CT of suspected appendicitis in adults: Current status
Images











Dr. Katz is Vice Chair of the Department of Radiology, Winthrop-University Hospital and Professor of Clinical Radiology, SUNY at Stony Brook. Dr. Belfi is a second-year Radiology Resident and Dr. Weston is an Attending Gastroenterologist, Winthrop-University Hospital, Mineola, NY.
Conflict of interest disclaimer: No specific CT vendor is mentioned in this article. The authors have no actual, potential, or apparent conflicts of interest regarding the material covered in this article.
Portions of the material covered in this article have been previously presented at the American Roentgen Ray Society 103rd Annual Meeting, May 4-9, 2003, San Diego, CA; and the Society of Gastrointestinal Radiologists Annual Meeting, March 7-12, 2004, Scottsdale, AZ, but this material has
Acute appendicitis represents the most common specific identifiable cause of an acute abdomen worldwide. There is an estimated 7% lifetime incidence of appendicitis in the United States, with more than 250,000 appendectomies performed each year. Accurate diagnosis of acute appendicitis is often difficult clinically. The classic triad of right lower quadrant abdominal pain (most typically beginning in the umbilical region and then migrating to the right lower quadrant), fever, and leukocytosis may be absent and may also be secondary to a wide variety of other processes. 1-3 Accurate clinical diagnosis is particularly challenging in older individuals. The negative appendectomy rate (NAR) in women of child-bearing age who do not undergo preoperative imaging is upward of 40% to 45%. 3
This article will: 1) review the rationale for routine computed tomographic (CT) imaging of adult patients with suspected appendicitis; 2) explain the advantages and disadvantages of various CT protocols; 3) review the CT findings of appendicitis and normal appendices; 4) review the controversies regarding techniques; and 5) describe the complications of appendicitis.
Rationale for routine use of CT in adults with suspected appendicitis
There is continuing controversy in the surgical/clinical literature regarding which adult patients with suspected appendicitis should undergo CT scanning versus initial surgical exploration. The historically accepted trade-off between a NAR of up to 20% and an increased perforation rate in patients without definitive appendicitis who are clinically observed has recently been challenged. 1,4 Since 1997, increased attention has focused on the routine use of CT in clinical practice, as more accurate diagnosis and prompt surgery, when indicated, have decreased the complication rate associated with appendicitis. Additionally, alternative diagnoses may be suggested or established using CT. In contrast to a 20% NAR cited above, the overall accuracy of CT ranges from 93% to 98% in most major published series. 5-8 In a retrospective series of 650 patients who underwent CT of the abdomen and pelvis with oral and intravenous (IV) contrast, a 98% accuracy rate was achieved. 5 In a study of 146 patients who underwent CT, the NAR was reduced to 4% and the perforation rate was 22%. 9 In another study, the NAR was reduced to 7% and the perforation rate was only 14%. 10 When one examines the cost-effectiveness of utilization of CT versus direct surgical exploration, the cost of a negative appendectomy has been found to be many times that of a CT scan. 11 In one study that involved 100 consecutive patients, routine CT changed management in 59% of patients, with a cost savings of $447 per patient. 6
Rationale for routine CT: Controversy in the clinical literature
Several studies published in the surgical/clinical literature in the past several years concluded that the use of CT did not improve the diagnosis and treatment of acute appendicitis in adults. 12-14 However, the conclusions of these studies are seriously fiawed. Specifically, only a small percentage of patients actually had a CT scan, 12 there was absence of published information on CT usage, 13 or there was lack of analysis of the impact of CT on the patients who did not undergo appendectomy but who had an alternate diagnosis established. 14
However, the majority of recent studies in the literature stress the correlation of CT findings with patient examination by a surgeon, with the brunt of the data supporting routine CT use. 15-20 In a randomized trial in which 65 patients with suspected appendicitis underwent CT were compared with 63 patients managed using clinical judgment alone, management changed in 26% in the former group. Based on these findings, the authors recommended CT for all patients with suspected appendicitis. 17 In another prospective study involving >100 patients, emergency-department physicians and surgeons recorded their respective management plans for each patient before and after CT (discharge, admit/ observe, or operate). The emergency-department physician plan changed in 35% of patients, and the attending surgeon's plan changed in 27%, with 20 more patients than originally planned undergoing surgery following CT. An alternate diagnosis was made on CT in 20%. 19
There have, however, been some recent dissenting clinical papers. 21-23 In one study of 110 patients, CT was only 89% accurate, and the authors recommended it only if clinical findings were equivocal. 21 In a larger randomized study of 182 patients, 90% accuracy was observed in both the group who underwent CT and the group who did not. The time to the operating room was shorter in the non-CT group, however. 23
Many questions regarding the routine use of CT for suspected appendicitis remain: Specifically, in terms of the reproducibility of the much more accurate results published in the radiology literature in the community, whether and when women of child-bearing age should undergo initial sonography and/or magnetic resonance imaging instead of CT, and the paradox of initial CT triage despite the call in the surgical literature for careful surgical evaluation of all patients. Additionally, the responsibility with the routine use of CT is transferred to the radiologist, along with potential liability, and if read as equivocal, the workup before definitive diagnosis may be prolonged. However, based on our own experience as well as our review of the literature, we favor the routine use of CT in adults with suspected appendicitis.
CT protocols: Overview
The more recent CT literature supports the use of thin-section imaging of the entire abdomen and pelvis, rather than just CT "focused" on the right lower quadrant, and cine review of the images at a monitor or workstation. There is a learning curve involved, regardless of the CT protocol, if one is initially interpreting CT scans for suspected appendicitis. It is important to attempt to identify the cecum, terminal ileum, and appendix on every CT scan, regardless of the protocol used. The choice of a specific protocol may depend on the expertise and preference of the radiologist and that of the ordering physician as well as the need for an urgent answer, the patient's body habitus, and any contraindications to contrast. However, in general, most practices now routinely use oral and IV contrast for most-if not all-patients.
The accuracy of CT is improved significantly when 5-mm as opposed to 10-mm images are performed in the same group of patients. 24 Currently, we reconstruct and review thinner (2 to 3 mm) images from a multidetector CT data set if the appendix is difficult to identify or evaluate on initial 5-mm images. We have found this to be particularly helpful in a subset of patients.
In a landmark study by Balthazar et al, 25 100 patients with clinically equivocal appendicitis underwent CT with oral and IV contrast. The authors stressed the importance of ileal opacification with oral contrast, the use of CT as a road map for surgical planning, and the use of CT for establishing alternative diagnoses (in 17 of 31 patients without a CT diagnosis of appendicitis). They also described the subtle findings of early appendicitis, including only slight appendiceal distension and wall thickening. 25 An appendicolith may or may not be present/identifiable. All of these principles remain very important to date.
Oral and IV contrast
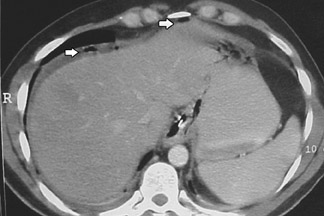
In the original series by Balthazar et al, 25 800 mL of oral barium, given at least 1 hour prior to CT, achieved an accuracy rate of 93%. The abnormal appendix was usually fiuid-filled and revealed an enhancing and slightly thickened wall (Figure 1). There were often associated infiammatory changes in the adjacent fat, and associated fiuid collections or abscesses were seen in cases with more advanced disease. In 2002, the vast majority of U.S. radiology practices always or usually used both oral and IV contrast for imaging patients with suspected appendicitis. 26 We suspect that this percentage has further increased in the last 3 years.
The advantages of routine IV contrast use include identification of earlier disease, easier identification of the appendix (especially in thin patients or patients with little fat in the right lower quadrant region), and potentially better characterization of nonappendiceal disease. Disadvantages include the additional time required for patients to drink oral contrast (and the potential unpleasantness for patients who may already be nauseous), slightly increased cost, and the small risk of a reaction to IV contrast.
Rectal and/or oral contrast only
In 1997, Rao et al published accuracy rates of 98% for CT with oral and rectal contrast 27 and then with rectal contrast only. 28 Up to 1 L of 3% water-soluble iodinated contrast was given rectally via a small-bore catheter immediately prior to scanning without additional patient preparation. A 15-cm-long "focused" region was then scanned centered above the cecal tip (based on the scout digital radiograph). The appendix was considered normal if the lumen filled completely with bowel contrast, air, or a combination of both, and the wall was ≤2 mm in thickness, regardless of maximum diameter. 27 Advantages of this technique include speed, decreased cost, and reduction in overall radiation dose. Disadvantages include the potential unpleasantness of routine rectal contrast use from the viewpoint of patients, technologists, and radiologists (contrast leaked externally in 24% of patients in one series 29 ), and the risk of missing pathology outside the right lower quadrant (ie, alternative diagnoses 30 ) or appendicitis itself (2 of 51 cases in another series 31 ).
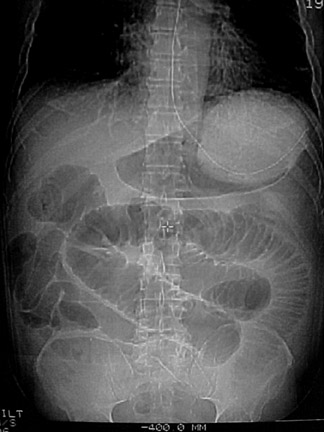
As of 2002, only 1% of residency radiology programs and 8% of private radiology practices in the United States responding to a survey were always or usually using rectal contrast on their patients with suspected appendicitis. 26 Although a recent article also showed very good results with "focused" CT scans obtained with rectal contrast only, 32 we are not aware of many practices currently using this protocol routinely. Oral contrast alone has been studied to a much more limited extent, but in one series a 96% accuracy rate was achieved (Figure 2). 33
Noncontrast CT
CT without oral, rectal, or IV contrast (ie, nonenhanced or noncontrast) was first attempted by a community hospital radiology group led by Malone et al 34 in 1993. In their series of 211 patients, 93% accuracy was achieved using this protocol. Similar or higher accuracy rates were obtained in subsequent series. 7,11,16 In a study of 300 patients published by Lane et al, 7 a 97% accuracy rate was achieved and 63 (21%) alternative diagnoses were correctly established prospectively.
The advantages of noncontrast CT include speed, decreased cost (as contrast is not given), elimination of the risk of an IV contrast reaction, and the ability to monitor the scan remotely without having to supervise IV contrast administration. Disadvantages include a steeper learning curve, difficulty in interpretation in thin patients, and a higher false-negative rate for earlier cases. 16,31,35
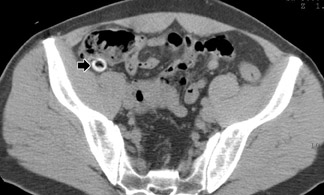
More recent investigations have yielded lower accuracy rates for noncontrast CT for suspected acute appendicitis-78% (in 199 patients imaged at a community hospital 36 ) and approximately 90% (in 95 patients imaged with both low-dose and standard-dose CT 37 ). Additionally, as of 2002, only 2% of radiology residency programs and 12% of private radiology practices always or usually used unenhanced CT. 26 However, since unenhanced CT is the test of choice for suspected renal colic, and because appendicitis and right renal colic may mimic each other clinically, 7 radiologists should be familiar with the appearance of the normal and abnormal appendix on unenhanced CT (Figure 3).
CT protocols: Comparisons
Raptopoulos et al 35 compared 2 cohorts of 50 consecutive patients who underwent CT (with oral and IV contrast) prior to appendectomy in 1997 and 2000. During that time, the use of CT for suspected appendicitis increased by 79%. In the second group, there were less severe imaging findings, including absence of periappendiceal stranding, with a corresponding decrease in pathological severity of appendiceal disease. 35 Jacobs et al 31 imaged 228 patients initially using oral contrast only with "focused" right lower-quadrant CT followed immediately by a CT of the entire abdomen and pelvis with IV contrast. Three radiologists all had higher sensitivity for detection of appendicitis with the second protocol, and increased confidence for alternative diagnoses. Of the 51 patients with appendicitis as the final diagnosis, 22% had no periappendiceal changes, which led to more false-negative diagnoses with the first protocol. The diagnosis of appendicitis was established in some of these cases based on abnormal enhancement of the appendiceal wall. 31 These studies suggest that because patients are being scanned earlier and with less stringent selection, IV contrast should be routinely administered.
CT findings of normal and abnormal appendices
The goal of CT interpretation is to identify the appendix and to characterize it as normal or abnormal. This can be surprisingly difficult in a minority of cases, even with optimized technique. The appendix arises from the medial cecal wall, approximately 3 cm below the ileocecal valve, although the location of the tip is variable (Figure 4). 1 The percentage of cases in which a normal appendix is identified increases with the routine use of thin sections, and the highest reported identification rates have been noted with rectal contrast. 27-28 Pitfalls include: Misinterpretation of a transversely lying ileocolic vessel as an appendix; missed identification of the appendix because of a low-lying cecum; and mistaken identification of an isolated appendicolith as a sign of appendicitis. In a recent series of 366 consecutive patients with possible appendicitis who underwent CT with oral and IV contrast using a slice thickness of 5 mm, the appendix could not be identified retrospectively in 46 (13%) patients, but only 1 of these patients proved to have appendicitis. 38
When determining if appendicitis is present, all of the CT findings should be integrated in making this determination. Size alone cannot be used as a criterion for appendicitis, as pointed out in the initial work of Balthazar et al. 25 The mean transverse diameter of the normal appendix is as high as 7 to 8 mm on noncontrast CT. 39,40 The individual wall of the appendix is usually "pencil thin," 1 regardless of the CT protocol used. Intraluminal gas is seen within the lumen of 75% of identifiable appendices on noncontrast CT, but may be present in >25% of cases of proven appendicitis. 41 In a series of rectal contrast CT cases, gas was present in the lumen in 57% of normal appendices, versus 19% in infiamed appendices. 42 An appendicolith (Figure 5) may be present in up to 10% of normal appendices on noncontrast CT 40 and in 47% of positive cases on noncontrast CT. 7 In some cases, oral contrast may obscure identification of an appendicolith. Review of the images using bone windows may be helpful. 43 Misinterpreting periappendiceal infiammatory changes secondary to a process centered outside the appendix-particularly infiammatory bowel disease-is another potential pitfall.
Perforated appendicitis
Perforation is common in elderly patients who often have atypical presentations, but it may be seen at any age. 3 Although still somewhat controversial, there is consensus in the literature that it is the delay in initial diagnosis, rather than the waiting time in the emergency department or the radiology department, that increases the perforation rate. Additionally, when the CT and clinical findings are initially equivocal for appendicitis, repeat imaging of the right lower quadrant can be performed. Multiple series have shown that intensive observation does not increase appendiceal perforation rates significantly. 3 Accurate diagnosis of perforated appendicitis may be difficult in some cases, as the CT findings may be confused with other disease processes. Identifying residual portions of the appendix, and particularly an appendicolith, adds specificity. To the authors' knowledge, there have not yet been any large series conducted on perforated appendicitis on CT, although smaller series have been published. 44-46 CT findings include phlegmonous changes or an abscess in the right lower quadrant, secondary changes involving the terminal ileum and cecum, a break in the enhancement of the appendiceal wall, extraluminal gas or extraluminal appendicolith, and associated small-bowel obstruction or other findings consistent with peritonitis (Figures 6 and 7). 44,45
Alternative diagnoses
Regardless of the specific protocol used, many alternate diagnoses have been suggested or established in the recent literature using CT for imaging adults with suspected acute appendicitis (Figures 8 and 9). The percentage of alternative diagnoses ultimately made ranges from slightly greater than 25% to 35% of all patients imaged. 7,16,27,33 This has a major impact on the management of patients, as they can be triaged to the appropriate therapy and specialist.
Conclusion
Although there is some continuing controversy in the surgical and clinical literature, a consensus is emerging regarding the utility of routine CT for most, if not all, adult patients with suspected acute appendicitis. Increasing evidence suggests that even young adult men should routinely undergo CT rather than initial surgical exploration, and there is no convincing evidence-based data that the routine use of CT increases the perforation rate. CT, regardless of the protocol used, permits diagnosis or exclusion of appendicitis and alternative diagnoses accurately compared with the historical 20% negative appendectomy rate. Furthermore, CT establishes the severity of appendicitis. The paradox is that the increased use of CT may have made accurate diagnosis more difficult in some patients, especially those in the earlier stages of appendicitis. Because patients are being scanned earlier, and because findings may therefore be more subtle or false-negative on unenhanced CT or on CT with oral/rectal contrast only, IV contrast should be considered routinely for imaging all patients with suspected appendicitis. Thin cuts, cine review of images on a monitor, and careful review of the right lower quadrant anatomy, as well as routine scanning of the entire abdomen and pelvis, should be performed in all cases. Radiologists need to appreciate the overlap of normal and abnormal appendiceal sizes, and should use all the CT findings present to make or exclude the diagnosis of appendicitis.