Current applications of MRI in emergent gastrointestinal diseases
Images




Dr. LeBedis is an Assistant Professor, Dr. Penn is a Radiology Resident, Dr. Gupta is an Associate Professor, Dr. Tkacz is an Associate Professor, and Dr. Soto is a Professor of Radiology, Boston University Medical Center in Boston, MA; and Dr. Broder is a Radiologist, Lahey Clinic, Burlington, MA.
The widespread availability and diagnostic capabilities of ultrasound (US) and computed tomography (CT) have made these tools invaluable in triaging patients with abdominal pain in busy emergency departments. Given the variety of diagnostic possibilities in patients with abdominal pain and their sometimes urgent ensuing treatments, a rapid and accurate diagnosis is of paramount importance. For example, emergent abdominal surgical procedures account for approximately 53% of all nontrauma-related surgical interventions performed in the acute care setting.1
The American College of Radiology (ACR) rates US and CT with a high priority score of 6 to 9 for acute abdominal and pelvic conditions in nonpregnant adults (1=least appropriate; 9=most appropriate). However, in pregnant or young patients, the appropriateness of CT drops to 4 to 6, depending on the indication.2 Although US yields high sensitivities and specificities in abdominal and pelvic pathology in the hands of an expert, it is highly operator and patient dependent. For example, obesity can affect the ability of the ultrasound beam to penetrate the soft tissues, and patient motion and bowel gas can prevent visualization of underlying organs.3 The main disadvantage of CT is exposure of the patient to ionizing radiation.4 In younger patients, the radiation dose considerably increases the risk of developing a radiation-induced cancer.5
With advances in magnetic resonance imaging (MRI) sequences, protocols, and coil technology, as well as growing familiarity with the modality on both the part of technologists and radiologists, MRI has become a viable alternative to CT. MRI can assess the entire abdomen within minutes, yielding diagnostic sensitivities and specificities similar to those of CT and without the operator dependence encountered in US. Acute abdominal and pelvic conditions that can be rapidly diagnosed with MRI include choledocholithiasis, acute cholecystitis, acute pancreatitis, bowel inflammation in the setting of inflammatory bowel disease (Crohn’s disease and ulcerative colitis) and appendicitis.6,7 In addition, MRI is critical in the characterization of indeterminate CT and US findings.7 The ACR, however, rates MR imaging of nonpregnant patients in acute abdominal and pelvic conditions with a medium appropriateness score of 4 to 6 because of its limited availability, longer acquisition times, higher cost and lack of incremental diagnostic gain compared with CT. The appropriateness score for evaluation of a pregnant woman with fever, leukocytosis and suspected appendicitis jumps to 7, just below the appropriateness score of 8 for US.2
MRI provides several notable advantages over US and CT in the assessment of abdominal pathologies. The first is its lack of ionizing radiation. This feature is of particular benefit to pediatric patients and, by extension, to pregnant women.5,8 Another subset of patients who undergo numerous CT scans for recurring abdominal pain are patients with inflammatory bowel disease. A second advantage of MRI is the ability to image patients who have allergies to CT contrast agents. Third, MRI can delineate certain disease entities better than US or CT, such as choledocholithiasis, where bowel gas and patient body habitus can obscure acoustic windows on US exams and many stones can go undetected on CT. Last, MRI provides superior contrast resolution and excellent characterization of pathologic tissue.9
Disadvantages of MR imaging in evaluating acute gastrointestinal conditions include its high cost, limited availability, longer examination times compared to US and CT, and its incompatibility with equipment used for intensive care and patient monitoring.7 In addition, MR imaging also has poorer spatial resolution and higher sensitivity to motion-related artifacts than does CT.10
Protocols
Minimizing MR imaging acquisition times by tailoring protocols to the clinical question at hand is of paramount importance in the emergent setting.
Oral contrast
The clinical indication for the study determines the choice of oral contrast. For MR cholangiopancreatography (MRCP), we prefer a negative oral contrast to minimize background bowel signal on the heavily T2-weighted MRCP sequences, allowing unobstructed visualization of the pancreaticobiliary tree. Similarly, for patients being evaluated for acute appendicitis, we prefer a negative oral contrast, which renders normal bowel dark, as compared with an obstructed appendix which can be filled with T2 hyperintense fluid. At our institution, a 50/50 vol/vol combination of ferumoxsil (Gastromark; Mallinckrodt Medical, St. Louis, MO) and barium sulfate suspension is utilized as the negative oral contrast for MRCP and acute appendicitis studies. It is particularly useful if the MR image is nondiagnostic for appendicitis, as the patient is simultaneously prepared to undergo a CT examination, without any additional delay for appropriate opacification of bowel. For imaging of inflammatory bowel disease, we prefer a neutral oral contrast agent, such as Volumen, which has improved bowel distention given the presence of 2% sorbitol. This oral contrast preparation has the added benefit of demonstrating maximal tissue contrast against the bowel wall on T1-weighted, gadolinium-enhanced sequences, where the bowel lumen is hypointense and the wall is hyperintense, and vice versa on T2-weighted sequences.
Sequences
If the patient is capable, breath-hold sequences are ideal, given their short acquisition times. Otherwise, lengthier free breathing or respiratory-triggered imaging protocols may be employed. Two-dimensional T1-weighted, gradient-recalled echo (GRE) sequences may be helpful in the workup of acute appendicitis, as gas or negative oral contrast within the appendix (suggesting luminal patency), will demonstrate susceptibility artifact on these sequences. Intravenous gadolinium-based contrast agent use is useful for detecting acute inflammation of the bowel wall, but is contraindicated in early pregnancy.
Single-shot half-Fourier T2-weighted turbo spin-echo sequences (SSFSE, SSTSE, or HASTE, based on the vendor) are particularly useful for bowel imaging with a neutral oral contrast agent, given their excellent spatial resolution, T2-weighting and rapid scan times. But they may demonstrate dark signal voids in fluid-filled bowel. Balanced steady-state free precession sequences, (TrueFISP, FIESTA and balanced FFE, based on the vendor), are also useful for bowel imaging, given their rapid acquisition time and lack of bowel signal voids, but they are prone to susceptibility artifacts that can be created in the presence of Gastromark. Balanced gradient echo techniques have the added benefit of creating “white blood” noncontrast MR angiographic images. Short tau inversion-recovery (STIR) and respiratory-triggered, T2-weighted, chemically fat-suppressed turbo SE sequences can be helpful, but scan times are inherently longer due to their multi-shot image techniques and longer TR.
For MRCP studies, we use heavily T2-weighted 2D SSTSE (20 mm thick) slabs, obtaining 5 radial slices in approximately 10-15 seconds. In addition, a coronal 3D, respiratory-triggered TSE sequence (1.6 mm slice thickness) is acquired, providing improved signal-to-noise ratio (SNR) compared with 2D techniques, and the ability to perform multiplanar reformatted images. Scan times, however, may be up to 5 minutes.
Post-gadolinium 3D T1-weighted sequences (such as THRIVE, VIBE, LAVA and FAME, depending on the MR vendor) can be useful in detecting active bowel inflammation, particularly in inflammatory bowel disease. These sequences provide high-resolution interpolated sections (2-3 mm thick) while allowing acquisition of dynamic phases after administration of intravenous gadolinium-based contrast (rate, 2 mL/sec; volume, 20 mL). To evaluate suspected inflammatory bowel disease, we add 3-plane SSTSE sequences and balanced gradient echo and coronal T1 dynamic, 3D fat-suppressed gradient echo sequences with and without gadolinium, using a neutral oral contrast. The examination is typically 20-30 minutes. 11,12
To evaluate suspected appendicitis, usually in the setting of pregnancy, our imaging protocol consists of 3-plane SSTSE sequences with and without chemical fat suppression, and axial T1-weighted, in-phase and opposed-phase GRE sequences with a negative oral contrast agent. Gadolinium is avoided in pregnant patients. Although the safety of MRI for the fetus has not been proven according to U.S. Food and Drug Administration guidelines, no human teratogenic or carcinogenic effects of MRI have been described in the literature.9 The effects of fetal exposure to high magnetic fields, gradient shifts and radiofrequency energy deposition remain largely unknown.7 At our institution, these facts are discussed with our pregnant patients, and written informed consent is obtained.
Clinical applicationsCholedocholithiasis
Choledocholithiasis, the presence of an obstructing stone in the CBD either from the passage of a gallbladder stone through the cystic duct, or primary formation of stones within the common bile duct, can lead to acute biliary obstruction with resultant pain, jaundice, fever, cholangitis, pancreatitis or sepsis.
Choledocholithiasis is encountered in 10% to 15% of the cholecystectomies performed each year,13,14 confounding the diagnosis and management of patients with right upper quadrant pain. Most patients presenting with right upper quadrant pain will undergo sonographic evaluation of the biliary tree for cholecystitis, given the high sensitivity and specificity of US for diagnosing this entity.15
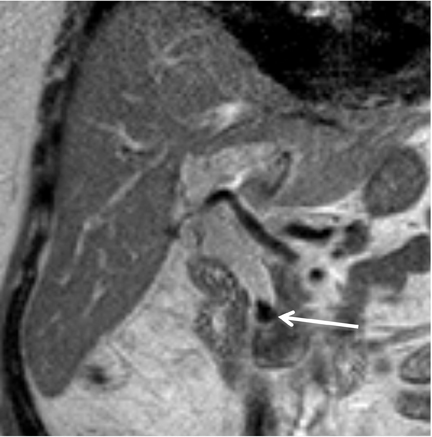
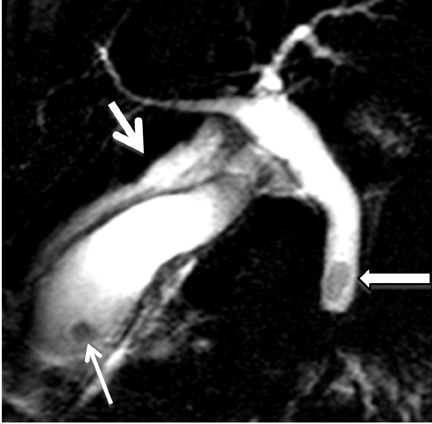
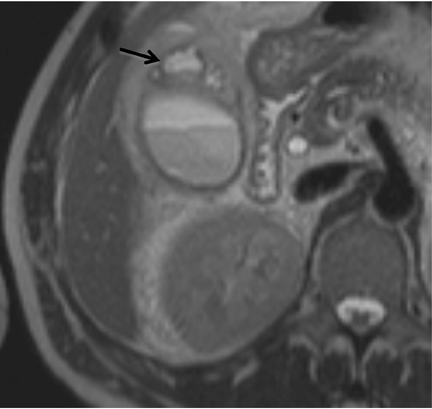
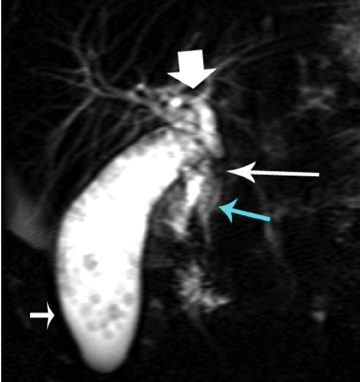
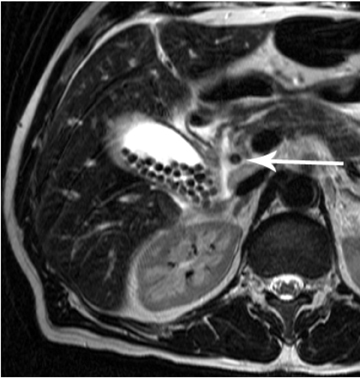
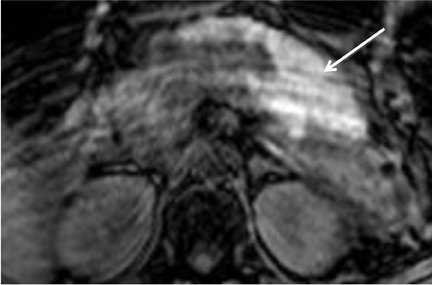
Choledocholithiasis is suspected dilation of the common bile duct (>8 mm) is present on US or CT. However, visualization of the distal common bile duct with these modalities can be limited. On US, overlying bowel gas can obscure the distal common bile duct and make stones difficult to visualize,15 and CT has inherent limitations for detecting choledocholithiasis. Thus, MRCP is typically performed when there is clinical suspicion for common bile duct stones given its high sensitivity and specificity (97% to 99% and 95%to 99%, respectively) for detecting common bile duct abnormalities. On MRCP, calculi appear as low signal intensity filling defects in the biliary tree against the high signal intensity bile (Figure 1). The differential diagnosis for a biliary tree filling defect includes air, neoplasm, blood clot and sludge.
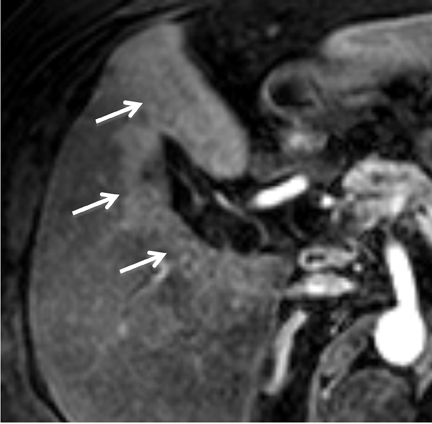
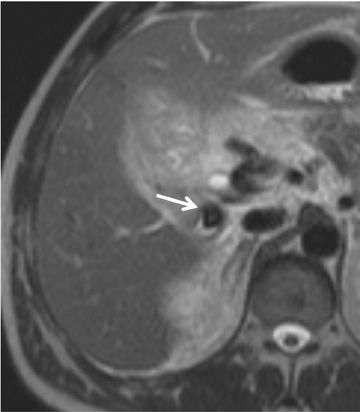
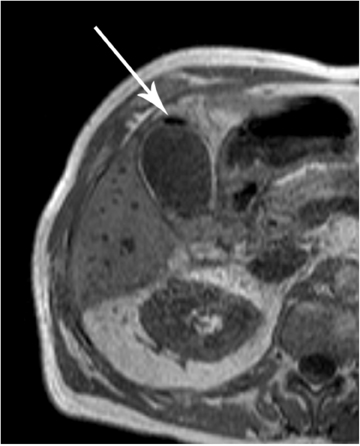
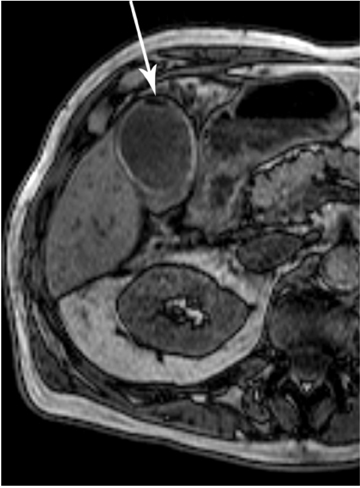
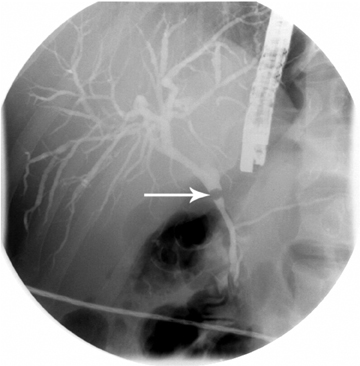
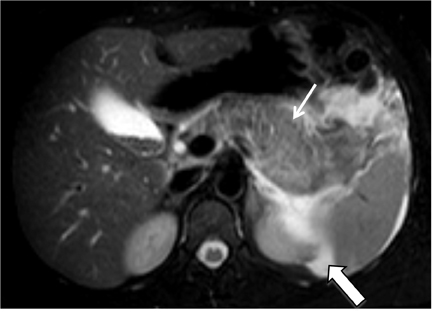
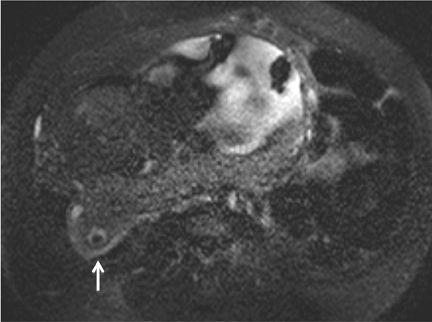
MRCP plays a crucial role in management of patients with cholecystitis in whom choledocholithiasis is suspected since it can accurately triage patients to endoscopic retrograde cholangiopancreatography (ERCP) and direct the appropriate surgical intervention. Although MRI is not used as a screening test for cholecystitis, the condition can be depicted on MR as pericholecystitic fluid, gallbladder wall thickening, and gallbladder wall edema on T2-weighted images. Transient hyperenhancement of the adjacent hepatic parenchyma can also be seen (Figure 2). Complications of acute cholecystitis such as gangrenous cholecystitis and Mirizzi syndrome can be diagnosed with MRCP.7 Gangrenous cholecystitis manifests as segmental absence of mucosal enhancement on contrast-enhanced MR images (Figure 3) or it can be visualized as air within the wall of the gallbladder, best seen as a focus of blooming artifact on opposed-phase, T1-weighted images (Figure 4). Mirizzi syndrome is the mechanical obstruction of the hepatic duct by a stone impacted in the adjacent cystic duct (Figure 5).
Pancreatitis
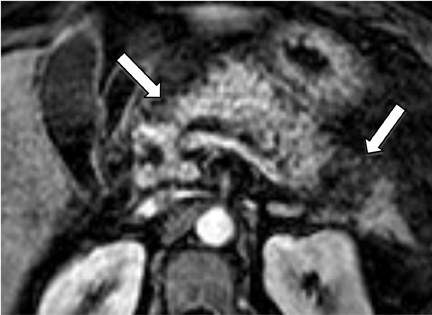
Gallstones are the inciting factor in 50% of patients with acute pancreatitis,16 as stones that migrate into the distal common bile duct can obstruct the pancreatic duct. Patients typically manifest with persistent epigastric pain, nausea and vomiting. Elevation of serum lipase and amylase is common. MRCP has been shown to be comparable to contrast-enhanced CT in the diagnosis of equivocal cases acute pancreatitis and for assessment of disease severity.17 Acute pancreatitis manifests as glandular enlargement (edema), periglandular inflammatory changes, and intra- and peri-pancreatic fluid collections on MR, particularly on fluid-sensitive sequences with fat suppression (Figure 6). Pancreatic necrosis is a complication of severe pancreatitis in which there are regions of nonviable pancreatic parenchyma (Figure 7); it carries higher morbidity and mortality rates relative to uncomplicated pancreatitis.18 The advantage of MRCP lies in its ability to identify choledocholithiasis as the cause of acute pancreatitis and to triage the appropriate patients to ERCP where sphincterotomy and retrieval of impacted stones can be performed. A potentially fatal complication of acute pancreatitis is hemorrhagic pancreatitis, where severe inflammation and regional necrosis cause vessel erosion with resultant hemorrhage into the pancreatic bed, retroperitoneum, peritoneal cavity or gastrointestinal tract.19 Hemorrhagic pancreatitis is depicted on T1-weighted sequences as a region of high signal intensity within the pancreas or adjacent structures (Figure 8).
Appendicitis/bowel inflammation
MR enterography (MRE) is beneficial in the emergent setting to evaluate pregnant patients with suspected acute appendicitis and patients with acute symptoms with inflammatory bowel disease (IBD). Pregnant patients benefit from MRE by obtaining imaging of the appendix without the hazards of fetal ionizing radiation. In patients with IBD, MRE can assess for active inflammation and its related complications without ionizing radiation.
The prevalence of appendicitis does not change during pregnancy and acute appendicitis is the most common cause of emergent gastrointestinal surgery in a pregnant patient.20 The diagnosis of acute appendicitis in pregnancy is challenging due to displacement of the appendix by the uterus. In addition, during pregnancy the classic signs of appendicitis (leukocytosis, fever, and right lower quadrant pain) are nonspecific, as leukocytosis can be normal in pregnancy.
At our institution, an algorithm based on the ACR Appropriateness Criteria was developed to assess pregnant patients with potential appendicitis. All pregnant patients with suspected appendicitis are initially evaluated with a directed abdominal ultrasound study. Prior to being transported to the ultrasound suite, the patient drinks a negative oral contrast agent as detailed above. In our experience, ultrasound visualization of the appendix is poor. If the ultrasound is nondiagnostic, MR imaging without intravenous gadolinium is performed 2 hours after oral contrast ingestion. If the appendix is not visualized on MR imaging, then the patient undergoes CT with intravenous noniodinated contrast agent. The dual oral contrast mixture provided in the emergency room prepares the patient for MR and CT simultaneously.
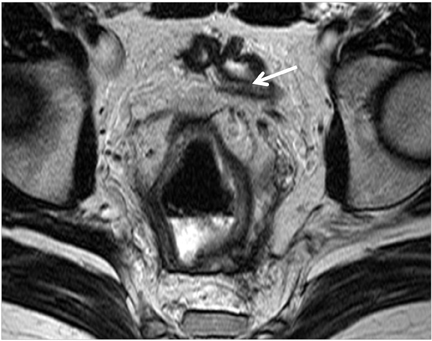
The MR imaging findings of acute appendicitis include appendiceal diameter of >7 mm (Figure 9) and a wall thickness of >2 mm, which are both best visualized on T2-weighted sequences.9 Periappendiceal and appendiceal inflammation and edema are best imaged on STIR sequences; they appear as hyperintense signal within the appendiceal wall or the surrounding tissue (Figure 9).12, 21-23 MR imaging can demonstrate fluid signal within the appendix, which can also suggest acute appendicitis. Overall, MR imaging demonstrates high sensitivity (97% to 100%) and specificity (92% to 93%) in acute appendicitis.12
A growing number of patients with IBD present to the emergency room with acute complaints;24 MRE can facilitate diagnosis of acute flares and/or complications. Crohn’s disease is a chronic granulomatous inflammatory process of the gastrointestinal tract that affects approximately 400,000 to 600,000 people in North America.25 The etiology of Crohn’s disease is complex and likely involves immunologic, genetic, infectious, vascular, dietary and environmental factors.26, 27
Crohn’s disease usually involves the small bowel (80%), but it can affect any portion of the gastrointestinal tract.26 Gastrointestinal involvement can be separated by uninvolved bowel termed “skip lesions”.26,27 Crohn’s disease consists of superficial mucosal ulcerations (aphthous ulcers) and deep fissuring ulcers. The deep fissuring ulcers can penetrate the mucosa and result in submucosal inflammation, edema, and bowel wall thickening. The submucosal edema results in increased T2-weighted signal intensity of the submucosa.27 The enhancing mucosa and serosa, combined with the submucosal edema on contrast-enhanced T1-weighted, fat-suppressed sequences, produces a “target” or “trilaminar” appearance of the bowel. Transmural inflammation and ulcerations in Crohn’s disease can result in sinus tracts, fistulas, and abscesses, while the chronic inflammatory changes can result in strictures and bowel obstruction (Figure 10).
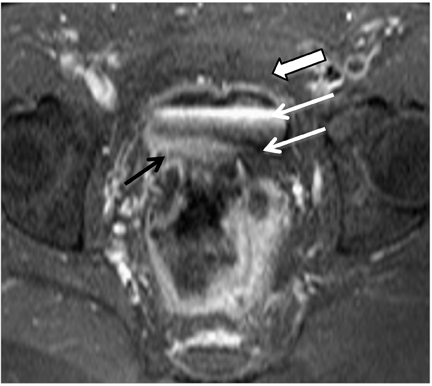
Patients with ulcerative colitis also benefit from MRE. For example, ulcerative colitis patients who are status post-ileal pouch-anal anastamosis can obtain MRE to accurately diagnose complications such as “pouchitis” (Figure 11), abscess, fistulas, strictures, and venous thrombi.28
MR and CT enterography in Crohn’s disease demonstrate equivalent rates of detecting active disease and complications.29 The cumulative radiation doses associated with CT scans for patients with Crohn’s disease is substantial, and MRE can significantly reduce their overall radiation exposure.30, 31
Conclusion
MR imaging can be used to accurately and rapidly diagnose and triage patients with acute abdominal pain presenting to the emergency department. MR imaging of the abdomen is particularly advantageous in subsets of patients who are at higher risk for radiation-related cancers, such as pediatric patients, pregnant women and patients who are serially imaged, and in patients with allergies to iodinated CT contrast agents. The relatively lengthy examination times and higher cost compared to CT, lack of availability, and its incompatibility with patient monitoring devices currently hinders the use of MR. As MR imaging techniques continue to evolve and attempts grow to reduce patient exposure to imaging-related radiation, this modality may play a larger role in delivering health care to patients with abdominal pain in the emergent setting.
References
- Ciesla DJ, Moore EE, Moore JB, et al. The academic trauma center is a model for the future trauma and acute care surgeon. J Trauma. 2005;58:657-662.
- Rosen MP, Ding A, Blake MA, et al. ACR Appropriateness Criteria® 2010. American College of Radiology Web site. http://www.acr.org/. Accessed July 1, 2011.
- Hanbidge AE, Buckler PM, O’Malley ME, Wilson SR. From the RSNA refresher courses: Imaging evaluation for acute pain in the right upper quadrant. Radiographics. 2004;24:1117–1135.
- Aldrich JE, Bilawich AM, Mayo JR. Radiation doses to patients receiving computed tomography examinations in British Columbia. Can Assoc Radiol J. 2006;57:79–85.
- Heverhagen JT, Klose KJ. MR Imaging for acute lower abdominal and pelvic pain. Radiographics. 2009;29:1781-1796.
- Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for nonobstetric conditions: Algorithms and radiation dose considerations. Radiographics. 2007;27:1705–1722.
- Tkacz JN, Anderson SA, Soto J. MR imaging in gastrointestinal emergencies. Radiographics. 2009;29:1767-1780.
- Oto A, Ernst RD, Shah R, et al. Right lower quadrant pain and suspected appendicitis in pregnant women; evaluation with MR imaging – initial experience. Radiology. 2005;234:445-451.
- Singh A, Danrad R, Hahn PF, et al. MR Imaging of the acute abdomen and pelvis: Acute appendicitis and beyond. Radiographics. 2007;27:1419-1431.
- Keeler EK, Casey FX, Engels H, et al. Accessory equipment considerations with respect to MRI compatibility. J Magn Reson Imaging. 1998;8:12-18.
- Pedrosa I, Rofsky NM. MR imaging in abdominal emergencies. Radiol Clin North Am. 2003;41:1243-1273.
- Pedrosa I, Levine D, Eyvazzadeh AD, et al. MR imaging evaluation of acute appendicitis in pregnancy. Radiology. 2006;238:891-899.
- Collins C, Maguire D, Ireland A, et al. A prospective study of common bile duct calculi in patients undergoing cholecystectomy: Natural history of choledocholithiasis revisited. Ann Surg. 2004;239:28-33.
- Phillips EH, Toouli J, Pitt HA, Soper NJ. Treatment of common bile duct stones discovered during cholecystectomy. J Gastrointest Surg. 2008; 12:624-628.
- Laing FC, Jeffrey RB Jr, Wing WV, Nyberg DA. Biliary dilatation: Defining the level and cause by real time US. Radiology. 1986;160:133-134.
- Stimac D, Miletić D, Radić M, et al. The role of nonenhanced magnetic resonance imaging in the early assessment of acute pancreatitis. Am J Gastroenterol. 2007;102:997–1004.
- Viremouneix L, Monneuse O, Gautier G, et al. Prospective evaluation of nonenhanced MR imaging in acute pancreatitis. J Magn Reson Imaging. 2007;26:331-338.
- Sharma M, Banerjee D, Garg PK. Characterization of newer subgroups of fulminant and subfulminant pancreatitis associated with a high early mortality rate. Am J Gastroenterol. 2007;102:2688-2695.
- Frey CF. Hemorrhagic pancreatitis. Am J Surg. 1979;137:616–623.
- Longo SA, Moore RC, Canzoneri BJ, Robichaux A. Gastrointestinal conditions during pregnancy. Clin Colon Rectal Surg. 2010;23:80-89.
- Birchard KR, Brown MA, Hyslop WB, et al. MRI of acute abdominal and pelvic pain in pregnant patients. AJR Am J Roentgenol. 2005;184:452–458.
- Oto A, Srinivasan PN, Ernst RD, et al. Revisiting MRI for appendix location during pregnancy. AJR Am J Roentgenol. 2006;186:883–887.
- Hormann M, Puig S, Prokesch SR, et al. MR imaging of the normal appendix in children. Eur Radiol. 2002;12:2313–2316.
- Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Trends in ambulatory and emergency room visits for inflammatory bowel diseases in the United States: 1994-2005. Am J Gastroenterol. 2010;105:363-370.
- Loftus EV Jr, Schoenfeld P, Sandborn WJ. The epidemiology and natural history of Crohn’s disease in population-based patient cohorts from North America: A systematic review. Aliment Pharmacol Ther. 2002;16:51-60.
- Tolan DJ, Greenhalgh R, Zealley IA, et al. MR enterographic manifestations of small bowel Crohn disease. Radiographics. 2010;30:367-384.
- Leyendecker JR, Bloomfeld RS, DiSantis DJ, et al. MR enterography in the management of patients with Crohn disease. Radiographics. 2009;29:1827-1846.
- Broder JC, Tkacz JN, Anderson SW, et al. Ileal pouch-anal anastomosis surgery: Imaging and intervention for post-operative complications. Radiographics. 2010;30:221-233.
- Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: Comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009;251:751-761.
- Fuchs Y, Markowitz J, Weinstein T, et al. Pediatric inflammatory bowel disease and imaging-related radiation: Are we increasing the likelihood of malignancy? J Pediatr Gastroenterol Nutr. 2011;52:280-285.
- Pariente B, Peyrin-Biroulet L, Cohen L, et al. Gastroenterology review and perspective: The role of cross-sectional imaging in evaluating bowel damage in Crohn disease. Am J Roentgenol. 2011;197:42-49.
Related Articles
Citation
Current applications of MRI in emergent gastrointestinal diseases. Appl Radiol.
November 7, 2012