High Quality Imaging with Reduced Dose


Roundtable Participants: Dianna M. E. Bardo, MD, Associate Professor of Diagnostic Radiology, Oregon Health and Science University, Portland, OR; Kate Feinstein, MD, Associate Professor of Radiology, Section Chief, Pediatric Radiology, Comer Children’s Hospital, The University of Chicago, Chicago, IL; Harvey S. Hecht, MD, FACC, Director of Cardiovascular Computed Tomography, Lenox Hill Heart and Vascular Institute of New York, New York, NY; Paul Schoenhagen, MD, staff physician, Department of Diagnostic Radiology and Cardiovascular Medicine, Cleveland Clinic, Cleveland, OH; Claudio M. Smuclovisky, MD, Director of South Florida Medical Imaging Cardiovascular Institute, Boca Raton, FL; Chip Truwit, MD, Professor and Chief of Radiology, Hennepin County Medical Center and Hennepin Faculty Associates, Minneapolis, MN; Michael W. Vannier, MD, Professor of Radiology, University of Chicago Medical Center, Chicago, IL; Charles White, MD, Director of Thoracic Imaging, University of Maryland Medical Center, Baltimore, MD
As efforts to reduce radiation dose gain momentum, a change in thinking within the radiology profession is necessary. Particularly, acceptance must be gained in order to convince radiologists that modifying the protocols they have used for years will still yield acceptable images. A significant benefit is coming from the growing range of advancements on the CT scanner to improve image quality at lower doses and to reconstruct more data from scans that use less radiation. Some targets remain a challenge, but with faster acquisition times, many of the traditional limitations are being overcome. When CT protocols are set across an institution, they must be set respective of each unique scanner.
“You have to tailor the protocols, and you have to work with the community of radiologists to make sure that they understand the rationale for dose reduction. It becomes a joint effort and hopefully a mutually beneficial effort,”said Charles White, MD, Director of Thoracic Imaging, University of Maryland Medical Center, Baltimore, MD. “The goal is to produce consistent scans to the greatest extent possible with whatever scanner is used for a patient’s examination. So, this requires a good deal of technical knowledge and skill.”
The task of achieving consensus across an entire group of radiologists can seem daunting, but the end result is to achieve diagnostic quality images with the most responsible use of radiation.
“As doctors, we are diagnosticians, and our ultimate goal should be to provide accurate diagnosis with the least amount of radiation to the patient,” said Claudio M. Smuclovisky, MD, Director of South Florida Medical Imaging Cardiovascular Institute, Boca Raton, FL. “We are always measuring our risk/benefit ratio, which depends on the complexity of the clinical problem and the age of the patient. In cardiovascular imaging, you are only as good as the quality of the image.”
Additionally, protocols must be adjusted based on scanner type. At the University of Chicago Medical Center, scanners are used from 16 slices through 256 slices.
“Achieving dose reductions on each type of scanner and maintaining the overall quality with the sheer number of protocols that are involved is always a challenge,” said Michael W.Vannier, MD, Professor of Radiology, University of Chicago Medical Center, Chicago, IL. “When you compound that with the fact that there are so many technologists and the fact that dose reduction technologies have basically blossomed in the last couple of years, the bigger challenge is informing and training this large group of individuals, who are crucial to optimal scanning.”
Objective measures of image quality
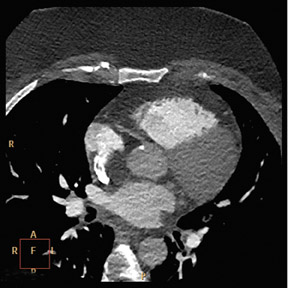
The “quality” of any image is subject to a wide range of definitions, and even in CT where there are strictly applied measures of quality, as defined by the ACR Panel for Accreditation, there is still a subjective analysis made by radiologists as to what constitutes a high-quality image. CT images are generally judged on the presence of noise, the slice thickness (e.g., the Z-axis resolution), and the high- and low-contrast resolution. In cardiac imaging, the measure of image quality revolves around contrast density (the maximum density of contrast opacification in the coronary arteries), and it is measured in Hounsfield units (HU), generally no less than 300 HU in the proximal coronaries. Cardiac imaging also is susceptible to motion artifact and the entire study is reviewed alongside the electrocardiogram (ECG).
“At the end of the day, the measure of image quality is determined by the noise in a study, and each physician sets his or her own barometer for an acceptable study,” said Chip Truwit, MD, Professor and Chief of Radiology, Hennepin County Medical Center and Hennepin Faculty Associates, Minneapolis, MN.
Imaging applications and exam optimization
Part of the ability to optimize any type of medical imaging is to choose the right modality for the right patient. For instance, a patient with a very high or irregular heart rate who very urgently needs an assessment of coronary anatomy might not be the best candidate for CT and instead should potentially be imaged with traditional cardiac catheterization. In younger patients, magnetic resonance imaging (MRI) or ultrasound may be better imaging choices for an initial assessment.
“In many instances, we discuss exams with referring physicians to determine if another exam would work just as well without radiation,” said Kate Feinstein, MD, Associate Professor of Radiology, Section Chief, Pediatric Radiology, Comer Children’s Hospital, The University of Chicago, Chicago, IL. “ For example, if a patient has right lower quadrant pain, we try to perform ultrasound to look for appendicitis.”
It is necessary to involve the referring physicians and ensure that they are educated about the role of each medical imaging tool.
“At the Cleveland Clinic, we employ a multimodality imaging model where a group of physicians, who are collectively knowledgeable about all imaging modalities and their limitations and advantages, direct patients to the optimal imaging modality in the right clinic setting,” said Paul Schoenhagen, MD, Staff Physician, Department of Diagnostic Radiology and Cardiovascular Medicine, Cleveland Clinic, Cleveland, OH.
Cardiacimaging
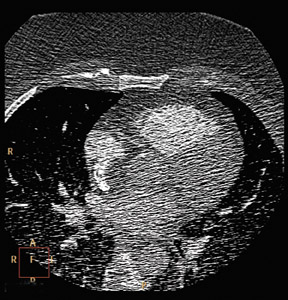
In cardiovascular work, the challenge between lowering dose and increasing quality is amplified because the imaging targets are small structures that move rapidly, according to Harvey S. Hecht, MD, FACC, Director of Cardiovascular Computed Tomography, Lenox Hill Heart and Vascular Institute of New York, New York, NY.
“There is no substitute for an excellent study,” said Dr. Hecht. “The biggest improvement in moving to the Brilliance iCT has been our ability to perform high quality prospective step-and-shoot images. We do that whenever possible, and I would say probably 85% of our cases are step-and-shoot.”
Other solutions to obtain high quality cardiac images, according to Dr. Hecht, are:
- Ensure the patient has an adequate heart rate — the lower the better.
- For retrospective imaging, obtain as many phases as possible and spend the appropriate amount of time to ensure that every phase is covered sufficiently to obtain excellent images from each of the coronary arteries.
- For step-and-shoot with prospective imaging, the choices are more limited. For instance, if a study is acquired of 75% of a cardiac phase, there is an option to reconstruct the phases at either 76% to 77%, or 73% to 74%, giving the same dose reduction from the prospective acquisition, yet providing more leeway in interpretation.
Pregnantpatients
When imaging pregnant patients through the thorax for suspicion of pulmonary embolism, clinicians must be mindful of both the patient and the fetus.
“Besides CT, one of your options is to do a ventilation/perfusion (V/Q) scan, but there are pros and cons to each of those options,” said Dr.White.“ Because of the expanded blood volume in pregnant patients, there is a hemodilution effect, and you run the risk of getting a nondiagnostic CT scan. In later stages of pregnancy, as the fetus moves higher up in the pelvis, there are times where we will opt towards other modalities. However, if CT is really the best way to address a life threatening issue, we will use it.”
At the University of Maryland Medical Center, these patients are counseled whenever possible and are asked to review and acknowledge their informed consent. The treatment decision is not a simple procedure. If more individuals are involved in these decisions, it lessens the likelihood of choosing an inappropriate examination, according to Dr.White. “ These decisions are handled at a much higher level of scrutiny, and they are made with great care. You also don’t want to take a chance making the dose so low that you acquire nondiagnostic images. This is one of the most challenging and difficult problems that we face with CT dose.”
Metal artifact reduction
Part of the appeal of CT imaging is that patient selection is not as restrictive as with MRI, that it provides higher anatomical detail than ultrasound, and produces excellent spatial and temporal resolution. While implantable devices may rule a patient out of MRI entirely, those patients could potentially be imaged on CT, although there had traditionally been challenges with the attenuation artifact.
“Metal implants are a big problem in the revascularized heart, where patients may have implants or multiple surgical clips,” said Dr. Smuclovisky.
In these cases, studies that employ iDose4 can be performed with less radiation and can reduce the amount of artifact from the implantable devices, thus improving image quality. The iDose4 approach is beneficial when imaging stents, however, surgical clips on bypass grafts can still lead to uninterpretable segments. The same issues occur when imaging patients with spinal implants and other fixation devices. The newly released Ingenuity CT addresses these clinical scenarios and complements the benefits provided by iDose4 with a novel metal artifact reduction algorithm incorporated into the reconstruction subsystem.
“This is one area for which the slice wars actually did provide answers,” said Dr.Truwit.“ When you go from 4 slices to 16 slices to 64 slices and now we’re at 256 slices, the degree of artifact drops dramatically when you go to these thinner slice scanners and this is built into the scanner.”
Conclusion
While there are technological improvements that can contribute to reduced radiation dose, one of the major advancements will be the effects of better ordering habits. These habits will be a result of better education for referring physicians. Additionally, increased utilization of the electronic medical record — with the ability to track a patient’s prior history of CT examinations — will provide a more informed picture to referring physicians. Finally, the industry is actively developing automated decision support tools that will help referring physicians understand the alternative imaging options that are available.
“In our hospital, the trauma center and the emergency room dictate the rules because half the patients come in through the emergency department,” said Dr. Truwit. “One of the benefits of an electronic health record is that information is immediately available that the patient may have had 3 prior CT studies in the past 10 days. While each individual admission stands on its own, you have to figure out if there is a better way of doing things for the patient who is back with abdominal pain for the fourth time over the last 6 weeks.”
Using these types of automated and electronic tools could help reduce the real problem that plagues CT: finding a way to increase the data about a patient’s procedure history so as to avoid excessive repeat scans.
“The real problem is not a single study, whether it is delivered at 1 mSv or 20 mSv,” said Dr. Smuclovisky.“ The problem is when patients receive multiple studies. If we really want to save patients from significant amounts of radiation, receiving multiple studies is where they get the lion’s share. Using tools that help us track this information can help us make more informed decisions and will ultimately benefit the patient.”
