Going beyond ALARA: Let’s keep contrast “ASARA”
By S Conway
We diagnostic radiologists often discuss how we can minimize ionizing radiation exposure to our patients by applying the ALARA Principle, which we all know stands for the concept of making ionizing radiation dose As Low As Reasonably Achievable whenever and wherever feasible.
Indeed, all imaging studies that utilize ionizing radiation (such as computed tomography) should be performed while keeping in mind those memorable and historically lengthy radiation physics classes we all endured during our radiology residency programs.
Yet, as we remind ourselves to incorporate those ALARA teachings into our daily practice, we should also be equally mindful about keeping contrast media volumes as low as possible.
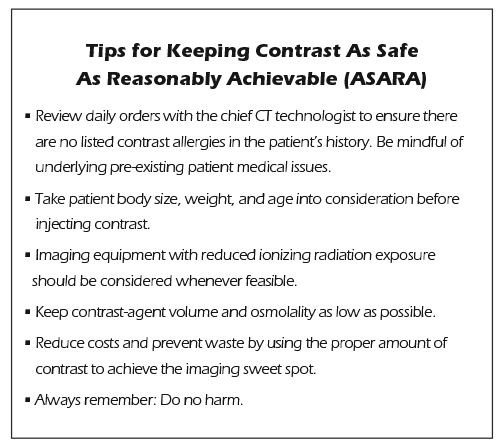
Indeed, I would go so far as to encourage us all to keep in mind the twin concept, if you will, of the “ASARA Principle—“ the idea that we should strive to keep intravenous contrast media dosages As Safe As Reasonably Achievable, wherever and whenever we can, for the safety of our patients.
Toward this end, I recommend the following measures:
- Technologists should utilize the lowest levels of both ionizing radiation and contrast media injection possible while achieving what I call the imaging “sweet spot” for an individual patient study. By providing an optimized and individualized patient dose at each CT visit, patient safety will be achieved, and radiologists and CT technologists will be satisfied in knowing that only the appropriate amount of contrast has been administered to each patient. The result will be optimal for the patient, and the best images will allow our diagnostic radiologists to make an accurate and highly specific diagnosis.
- The safest osmolality should be utilized for each examination. Ideally, low-osmolar or iso-osmolar agents in low volumes should be used, particularly in patients at risk for contrast-induced nephropathy (CIN).1
- Special considerations and accommodations should always be made for patients of different sizes, shapes, and weights, including our pediatric population.
- >When reviewing our daily schedule of patients, we radiologists must ensure that a contrast injection is warranted and is safe for a particular patient. Checking orders in the morning with the chief CT technologist is always a good idea. Ideally, the safest amount of contrast used in a given patient is the lowest dose possible to achieve a specific diagnosis. If no contrast is needed to make the diagnosis, or if the patient will not tolerate contrast due to severe allergies (despite premedication), none should be used; alternatively, a different imaging study should be considered. These decisions require careful review of patient histories, and thoughtful decision making on the part of the diagnostic radiologist in charge of the CT section. This is where the diagnostic radiologist must rely upon the art and science of medicine. The exam should always be performed with the right amount of contrast for the right patient at the right (and preferably the lowest) radiation exposure level.
In addition to their safety and quality benefits, these measures will have the side benefits of saving money and preventing the waste of unused contrast media in the CT suite. Indeed, in light of our new healthcare landscape, it is of paramount importance for physicians to be mindful of preserving quality and safety for patients, and creating more optimized methods when it comes to administering contrast media. In addition, cost-containment measures in this new healthcare landscape are important in this era of value-based care.
During a busy and hectic day at the hospital, it may be easy to let safety measures like these slip past. However, if we are consistently mindful about preventing harm to the patient and reducing both ionizing radiation exposure and contrast media exposure, we will arrive at better practices for our patients.
Reference
- Katsiki N, et al. Contrast-induced nephropathy: An “all or none “phenomenon? Angiology. 2015 Jul;66(6):508-513.
