Discrepancies Found Among 5.9 Million Radiological Examinations
 A new study shows that imaging practice leaders should carefully consider efforts to match interpretation of subspecialty examinations with radiologists’ fellowship training in the acute community setting. The study, titled “Interpretations of Examinations Outside of Radiologists’ Fellowship Training: Assessment of Discrepancy Rates Among 5.9 Million Examinations From a National Teleradiology Databank,” was published in ARRS’ American Journal of Roentgenology (AJR).
A new study shows that imaging practice leaders should carefully consider efforts to match interpretation of subspecialty examinations with radiologists’ fellowship training in the acute community setting. The study, titled “Interpretations of Examinations Outside of Radiologists’ Fellowship Training: Assessment of Discrepancy Rates Among 5.9 Million Examinations From a National Teleradiology Databank,” was published in ARRS’ American Journal of Roentgenology (AJR).
Pointing out that major and minor discrepancy rates were not higher for acute community setting examinations outside of interpreting radiologists’ fellowship training, “discrepancy rates increased for advanced examinations,” acknowledged lead investigators Suzanne Chong from Indiana University in Indianapolis and Tarek Hanna of Emory University in Atlanta.
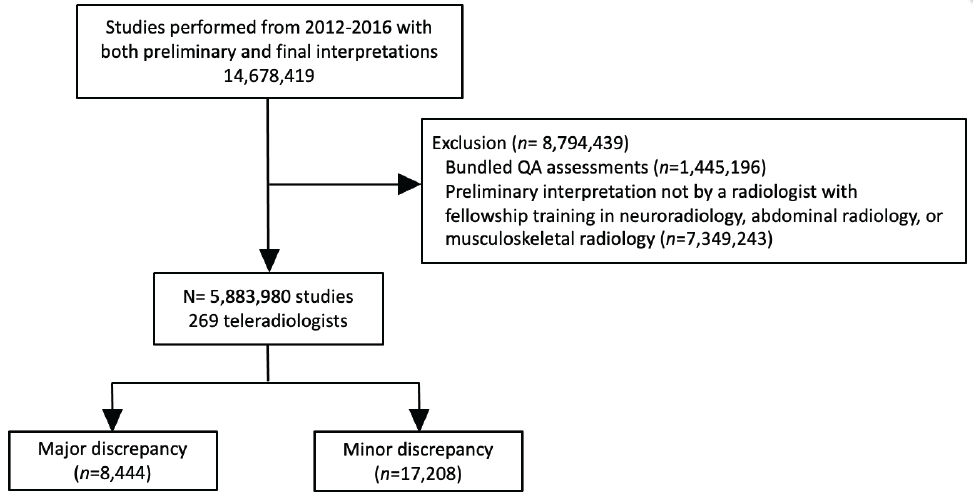
Using the databank of Virtual Radiologic, a large US teleradiology company, Chong, Hanna and colleagues’ analysis included 5,883,980 acute examinations performed from 2012 to 2016 that were preliminarily interpreted by 269 teleradiologists with a fellowship of neuroradiology, abdominal radiology, or musculoskeletal radiology. When providing final interpretations, client on-site radiologists voluntarily submitted quality assurance (QA) requests if preliminary and final interpretations were discrepant; the teleradiology company’s own QA committee categorized discrepancies as major (n=8,444) or minor (n=17,208).
Among the preliminary teleradiology interpretations of acute community setting examinations, common examinations’ major and minor discrepancies rates were not different when concordant versus discordant with radiologists’ fellowship training (p>.05). However, advanced examinations’ discrepancy rates were higher when concordant with radiologists’ fellowship (relative risk = 1.45 and 1.17, respectively; p<.05).
Noting that their findings support multispecialty radiologist practice in acute community settings, “efforts to match examination and interpreting radiologist subspecialty may not reduce diagnostic discrepancies,” the authors of this AJR article added.
