Current status of MRI in patients with inflammatory bowel disease colitis
Images






Dr. Geenen is a Radiologist, Medisch Centrum Alkmaar, Alkmaar, The Netherlands. Dr. Hussain is a Professor of Radiology, University of Nebraksa Medical Center, Omaha, NE. At the time this article was written, Drs. Geenen and Hussain were affiliated with Erasmus MC-University Medical Center. Dr. Poley, Dr. Siersema, and Dr. Kuipers are Gastroenterologists, and Dr. Kuipers is a Professor of Gastroenterology, Department of Gastroenterology & Hepatology, Erasmus MC. Dr. Krestin is a Radiologist, a Professor of Radiology, and Chairman of the Department of Radiology, Erasmus MC-University Medical Center Rotterdam, Rotterdam, The Netherlands. Portions of this article were previously presented in: Geenen RWF, Hussain SM, Poley JW, et al. Combined bright and black lumen MR. Colonography in patients with inflammatory bowel disease (IBD). Preliminary results. Presented at The Scientific Assembly and Annual Meeting of the Radiological Society of North America; November 28, 2004; Chicago, IL.
Inflammatory bowel disease (IBD) is characterized by an inappropriate and ongoing activation of the bowel mucosal immune system in the presence of a normal bacterial flora. 1 The current general view is that IBD manifests itself under certain environmental conditions on a genetic basis. 2 The etiology and pathophysiology of IBD consist of 4 interacting factors: genetic, environmental, microbial, and immune. 1,3,4 It includes 2 distinct diseases: ulcerative colitis (UC) and Crohn's disease (CD). 1 In 10% of patients with IBD that is limited to the colon, it is initially not possible to distinguish UC from CD; this is the so-called indeterminate colitis (IC). 1
With their high incidence and prevalence, both UC and CD are huge healthcare problems in the Western world. Extrapolation of reported incidence and prevalence rates of UC in North America show that 7000 to 46,000 new cases of UC are diagnosed annually and that approximately 780,000 people have UC. 5 Extrapolation of European incidence and prevalence figures for UC produces estimates of 50,000 to 68,000 new cases of UC annually and approximately 1 million UC patients. 5,6 Extrapolation of epidemiological figures for CD show that 10,000 to 47,000 residents of the United States and Canada are diagnosed with CD each year and that approximately 630,000 have CD. 5 Extrapolation of European data gives incidence rates of 23,000 to 41,000 annually and prevalence rates of 850,000, 5,6 with up to 25% of the UC and CD cases manifesting in childhood. 7 The median age of CD diagnosis is reported to be 29.5 years. 5 Generally, UC is diagnosed 5 to 10 years later than is CD. 5
Ulcerative colitis is a chronic inflammatory process that is limited to the colorectal mucosa. 4 The rectal mucosa is invariably affected, and inflammation and superficial ulceration extend proximally from the anal margin. Depending on the extension of the disease process, a patient may have proctitis, left-sided colitis (extension into the descending colon), extensive colitis (involvement of the transverse colon), and/or pancolitis. 8 Pathologically, the disease process is continuous and the cutoff between colitis and normal mucosa is sharp. 9 In 15% to 20% of patients with severe UC, a so-called backwash ileitis develops, which almost always resolves after total colectomy. 10 Data on UC suggest that this disease results from environmental factors that trigger a breakdown of the mucosal immune response regulation to enteric bacteria in genetically susceptible individuals. 4
Crohn's disease is characterized by transmural inflammation that can affect any part of the gastrointestinal tract with relapses and remissions throughout its course. 3 Data suggest that intestinal inflammation arises from abnormal immune reactivity to bacterial flora in the intestine of genetically susceptible individuals. 3 The colon and ileum are the most involved parts of the gastrointestinal tract in two thirds of CD patients. Involvement of other parts of the digestive tract does occur but is uncommon. 1 Three patterns of isolated colonic CD are found: CD isolated to the rectum, stricturing CD, and diffuse Crohn's colitis. 9 Pathologically, CD is a discontinuous patchy or focal process. Ulcers vary from superficial aphtoid ulcers to deep fissuring ulcers, which can give rise to fistulae or abscesses. Strictures can occur at sites of transmural inflammation. 9
Overview of UC and CD imaging
Imaging in patients with (suspected) IBD colitis has 3 major goals: Distinguishing UC from CD, assessment of disease activity and extension, and cancer surveillance in long-standing colonic IBD. 11 Colonoscopy is the primary imaging modality for IBD. The disadvantage of this technique is its relative invasiveness as compared with radiological techniques such as computed tomography (CT), ultrasound, magnetic resonance imaging (MRI), and scintigraphy. Diagnostic colonoscopy carries a small risk of 1:3000 to 1:5000 for perforation. 12 Double-contrast barium enema (DCBE), CT, and scintigraphy involve a radiation burden to the patient, which is undesirable, since these patients are often young and since (because of the chronic course of IBD) repeated examinations are often necessary over a number of years. Also, DCBE carries a small risk (1:25,000) of perforation. 13 The only noninvasive examination methods that do not have any radiation exposure to the patient are ultrasound and MRI. Ultrasound has the disadvantage of being more operator-dependent than is MRI.
The main goal of this review article is to summarize the literature about MRI in patients with IBD colitis and present MRI features of IBD colitis. The article also discusses the status of other examination methods and compares them with the results of MRI.
Examination and imaging techniques
Double-contrast barium enema
This examination method can be used to assess the extent and severity of IBD and to differentiate UC from CD. 10 Precise data on sensitivity and specificity for diagnosis and for determining the extent and severity of colonic IBD are lacking. In the modern colonoscopy era, DCBE is rarely used in IBD patients. The calculated effective DCBE radiation dose is reported to be 6.4 to 17.0 mSv. 14
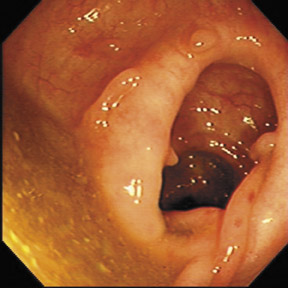
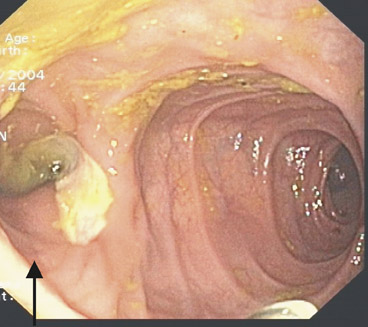
Colonoscopy
This method is more sensitive than DCBE in detecting early IBD changes. 15 Furthermore, it is the primary method for obtaining tissue samples for histologic examination. Even in normal macroscopic mucosa, histologic changes that are diagnostic for IBD can be seen. Therefore, it is important to take biopsies even from normal-appearing tissue. 15 A colonoscopic accuracy of 89% for distinguishing UC from CD has been reported. 11
Ultrasound
The sensitivity for the diagnostic value of ultrasound in the diagnosis of CD has been reported to be 67% to 96% and specificity 79% to 97%. 16 For UC, the main problem for ultrasound is that the rectum is a relatively inaccessible area; proctitis is correctly detected by ultrasound in only 15% of cases. 16 The reported sensitivity for UC detection by ultrasound is 77% to 83%. 16 Attempts have been made to assess disease activity by adding power Doppler to the ultrasound examination. This is based on the assumption that inflammation leads to neovascularization and dilation of feeding arteries and draining veins, which results in increased blood flow through the splanchnic circulation and bowel wall. Conflicting results have been reported regarding the correlation between splanchnic circulatory changes and disease activity. 17
CT
Only a few studies have compared CT results with the results of other imaging methods for evaluation of IBD. CT sensitivity for colonic IBD changes has been reported to be 69% to 84%. 18 An emerging technique is CT colonography. To the authors' knowledge, 3 studies discussing the value of this technique exist. 19-21 Biancone et al 19 report the results of CT colonography in 16 patients with CD and an ileocolonic anastomotic stricture. CT colonography had a sensitivity of 73% and a specificity of 100% compared with colonoscopy for detection of anastomotic recurrence. 19 Ota et al 20 showed that CT colonography had a good correlation with DCBE and colonoscopy for the detection of elevated lesions, such as inflammatory polyps and cobblestoning. Andersen et al 21 found a sensitivity for CT colonography of 100% for endoluminal lesions. Acute IBD was correctly identified in 63.6% and chronic IBD in 100%. 21 For ulcerated lesions, DCBE and colonoscopy were superior to CT colonography. 21 The median effective radiation dose of CT colonography is reported to be 7.2 mSv. 22
Scintigraphy
The 2 radiopharmaceuticals suitable for IBD detection are 111In oxine and 99mTc-hexamethylpropyleneamine oxime (HMPAO)-labeled leukocytes. 23,24 Since 99mTc-HMPAO has a higher sensitivity for the small bowel and gives better quality images and because of superior resolution and count density, it is the preferred agent. 23,24 Reported sensitivities and specificities for IBD detection are 83% to 98% and 92% to 100%, respectively. 23 The mean effective radiation dose for 99mTc-HMPAO is reported to be 3.3 mSv and 4.5 mSv for 111In-oxine. 25
MRI sequences
Large-bowel IBD imaging has been performed with field strengths ranging from 0.1T to 3T. The combination of sequences used most often is T2-weighted (T2W) turbo spin-echo (TSE) with T1-weighted (T1W) gradient echo (GRE). The T1W GRE is mostly performed before and after administration of gadolinium (Gd) in conjunction with fat suppression techniques. As early as 1997, it was shown that T1W GRE images in conjunction with intravenous Gd and oral barium were superior to T1W spin-echo (SE) and T2W TSE images for the depiction of normal and abnormal bowel wall, the depiction of mural thickening, and the overall visualization of the gastrointestinal tract. 26 Several years later, the same group reported that Gd-enhanced T1W GRE imaging better depicted the extent and severity of CD than did T2W single-shot (SS) TSE sequences. 27 Others concluded that SS sequences and Gd-enhanced T1W GRE sequences with fat suppression are complementary. Post-Gd sequences depicted inflammatory changes much better, whereas SS sequences defined air-filled loops much better because of the lack of air-related susceptibility artifact. 28 In a group of patients with CD, it was concluded that T2W MRI depicts CD lesions and assesses mural and transmural inflammation with the same accuracy as Gd-enhanced T1W MRI. These results were obtained with the use of an oral superparamagnetic contrast agent. 29
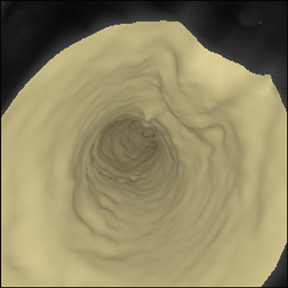
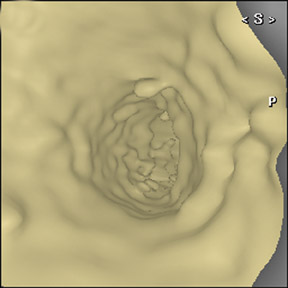
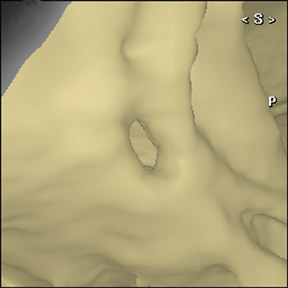
Recently, 3 groups described the use of MR colonography in IBD. The technique involves filling the colon with water or a water/Gd enema in order to distend it. This is used in conjunction with 3-dimensional (3D) T1W GRE techniques before and after the administration of intravenous Gd. 30-34
Filling and distension of the colon makes it possible to use more sophisticated postprocessing techniques, such as virtual colonoscopy. Whether filling and postprocessing techniques are helpful in diagnosing the type, severity, and extent of colonic IBD is unknown. A review on scanning techniques and reconstruction possibilities has been published. 35 For water enema MR colonography, it has been reported that a combination of T2W balanced GRE (B-GRE) and 3D T1W GRE after intravenous Gd is a good combination for MR colonography. The B-GRE gives superb contrast and motion insensitivity, and the 3D T1W GRE has the ability to image the whole colon within 1 breath-hold while maintaining relatively high spatial resolution. 36 In a small group of 5 patients, water enema MRI colonography was performed with both a 3D T1W GRE sequence (before and after administration of intravenous Gd) and a 2-dimensional (2D) T2W B-GRE sequence. Both sequences showed equal results in the visualization of IBD, but the image quality of the 2D T2W B-GRE sequence was rated superior over the 3D T1W GRE. 32
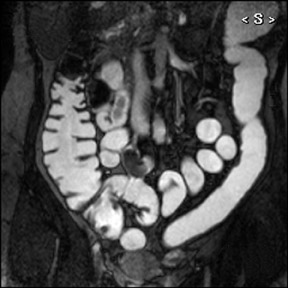
MRI appearance of normal colon wall
Several authors have described the MR features of normal and abnormal bowel wall in both patients and healthy volunteers. 25,37-39 These articles were published in the early and mid 1990s. In interpreting the results, however, it is important to keep in mind that current MRI sequences for abdominal imaging are much faster and have a higher temporal and spatial resolution than those reported in these articles. Normal colonic wall has signal intensity (SI) between that of water and muscle on T1W sequences, has a slightly higher SI than the surrounding fat on T1W sequences with fat suppression, and has signal intensity between that of fat and water on T2W sequences. 38 Normal colonic wall thickness is 3 to 4 mm, 37 although others report <5 mm. 39 After Gd enhancement, the wall appears as a thin enhancing line (Figure 1). 37 Normal contrast enhancement is reported to be minimal. 37 An enhancement percentage of 108% for normal colonic wall has been reported. 38 Ajaj et al 31 reported a mean colonic wall thickness in healthy volunteers on a 3D T1W GRE sequence after intravenous Gd of 2 mm, while D'Arienzo et al 40 reported a <4mm wall thickness in healthy volunteers. Wall thickness of noninflamed segments in patients with UC was 3.7 mm ± 0.6 mm. 41
MRI features of IBD
The most striking abnormalities in both UC and CD are wall thickening and increased enhancement.
Wall thickening
Measured wall thickness is dependent on the spatial resolution of the sequence and the precision of the measurement. A true cutoff point between normal and inflamed bowel wall cannot be established by interpreting the literature. The median wall thickness in CD that is reported in different studies ranged from 4.9 to 6.7 mm and in UC from 4.7 to 9.8 mm. 41-48 Ranges of wall thickness were 2 to 12 mm for CD and 3.5 to 11.6 mm for UC. 41-48 In general, the more severe the inflammation, the thicker the colonic wall. 44-46 After medical treatment, both the colonic and terminal ileal wall become thinner. 47 The wall thickness of the terminal ileum has been reported to be <3 mm in healthy volunteers and 5.9 mm ± 1.3 mm in patients with IBD. 48 When interpreting these results along with the results in healthy volunteers, a colonic wall thickness <3 mm can be appreciated as normal, 3 to 4 mm as a "gray zone," and >4 mm as pathologic.
Increased enhancement
There are many ways to define and measure increased enhancement. In some articles, it is determined visually, compared with either enhancement of the liver or of the psoas muscle. Authors use different formulae on different workstations with different Gd-enhanced sequences and different sequence timing. The results, especially the quantitative calculations and measurements, are thus difficult to reproduce and compare.
In patients with UC, an overlap in the percentage of enhancement of inflamed and noninflamed segments has been reported, with enhancement of inflamed segments of 40% to 313%, enhancement of noninflamed segments at 7% to 63%, and enhancement in a healthy control group at 10% to 66%. 44 Both diffuse enhancement (all parts of the bowel wall) and layered enhancement (more enhancement of mucosa and serosa) have been reported in patients with CD. 46,49 Layered enhancement seems to be a particularly good indicator of active CD. 46,49 Also, increased mesenteric vascularity, in the form of dilated, terminal branches of the mesenteric arteries (vasa recta), is a feature of IBD. 46,49 This is the so-called comb sign, which is produced by increased flow and fibrofatty proliferation in the mesentery of inflamed bowel. 50 This sign is not specific for IBD, as it can also occur in forms of vasculitis and bowel ischemia. 50 In a study of patients with CD of the terminal ileum, using T1W GRE sequences after Gd, the enhancement of inflamed terminal ileum was 266% (range 105% to 450%). 51
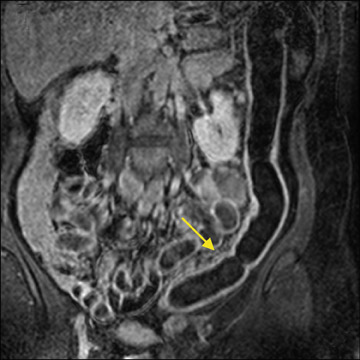
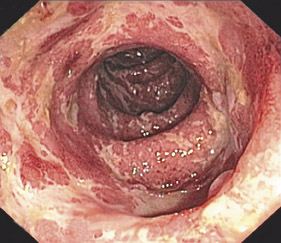
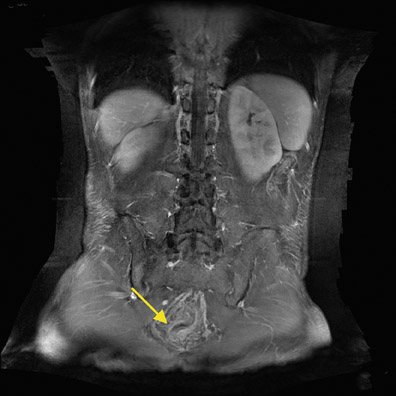
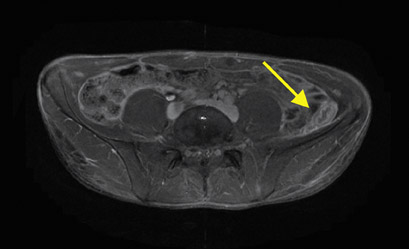
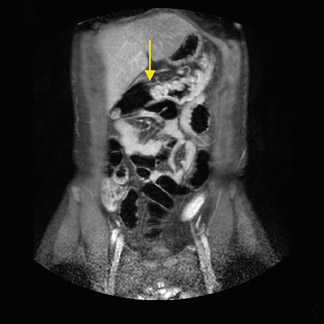
Specific features of UC
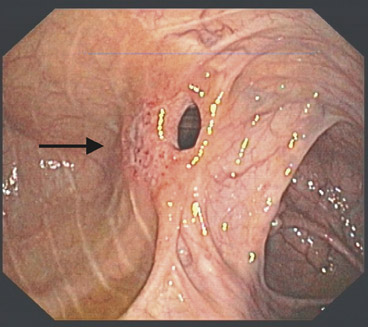
Figures 2 through 5 illustrate and Table 1 summarizes the MRI features of UC. In a specimen study, a high SI of both mucosa and submucosa of patients with active UC was found on T1W and T2W images. 52 In patients with inactive disease, the colonic specimen showed a low SI of both mucosa and submucosa on T1W and T2W images. 52 Reported MRI criteria for UC include wall thickening from the rectum to the proximal colon and enhancement of the mucosa with no or less enhancement of the submucosa. 44,53 This produces a low SI stripe- the so-called submucosal stripe. 44,53 Furthermore, increased SI of the pericolonic fat has been reported. 45 Backwash ileitis in UC shows mild enhancement and no wall thickening. 54 Furthermore, the loss of haustral markings has also been reported to be an MRI feature of UC. 55 In cases of long-standing colitis, pseudopolyps can develop.
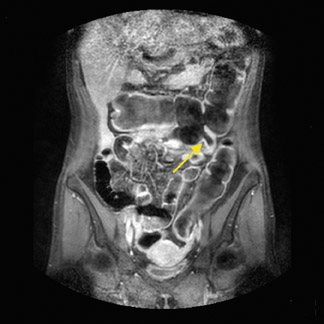
Specific features of CD
Figures 6 through 8 illustrate and Table 1 lists the specific MRI features of CD. MRI criteria for CD include involvement of the terminal ileum, enhancement of the entire bowel wall (full thickness and transmural enhancement), relative sparing of the rectum, wall thickening, increased SI of bowel wall and surrounding fat, asymmetry, skip lesions, fistulae, infiltration of fat around inflamed bowel wall, abscesses, lymphadenopathy, and fibrofatty proliferation. 44,46,53,56 Fibrofatty proliferation is present if an increase in mesenterial fat results in separation or displacement of adjacent bowel loops. 46
Comparison of modalities
MRI versus CT
Low et al 57 made a diagnostic comparison of CT and MRI in 26 patients with CD who underwent both MRI and CT. Patients fasted for 3 hours before each study. One hour prior to scanning, patients drank 1350 mL of 2% dilute barium contrast. For MRI, rectal water (500 to 1000 mL) was administered; for CT, 500 to 1000 mL of iodinated contrast was administered. For both examinations, 1 mg of intravenous glucagons was administered. Coronal and axial T1W GRE sequences with a slice thickness of 10 mm were performed, before and after intravenous Gd. Helical CT was performed with a pitch of 1 and a collimation of 10 mm. Thickening of the bowel wall and increased enhancement were evaluated. Colonoscopy, barium enema, or surgery was used as a gold standard. In a total of 65 diseased bowel segments, 54 were depicted by MRI and 41 by CT. This resulted in a sensitivity of 83% and a specificity of 91% for MRI. For CT, these figures were 63% and 91%, respectively. MRI had an accuracy of 89% and CT of 82%. 57
MRI versus DCBE
Sardanelli et al 41 reported the results of a study comparing MRI with DCBE in 6 patients with UC. MRI was performed after bowel cleansing, and the colon was filled with a mixture of air and superparamagnetic iron particles. Intravenous Gd was also administered. A T1W GRE sequence with 8-mm thickness and an 0.8-mm interslice gap was used. In addition to the previously mentioned wall thickness and enhancement percentage, the authors reported that MRI findings of disease extension were consistent with the DCBE findings. 41 Nozue et al 55 also described their results in 6 patients with UC. In 5 of the 6 patients, MRI was in accordance with DCBE and endoscopy for assessing disease extent. 55
MRI versus ultrasound
Table 2 presents the conflicting results of 4 published articles that compared MRI findings with those of ultrasound. 49,58-60 The study by Potthast et al 58 is more focused on small bowel abnormalities. In addition to sensitivity and specificity for diagnosing CD in the terminal ileum, this article also described other parameters. Sensitivity of MRI for the number of affected bowel segments was 97.5% with a specificity of 100%, whereas ultrasound scored 76% and 75%, respectively. For stenosis, MRI had a sensitivity of 100% and a specificity of 96%, and ultrasound a sensitivity of 58% and specificity of 100%. For abscesses, MRI showed a sensitivity of 100% and a specificity of 97%, whereas ultrasound showed a sensitivity of 89% and a specificity of 92%. For fistulae, MRI had a sensitivity of 87% and a specificity of 93%, while ultrasound had a sensitivity of only 31% and a specificity of 100%. 58
MRI versus nuclear medicine
Neurath et al 61 reported the results of a study of 59 patients with CD, who underwent fluorodeoxyglucose-positron emission tomography (FDG-PET) scanning, antigranulocyte scintigraphy, and MRI. In 28 patients, there was also involvement of the terminal ileum and colon. These patients also underwent ileocolonoscopy, which served as the gold standard. MRI was performed on a 1T system. Axial and coronal T2W TSE sequences, coronal T1W GRE sequences before and after intravenous Gd, and axial and coronal T1W GRE fat-saturated sequences after Gd were peformed. No colon filling was performed-only small bowel filling with 1 L of mannitol solution orally. Slice thickness was 8 mm. For the detection of inflamed areas in the terminal ileum and the colon, FDG-PET had a sensitivity of 85% and a specificity of 89%. MRI had a sensitivity of 67% and a specificity of 93% and scintigraphy a sensitivity of 41% and a specificity of 100%. 58
MRI versus colonoscopy
Several articles have compared findings of MRI and colonoscopy and have reported sensitivity and specificity values 30,31,46,54 (Table 3).
Schreyer et al 30 and Ajaj et al 31 have described the results of MR colonography, and their results are conflicting. Sensitivity on a per-patient basis ranges from 75% to 91%. On a per-segment basis, reported sensitivities range from 32% to 89%. A specificity of 71% on a per-patient basis is mentioned by Koh and coworkers 46 only. Specificity on a per-segment basis has been reported from 67% to 100%. Since MR colonography is a developing technique, its final place in the diagnosis of IBD is yet to be determined. Sensitivity and specificity values might improve in the near future with faster scanning techniques and 3T MRI.
Summary of MRI studies
The most striking MRI abnormalities encountered in IBD colitis are wall thickening and increased enhancement. A thickness ≥4 mm has to be considered pathologic, whereas a thickness of 3 to 4 mm should raise suspicion and other IBD characteristics should be sought. Besides these shared characteristics, UC and CD have their own more or less specific characteristics (Table 1).
The first goal in imaging patients with suspected IBD colitis is to distinguish UC from CD. The extent to which MRI can accomplish this remains uncertain. In a study performed in the early 1990s, MRI provided the correct diagnosis in 17 of 18 patients. 44 Alternatively, MRI permitted the correct diagnosis in only 50% of the patients with CD in a study of pediatric patients. 53 In another pediatric study of IBD patients, MRI had a sensitivity of 96% and specificity of 92% for distinguishing CD from UC. 62
The second imaging goal relates to defining disease extent and activity. Attempts have been made to correlate MRI results, such as wall thickening and wall enhancement, with endoscopy scores, activity indices, and laboratory parameters. These study results are both conflicting and difficult to reproduce because of the different definitions of endoscopic and MRI severity and the subjective aspect of activity indices. More uniformity for endoscopic and MRI grading of inflammation is needed to reliably compare study results. In UC, a significant correlation between wall thickness, enhancement percentage, and endoscopic abnormalities has been reported. 40 The same has also been reported in a mixed population of CD and UC patients. 44 A significant correlation has been reported between the Crohn's Disease Activity Index (CDAI), maximum enhancement, and time to enhancement peak for the terminal ileum. 49 A good correlation, 54,63 as well as a poor correlation, 53 between enhancement percentage and endoscopic severity in mixed patient groups has been reported. Three articles found no correlation between the CDAI and MRI findings, 46,56,61 while another article found a significant correlation. 64
Recently, a significant correlation was found between the degree of bowel wall enhancement and CDAI and between the change of signal intensity of the bowel wall after the administration of intravenous Gd and the inflammation severity at colonoscopy. 33,65 Furthermore, it has been reported that both wall thickening and bowel wall enhancement decrease in patients with CD that is moving from the active phase into remission due to treatment. 66 In 2 studies, MRI results were compared with Crohn's disease endoscopic index of severity (CDEIS). 67,68 The results of 31 patients undergoing 1.5T MRI showed a moderate-to-strong correlation between MRI severity and CDEIS (r = 0.62). 67 The first publication about the use of 3T abdominal MRI in 20 patients with CD showed no statistically significant correlation between MRI grading and CDEIS. 68
On determining the extent of UC, MRI and DCBE have been shown to have equivalent results, but only in 12 patients from 2 studies. 41,55 Conflicting results on the extent of IBD has been reported, both when MRI was compared with ultrasound and with colonoscopy. 30,31,46,49,54,58-60
Also, a significant correlation between MR findings and increase of acute phase reactants had been described. 56 No data exist on cancer surveillance in long-standing colonic IBD and the role of MRI in this area.
One study on the diagnostic capabilities of MRI compared with other techniques showed that MRI has higher sensitivity than CT for the diagnosis of inflamed bowel segments. 57 MRI has scored better than scintigraphy, and FDG-PET showed promising diagnostic results. 61 Conflicting results have been reported between MRI and ultrasound and MRI and colonoscopy. 30,31,46,49,54,58-60 Many reasons for the conflicting study results can be proposed, such as inclusion of patients with different disease severity, different MRI and ultrasound definitions of imaging features of IBD, different "gold" standards, different ultrasonographers and colonoscopists, and different MRI sequences. The chosen enema composition also likely plays an important role in achieving higher sensitivity in MR colonography. Schreyer et al 30 used a water/Gd enema, which is bright on T1W sequences, and makes the appreciation of colonic wall enhancement more difficult. Ajaj et al 31 used a water enema, which is black on T1W sequences. The enhancing colonic wall is better appreciated against a black background lumen and suppressed fat signal than against a white background lumen and suppressed fat signal. Because of higher sensitivity and specificity, the black lumen technique seems to be favorable for IBD detection compared with the bright lumen, although no comparative research exists.
Recent research shows that because of limited spatial resolution, MRI is not able to show superficial IBD lesions, such as superficial ulcerations and mucosal erythema. 69 This is confirmed by others, showing that slight inflammation of an anastomosis is diagnosed by colonoscopy but is not visible on MR colonography. 34 Therefore, scientific results point to a role of MRI in IBD patients with moderate or severe complaints, where wall thickening and increased enhancement are more likely to be present.
Conclusion
The current status of MRI in IBD colitis is that of a promising, noninvasive technique for imaging extent of more severe colonic IBD. When using MRI for this group of patients, one has to keep in mind that in a normal-appearing colon, superficial ulcerations and mucosal erythema can be present and that the disease extent is probably greater than may be indicated on MRI.