presenting complaint. Possible complications are identical to those of simple cysts but are more frequent. 1 The existence of any correlation between the severity of cystic disease in the liver with renal cystic disease is controversial. 4,7
Bile duct hamartoma
Also known as von Meyenburg complexes, bile duct hamartomas arise from ductal plate malformations that involve the small interlobular bile ducts. 6 They are seen in up to 3% of autopsy specimens 8,9 though in only 0.7% of CT studies; 10 44% of bile duct hamartomas are thought to be occult on CT. 8 They typically are small lesions that range from 2 to 15 mm in diameter; the larger lesions may, in fact, constitute an aggregation of smaller lesions. 10 They are generally scattered throughout the liver, are of uniform size, and are rounded or oval. While there is some variability in their imaging appearances, they are typically anechoic on ultrasound and of fluid density on CT, low SI on T1W MRI and high SI on T2W MRI. 8,9,11 Their enhancement following contrast administration is variable; no enhancement, rim enhancement, and slow homogenous enhancement have all been reported. 8,9 The differential diagnosis for multiple small cystic liver lesions includes simple cysts, microabscesses, granulomata, and metastatic disease. The small and uniform size is unusual in simple cysts and metastasis, while clinical correlation is obviously essential to discriminate hamartomata from other imaging possibilities. Imaging features are ultimately nonspecific, and needle aspiration may be required in some cases.
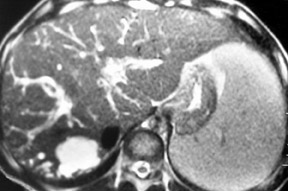
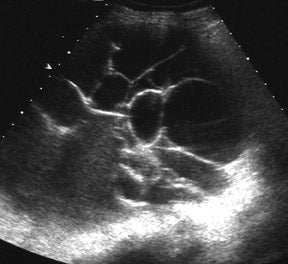
Caroli's disease
Caroli's disease is an autosomal recessive disorder, also known as congenital cavernous ectasia of the biliary tree. It can be segmental or diffuse and can cause marked saccular dilatation of the affected bile ducts (Figure 3). Two forms have been described: the pure form, which is associated with attacks of cholangitis and intraductal stone formation; and the complex form, which is more common and is associated with other ductal plate malformations. 4,6 Affected ducts are markedly dilated and contain bile and sludge, and, occasionally, stones and pus. The ducts often have a beaded appearance with strictured and dilated segments alternating. Ultrasound and CT may show beaded dilated ducts, but it can be difficult to visualize the communication of the cystic structures to the biliary tree. Endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC) can be diagnostic by showing that the dilated ducts opacify with contrast, but these are invasive procedures and are not without risk. MRCP has shown promise as a noninvasive imaging modality for the diagnosis of this entity. 12 A hallmark of this condition on both CT and MRI is the presence of the "central-dot sign," which is a fibrovascular bundle lying centrally within the dilated duct that contains a portal vein radical that enhances with contrast. 1,6 Complications include stone formation, cholangitis, and liver abscesses; there is also an increased risk of developing a cholangiocarcinoma. 6 The differential diagnosis includes primary sclerosing cholangitis and recurrent pyogenic cholangitis, though both of these conditions usually cause stricturing and dilatation of both the intra-and extrahepatic biliary tree, in contrast to Caroli's disease, which affects only intrahepatic ducts. 6
Neoplastic cystic lesions
Undifferentiated embryonal sarcoma
This is a rare malignant tumor that is usually seen in teenagers and that frequently manifests as a large, solitary, predominantly cystic mass. The cystic appearance relates to the high water content of the myxoid stroma. 13 It is usually a multiseptate lesion with a variable, predominantly peripheral solid component. The multiseptate nature may be better appreciated on ultrasound and MRI than on CT. MRI generally shows a focal mass with multiple cystic spaces, septations, and central necrosis. 14 Following contrast administration, there may be heterogenous enhancement of the solid components of the tumor. As with all cystic lesions, intralesional hemorrhage will alter the signal characteristics, typically increasing the SI on T1W imaging. While this is a rare tumor, the diagnosis should be borne in mind when a teenage patient presents with a large, solitary cystic mass.
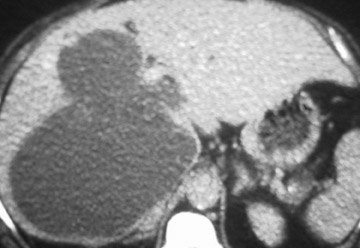
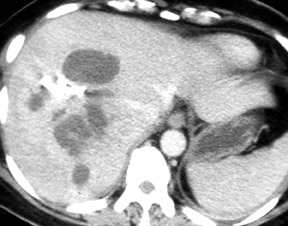
Biliary cystadenoma and adenocarcinoma
These are rare, slow-growing, multilocular cystic tumors derived from biliary epithelium, although they generally do not communicate with the biliary system. 5 The subepithelial stroma may be similar to ovarian or be of mesenchymal histology. 4,15 Histological types include mucinous (the commonest type), serous, and papillary. They are most frequent in middle-aged women and on ultrasound are seen as a multiloculated cyst. CT usually reveals a solitary, well-defined cystic lesion with a thick, fibrous capsule; mural nodules, internal septations, and, occasionally, capsular calcification may also be seen (Figure 4). MRI may also show nodules and septations, which are more commonly seen in the adenocarcinoma variety. However, neither radiology nor cytology of cyst fluid is reliable enough to discriminate adenoma from adenocarcinoma; thus, if this diagnosis is suspected, surgical resection is essential. 16 The prognosis is good if the tumor is completely resected, but recurrence is frequent if resection is incomplete.
Cystic subtypes of liver neoplasia
The most common primary liver tumors with cystic subtypes are hepatocellular carcinoma (HCC) and giant cavernous hemangioma. At imaging, HCC may appear cystic either because of necrosis or the effects of local treatment, such as radiofrequency ablation. Roughly 70% of patients with HCC have underlying cirrhosis, 4 although presentation as a multicystic mass in a non-cirrhotic liver has been reported. 17 Nonetheless, this diagnosis should be considered when a cirrhotic patient presents with a partially cystic mass. Vascular invasion is also typical of this condition. Giant cavernous hemangioma may rarely become cystic if it outgrows its blood supply. However, the typical appearance of peripheral nodular enhancement following contrast administration may well be preserved and should suggest the diagnosis. Rare tumors reported to have presented with a partially cystic mass at imaging include adenosarcoma 18 and adenoma. 19
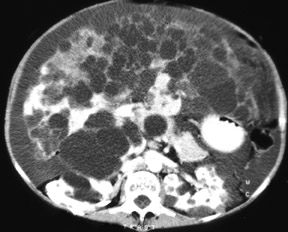
Cystic liver metastases
The liver is second only to lymph nodes as a site of metastatic disease, and liver metastases are 20 times more common than primary liver tumors. 4 Metastases in the liver may be cystic for a variety of reasons. Metastases that become necrotic will appear cystic at imaging, which is most commonly seen in hypervascular metastases--for example, from a neuroendocrine tumor or sarcoma. 20 Mucinous primary tumors such as colorectal or ovarian tumors frequently give rise to cystic metastases (Figure 5). In the case of a cystic ovarian primary tumor, metastases have been reported to evolve into cystic lesions, even if they were initially solid. 21 Also, metastases may undergo cystic change with response to treatment, which has been reported in the case of metastases from a testicular teratoma 22 and a gastrointestinal stromal tumor. 23 On imaging, cystic liver metastases may show variable wall thickness, and, on MRI, enhancement and fluid-fluid levels may be seen. 4 Their imaging appearance will vary depending on the primary tumor and the stage of treatment.
Infective cystic lesions
Liver abscess
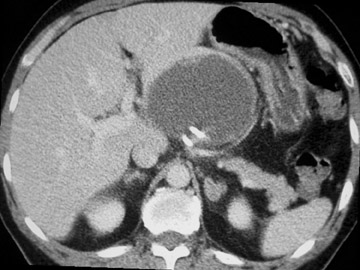
Organisms may reach the liver either from the biliary tree (ie, secondary to ascending cholangitis), hematogenously, or because of superinfection of necrotic tissue. The most common subtypes of liver abscess are pyogenic and amoebic. Organisms causing pyogenic abscess include clostridium and gram-negative bacteria, such as Escherichia coli . Ultrasound, CT, and MRI are all >90% sensitive for the presence of a liver abscess, 24 although there is great variability in imaging appearances depending on the stage of infection. For this reason, imageguided aspiration, with or without drain placement for treatment, may be necessary to make the diagnosis. A pyogenic abscess may initially manifest as a cluster of small abscesses that coalesce into a large abscess cavity. Ultrasound may show a variable appearance that ranges from echogenic to anechoic 5 (Figure 6), while CT generally shows a uni- or multilocular cystic lesion that may be associated with a thick enhancing wall and perilesional edema 24 (Figure 7). Gas within a cystic lesion is characteristic for an abscess. MRI appearances are also variable, though wall enhancement and perilesional edema are typical. Prompt diagnosis and treatment of this condition have reduced mortality from 40% to approximately 2%. 24
Amoebic abscess has an imaging appearance that is similar to that of a pyogenic abscess; however, it is generally seen in younger patients and there may be a helpful travel history. If this diagnosis is suspected, serology may be positive, and if confirmed, percutaneous drainage is generally not necessary, as the abscess responds well to antiamoebic therapy. 4
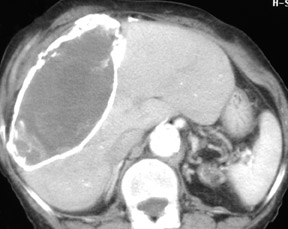
Hydatid cysts
A hydatid cyst is caused by an infection with the eggs of the echinococcus species of tapeworm; E granulosus is the more common type, with E multilocularis causing the infection alveolar echinococcosis.
E granulosus eggs reach the liver via the portal vein and give rise to a 3-layer hydatid cyst. The outer layer is the pericyst, which consists of compressed liver; inside this is the endocyst, a germinal layer; and inside this is the ectocyst, a thin membrane. The imaging appearances depend on the degree of cyst maturation. Initially, a simple cyst is seen that may have an enhancing rim on CT and MRI; the pericyst is typically low signal on T2W MRI. 24,25 A simple cyst on ultrasound may contain multiple mobile echogenic foci (hydatid sand), which enables differentiation from a congenital simple cyst. Subsequent to this, the classical imaging appearance of daughter cysts within the mother cyst caused by endocyst invagination may develop, giving rise to a wheel-spoke or rosette appearance. Daughter cysts are typically of lower SI relative to the high SI cyst matrix on T2W MRI. Peripheral calcification may be seen in up to 50% of cysts on CT 1 (Figures 8 and 9). If the cyst is entirely calcified, it is usually dead. Cysts may be complicated by rupture (in 50% to 90% of cases) that can communicate with the biliary tree or directly into the pleural or peritoneal cavity, and superinfection may follow cyst rupture. The typical-and quite specific-imaging appearance of E multilocularis infection is multiple small cysts with echogenic nodules on ultrasound and a solid mass with numerous small (<1 cm) cysts on CT and MRI. 24,26
Miscellaneous cystic lesions
Intrahepatic pseudocyst
Rarely, pancreatitis may cause the development of a pseudocyst in the liver, usually in the left lobe. This diagnosis is suggested by both the patient's medical history and the imaging features of pancreatitis. MRI is the optimal imaging modality to distinguish pseudocyst contents such as hemorrhage and debris, although intralesional hemorrhage may cause an increase in the attenuation on CT. These fluid collections usually become better defined with time 1,4 (Figure 10).
Hematoma
A hematoma in the liver may be due to surgery, trauma, or a bleed from a liver lesion. In cases caused by surgery or trauma, the diagnosis should readily be suggested by the clinical history. The most common liver lesions that bleed spontaneously are an HCC and an adenoma. 13 Areas of focal nodular hyperplasia, metastases, or hemangiomata very rarely bleed. As with hemorrhage anywhere in the body, the imaging appearances vary depending on the chronicity. For example, a subacute hematoma may have increased SI on T1W MRI because of the paramagnetic effects of methemoglobin. After approximately 10 days, a hematoma is usually of fluid attenuation and has the imaging appearance of a cystic lesion.
Biloma
Biloma occurs because of rupture of the biliary system, which may be caused by either surgery or trauma or may occur spontaneously. It may be intra- or perihepatic and is generally seen near the porta hepatis or gallbladder fossa. Bile causes an intense inflammatory response that leads to the development of a pseudo-capsule. Imaging shows a cystic lesion that may contain debris but rarely has septations or calcification 1,4 (Figure 11). The diagnosis may be suggested by the clinical history. Cholescintigraphy may confirm communication of the fluid collection with the biliary tree. The liver-specific contrast agent mangafodipir trisodium (Teslascan, GE Healthcare, Princeton, NJ) is excreted via the biliary system and T1W MRI after injection of this agent may be useful in the diagnosis of a bile leak. 27
Conclusion
There are many causes of cystic liver lesions with a huge variability of clinical significance attached to them. Awareness of the clinical history is always useful in narrowing the differential diagnosis. However, given the regularity with which these lesions are encountered in everyday practice and their often nonspecific clinical presentations, it is also essential for radiologists to be armed with knowledge of the key imaging features of the more important lesions. Avoiding the need for aspiration or biopsy, if at all possible, must be a primary goal for the radiologist.
Related Articles
Citation
Imaging of cystic liver lesions in the adult. Appl Radiol.
May 1, 2007