Stent Grafting for Traumatic Arterial Injuries


Stent grafting, either bare or covered, for traumatic arterial injuries has been increasing as surgeons become more familiar with interventional radiology-assisted procedures as an alternative or adjunct to open surgical repair.
In their review of the National Trauma Data Bank, Reuben, et al, found that the use of endovascular intervention for arterial trauma grew from 2.1% of all cases in 1994 to 8.1% in 2003, with an accompanying increase in the use of stents.1 In the appropriate setting, stent grafting can reduce operative times, blood loss, hospital mortality, incidence of sepsis, and hospital length of stay as well as limit surgical dissection in a traumatized operative field.2
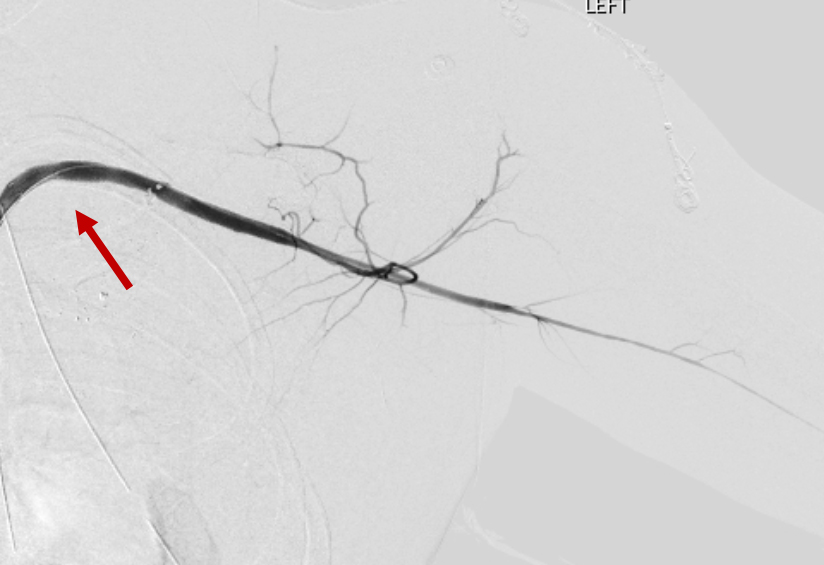
More than half (55%) of vascular injuries result from blunt mechanisms, while 45% are secondary to penetrating trauma. The most frequently injured blood vessels in blunt trauma cases include the iliac, internal carotid, and brachial arteries. The most frequently injured blood vessels in penetrating trauma cases are the brachial and superficial femoral arteries.1 Successful management of traumatic injuries to the carotid, femoral, axillary, subclavian, and iliac arteries, as well as the thoracic aorta, great vessels, and the abdominal aorta has been documented (Figure 1).
Ideal candidates for arterial stent grafting are more stable than those treated with open surgical repair, have fewer head and other associated injuries, and have higher Glasgow Coma Scores.1 In addition, patients with low-velocity injuries in an anatomic region more vulnerable to ischemia or bleeding complications, or to regions with a high-risk of iatrogenic nerve injury, such as the subclavian and carotid arteries, are also more favorable for arterial stent grafting.2 Injuries that require surgical debridement may not benefit significantly from stenting. While stenting may not be able to provide definitive treatment in all trauma situations, it can still serve as a bridge to open procedures by controlling hemorrhage or damage, thereby facilitating surgical repair.
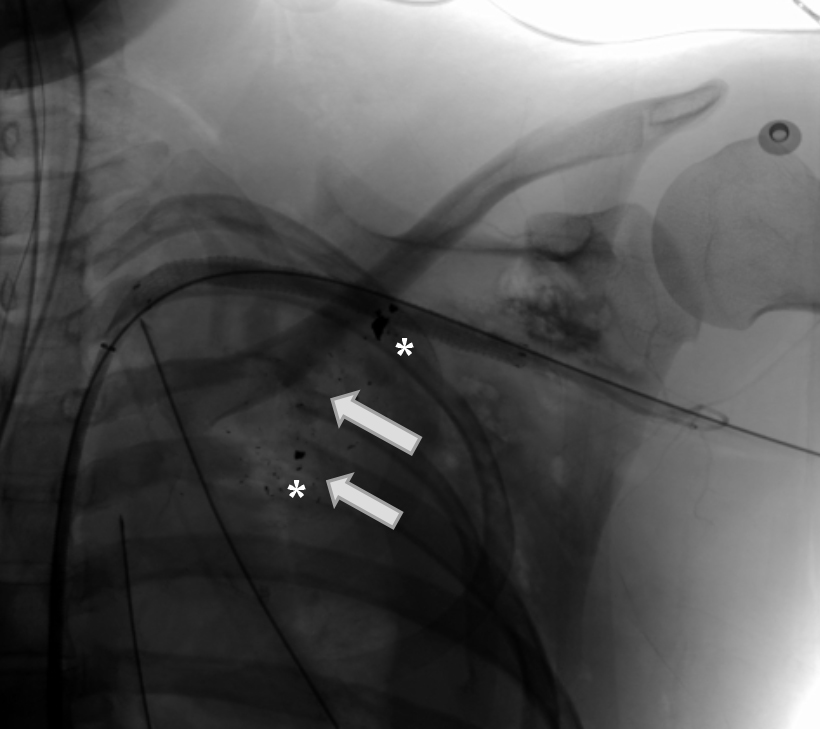
Open surgical repair of ruptured abdominal aortic aneurysms (AAAs) has been giving way to growing use of stenting in these cases, owing to stenting’s lower 4-year mortality rate and lower pulmonary, renal, and bleeding complication rates.3 The technical success rates of endovascular treatment of supradiaphragmatic arterial injury are as high as 96.7% with only a 6.4% complication rate.4 In thoracic aortic trauma, stenting can avoid thoracotomy-associated complications, aortic cross clamping, related ischemic events, and extracorporeal bypass.1
In a review of the Pubmed and OVID Medline databases, DuBose, et al, identified 113 patients over a 19-year period treated with stenting for carotid artery injury. Stenting was most commonly used after blunt injuries, the most common being pseudoaneurysm, followed by arteriovenous fistula, dissection, partial transection, occlusion, intimal flap, and aneurysm. The authors found an initial success rate of 76.1% and a patency rate of 79.6%, with radiographic and clinical follow-up periods ranging from two weeks to two years. There were no reported stent-related mortalities and only 3.5% of patients reported new neurologic deficits.5 Carotid artery stenting is of more value in Zone 1 or 3 injuries of the neck, where injury exposure and identification are more technically difficult.
Stent grafting can be particularly advantageous to surgeons faced with injury to difficult anatomic regions, such as the axillary artery, where the risk of iatrogenic trauma to neurovascular bundles and other surrounding structures is high.
DuBose, et al, also reviewed the Pubmed and OVID Medline databases for stenting of subclavian and axillary injuries. They identified 160 patients during a 22-year period treated with stents following penetrating or blunt trauma, iatrogenic catheter-related injury, and surgical injury. The specific injuries included pseudoaneurysm, arteriovenous fistula, occlusion, transection, perforation, dissection, and others not specified. The authors found a 69.6% initial placement success rate and a patency rate of 84.4% during radiographic and clinical follow-up ranging from hospital discharge to 70 months. No mortalities were reported and only one of the 160 patients reported new neurological deficits. 6
In regard to the lower extremities, the popliteal and iliac arteries are ideal candidates for stenting, owing to their challenging accessibility for surgeons. Furthermore, iliac-artery intervention reduces the risk of retroperitoneal hematoma and iatrogenic damage to the ureter and underlying iliac veins better compared with open surgery.2 There have been case reports of superficial femoral artery (SFA) stenting; however, the SFA is easily accessible with surgical exposure, making endovascular management less beneficial. Nevertheless, there may be some benefit in situations of concomitant orthopedic injuries, where hardware compromises surgical exposure.1 There are also case reports of the arteries of the lower leg, including the posterior tibial arteries, being treated with carotid stents to maintain patency in cases of ischemia in the setting of tibial fracture and orthopedic hardware.7
Contraindications
Several contraindications to arterial stenting should be considered. One is the inability to cross a lesion with a wire; interventional embolization may be of value in these circumstances.2 Other relative contraindications include infection, uncontrolled hemorrhage, and hemodynamic instability.
Also important to consider when determining if stenting is a viable option include availability of an interventional suite or a hybrid operating room, as well as proximity of the OR should emergent surgical assistance be required. Other considerations: the facility’s inventory and equipment, including, but not limited to, stents, exchange length wires, sheaths, balloons, power injectors, and digital subtraction capabilities. All these factors, along with other institutional specific factors, must be addressed beforehand to prevent unnecessary treatment delays.2
Follow-up protocols
The appropriate period for post-procedural follow-up and ongoing surveillance for complications such as stent migration, endoleaks, and stenosis has not been well studied or established. As most trauma patients are typically younger, with a lower incidence of atherosclerotic disease, stent placement is not typically seen in this population.
Conclusion
Many studies have reported the technical success rate of arterial stenting and its potential morbidity and mortality benefits over traditional surgical repair. However, most are limited to case reports and series and retrospective reviews, and long-term data is lacking. Larger and longer-term studies and randomized controlled trials are needed to further define the role of arterial stenting for traumatic injuries.
References
- Reuben BC, Whitten MG, Sarfati M, Kraiss LW. Increasing use of endovascular therapy in acute arterial injuries: analysis of the National Trauma Data Bank. J Vasc Surg. 2007; 46:1222–1226.
- Johnson CA. Endovascular management of peripheral vascular trauma. Semin Intervent Radiol. 2010;27(1):38-43.
- Greco G, Egorova N, Anderson PL, Gelijns A, Moskowitz A, Nowygrod R, Arons R, McKinsey J, Morrissey NJ, Kent KC. Outcomes of endovascular treatment of ruptured abdominal aortic aneurysms. J Vasc Surg. 2006 Mar;43(3):453-459.
- Hershberger RC, Aulivola B, Murphy M, Luchette FA. Endovascular grafts for treatment of traumatic injury to the aortic arch and great vessels. J Trauma. 2009 Sep;67(3):660-71.
- DuBose J, Recinos G, Teixeira PG, Inaba K, Demetriades D. Endovascular stenting for the treatment of traumatic internal carotid injuries: expanding experience. J Trauma. 2008 Dec;65(6):1561-6.
- DuBose JJ, Rajani R, Gilani R, Arthurs ZA, Morrison JJ, Clouse WD, Rasmussen TE; Endovascular Skills for Trauma and Resuscitative Surgery Working Group. Endovascular management of axillo-subclavian arterial injury: a review of published experience. Injury. 2012 Nov;43(11):1785-92.
- du Toit D F, Coolen D, Lambrechts A, de V Odendaal J, Warren B L. The endovascular management of penetrating carotid artery injuries: long-term follow-up. Eur J Vasc Endovasc Surg. 2009; 38:267–272.
