Labyrinthine ossificans
By Larson C, Jorgensen SA, Towbin, AJ, Towbin R
CASE SUMMARY
A 6-year-old girl presented with a 3- to 6-month history of sensorineural hearing loss. Previous hearing exams were normal.
IMAGING FINDINGS
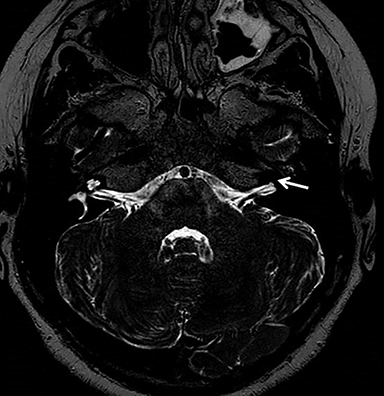
A high-resolution, axial MR T2-weighted image through the internal auditory canals (IACs) (Figure 1) demonstrated normal appearance of the right IAC, cochlea and partially visualized the vestibule/lateral semicircular canal. The left IAC was normal in appearance; however, the cochlear aperture was blind-ending and the normal inner ear structures were not identified.
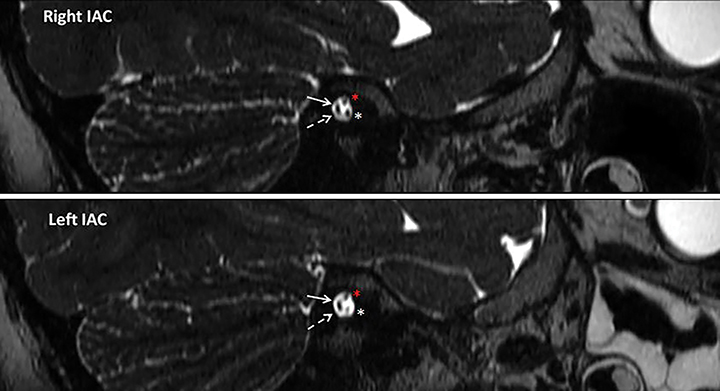
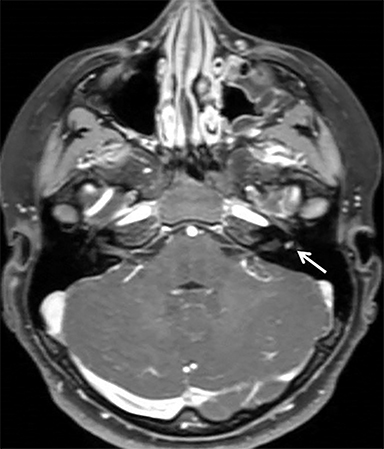
High-resolution, sagittal MR T2-weighted images through the left IAC and right IAC (Figure 2) revealed normal facial nerves, cochlear nerves, superior vestibular nerves and inferior vestibular nerves bilaterally. An axial MR T1-weighted post-contrast image through bilateral IACs (Figure 3) showed a small focus of enhancement in the area of the left vestibule, likely representing granulation tissue.
DIAGNOSIS
Labyrinthine ossificans. The differential diagnosis also includes labyrinthine aplasia, cochlear aplasia, and cochlear otosclerosis.
DISCUSSION
Labyrinthine ossificans (LO) is a condition in which the normal membranous labyrinth becomes replaced by fibrous and/or osseous tissue. A three-stage classification has been proposed for labyrinthitis: acute inflammatory, fibroblastic, and eventual osseous formation. LO consists of the fibrous and osseous stages.1 Spread of intracranial infection to the membranous labyrinth is the most common etiology of labyrinthitis/LO, with other routes of infection including contiguous spread from the auditory canal and hematogenous. Less common etiologies include trauma, tumor, prior surgery, vascular, inflammatory, and hematologic disorders.1,2 When LO is associated with bacterial meningitis, bilateral inner ear involvement is common.1 Patients most often present with sensorineural hearing loss of the affected side.
Temporal bone CT and MR with high-resolution, T2-weighted imaging of the middle ear are considered complementary in diagnosis and evaluation of LO. CT findings include ossification within the middle ear structures, including the membranous labyrinth, semicircular canals and vestibule. MR imaging is considered more sensitive than CT for LO and can reveal replacement of the normal fluid-filled, T2 hyperintense structures of the inner ear with intermediate and low signal.3 Eventual atrophy of the cochlear nerve can be seen in severe cases. With MRI, initial changes of fibrosis can be seen earlier than with CT. Post-contrast T1-weighted imaging can show enhancement of inner ear with active labyrinthitis, the precursor to LO.
Treatment of hearing loss attributed to labyrinthine ossificans is typically cochlear implantation; however, the success of this procedure is determined by the extent of the inner ear obliteration. Ossific changes of LO have been documented as early as 4 weeks following infectious insult; thus, timely diagnosis and intervention is recommended to increase success rates of surgery.3 It is important for the interpreting radiologist to comment on cochlear involvement as this may preclude success with cochlear implantation.4 Nevertheless, newer “drill-out” cochlear implant surgical techniques as well as auditory brainstem implantation have shown success in those with complete cochlear ossification.4,5
CONCLUSION
LO is due to chronic fibrosis/ossification of the membranous labyrinth as a result of infectious/inflammatory/traumatic insult, most commonly spread from bacterial meningitis. Patients typically present with sensorineural hearing loss on the affected side. These destructive changes can present as early as 4 weeks following initial insult.
CT and MR imaging are considered complementary in diagnosis of LO, although MR is more sensitive for detecting early fibrous changes in the membranous labyrinth. The interpreting radiologist plays a vital role in early recognition of these changes and detailed description of the involved structures can help guide surgical therapy and improve patient outcomes.
REFERENCES
- Booth TN, Roland P, Kutz JW, Lee K, Isaacson B. High-resolution 3-D T2-weighted imaging in the diagnosis of labyrinthitis ossificans: emphasis on subtle cochlear involvement. Pediatr Radiol. 2013; 43(12):1584-1590.
- Becker TS, Eisenberg LS, Luxford WM, House WF. Labyrinthine ossification secondary to childhood bacterial meningitis: implications for cochlear implant surgery. AJNR Am J Neuroradiol. 1984; 5(6):739-741.
- Coelho DH, Roland JT. Implanting obstructed and malformed cochleae. Otolaryngol Clin North Am. 2012; 45(1):91-110.
- Harnsberger HR, Dart DJ, Parkin JL, Smoker WR, Osborn AG. Cochlear implant candidates: assessment with CT and MR imaging. Radiology. 1987; 164(1):53-57.
- Grayeli AB, Bouccara D, Kalamarides M, et al. Auditory brainstem implant in bilateral and completely ossified cochleae. Otol Neurotol. 2003; 24(1):79-82.
