Currarino syndrome and the effect of a large anterior sacral meningocele on distal colostogram in an anorectal malformation
By Lee JK, Towbin RB, Towbin AJ
CASE SUMMARY
A 2-year-old boy with a history of a complex anorectal malformation (ARM) consisting of a rectourethral fistula and a large anterior sacral meningocele was initially treated with a double-barrel colostomy at another institution. He was referred to our facility for simultaneous definitive colorectal and neurosurgical repair. Prior to surgical intervention, imaging of the gastrointestinal tract, genitourinary tract and spine was performed.
IMAGING FINDINGS
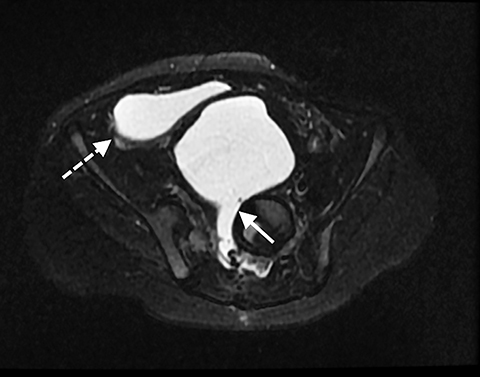
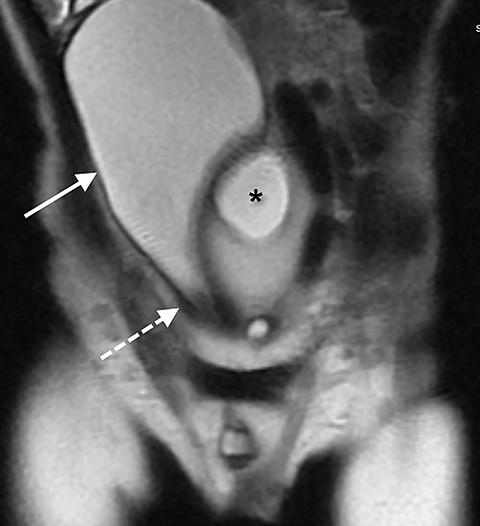
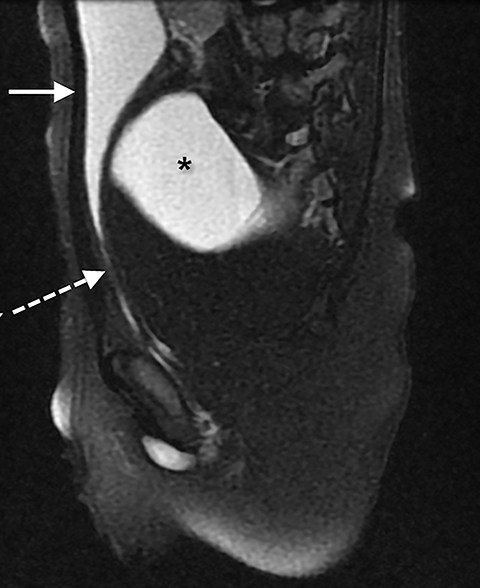
An MR scan of the pelvis was first performed (Figures 1-3), utilizing the following sequences: coronal T1, coronal 3D proton density, axial and sagittal T2 with and without fat saturation, direct coronal T2, and a coronal T2 oblique to the plane of the rectum. The images from this study showed a large anterior sacral meningocele displacing the bladder anteriorly, superiorly, and towards the right side of the pelvis. The bladder appeared vertical and its neck elongated. As typical on MRI, the fistula was not visible. In this case, the large meningocele and distorted bladder made visualization impossible.
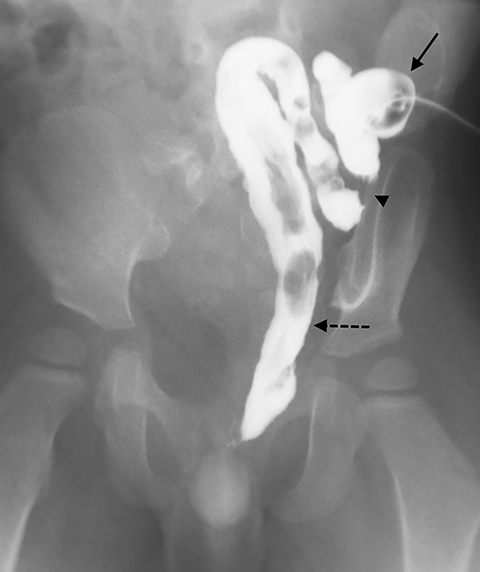
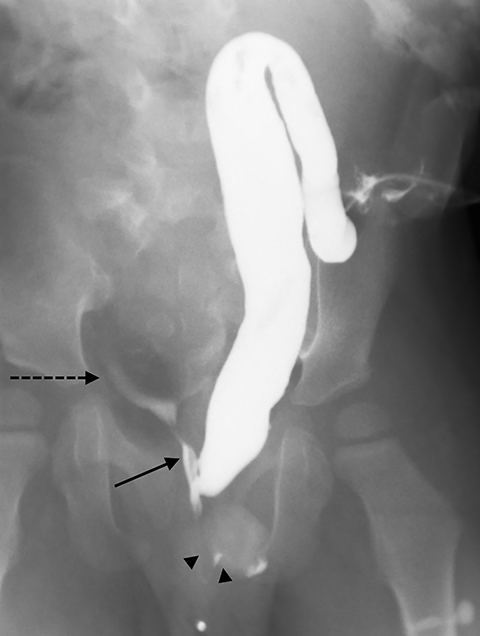
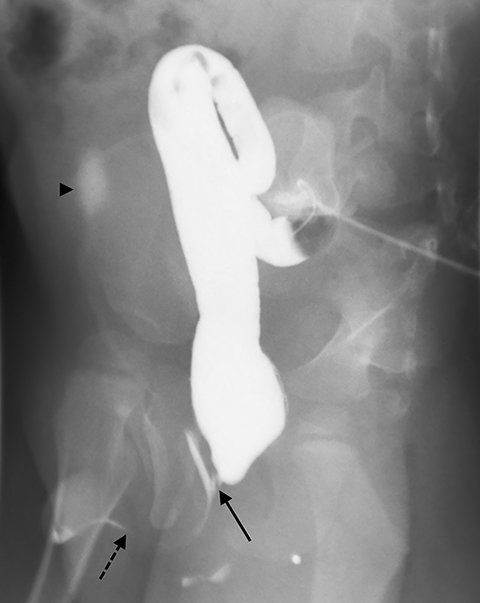
One day later, the patient underwent a high-pressure distal colostogram. To perform this procedure, an 8-Fr Foley catheter was inserted into the ostomy of the distal colon and the balloon was inflated with 2 ml of air just beneath the skin surface to prevent leakage. With the patient supine, the catheter was injected with 60 mL of water-soluble contrast (Figure 4). The initial images showed a long segment of distal colon traversing the ostomy to the rectum. Approximately 2 cm from the ostomy site, the colon folded back upon itself. This fold made it impossible to generate the pressure required to distend the distal rectum; therefore, the Foley catheter was advanced so that the tip was beyond the fold (Figure 5). Contrast was again injected through the catheter and the rectum was successfully distended.
The patient was then moved to the left lateral decubitus position to best reveal the rectourinary fistula. With continued pressure, a small, linear area of contrast was seen overlying the pubic symphysis. To fully visualize the fistula, the patient was placed into a right posterior oblique position, which showed a rectourethral fistula. As contrast was injected, a small amount began to pool over the right iliac crest in the region of the urinary bladder (Figure 6).
Several days later, the patient underwent cystoscopy, a posterior sagittal anorectoplasty for a rectoprostatic urethral fistula, and placement of a suprapubic catheter. At the time of repair, a large anterior meningocele, which was partially repaired several months earlier, was noted to still be large enough to compress the descending colon and rectum toward the left and to displace the bladder superiorly and anteriorly. A significant amount of fibrotic tissue was encountered at the time of dissection and the anatomy was clearly abnormal due to the presence of anterior meningocele.
DISCUSSION
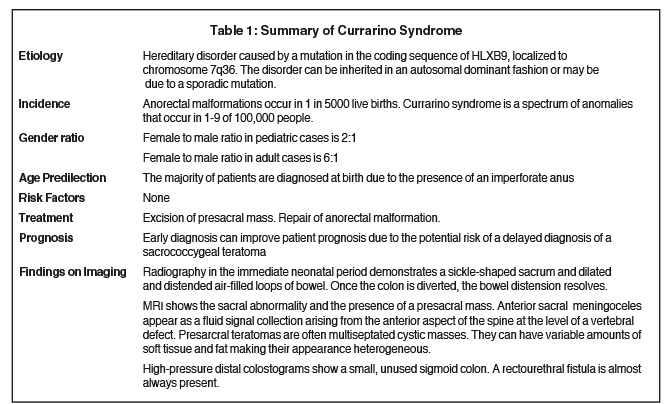
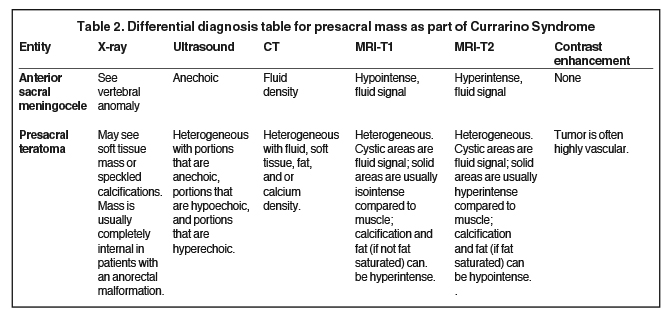
Anorectal malformations are congenital anomalies that occur in approximately 1 in 5000 live births and range in severity from anal stenosis or imperforate anus to complex deformities such as cloacal exstrophy.1 Risk factors for an ARM include genetic predisposition, prenatal exposure to nicotine, alcohol, caffeine, or illicit drugs, maternal obesity and maternal diabetes mellitus.2 Children with an ARM may also present with other associated anomalies. The Currarino syndrome is a triad of anomalies consisting of an ARM, sacral defect, and presacral mass.3 It occurs in approximately 1 in 100,000 people.4 Anterior sacral meningoceles are the most common presacral mass in patients with Currarino syndrome, occurring in 60% of patients; and its presence may affect the surgical management of these patients.5,6 Other potential presacral masses include a presacral teratoma or an enteric cyst.
Palliative surgery is initially performed in an infant born with an ARM to divert the colon and allow the patient to mature before definitive surgery.1 The initial palliative surgery of an imperforate anus includes a colostomy to allow enteric contents to evacuate while an additional stoma is created for the distal colon.1
Patients with an underlying diagnosis of ARM must undergo multiple radiologic examinations prior to definitive repair. These include abdominal radiography to evaluate for masses and vertebral anomalies, abdominal and pelvic ultrasound to evaluate for urological abnormalities, fluoroscopic imaging of the genitourinary tract to evaluate the bladder and urethra, and MRI of the abdomen, pelvis, and spine to evaluate the complexity of the malformation and pelvic musculature. A high-pressure distal colostogram (HPDC) is also performed to determine if a fistulous tract from the rectum to either the bladder or urethra is present. While there is one report of MRI being used to define the fistula,7 we do not believe this technique allows for adequate distention of the rectum or fistula. In one study, the lack of an HPDC led to misdiagnoses and an insufficient repair, requiring reoperation.8 Once all imaging is obtained and the anatomy is appropriately defined, a roadmap and clinical decision can be made for an appropriate surgical plan.
In this patient, the presence of a large anterior sacral meningocele altering the bladder anatomy affected performance of the HPDC. Normally, when this procedure is performed, the patient is placed in a true lateral position to optimally demonstrate the recto-urinary fistula. This allows the radiologist to determine if the fistula connects with the bladder or the urethra. Because of this patient’s altered anatomy, the fistula could not be demonstrated with the patient in the true lateral position. However, when the patient was placed in the right posterior oblique position, the fistula was most apparent.
When performing an HPDC, the rectum must be completely distended so that it appears rounded in its most distal portion. This helps to open the distal fistula. In our patient, the long segment of distal colon with a proximal fold made it difficult to generate the pressure needed to distend the rectum until the catheter was advanced beyond the proximal fold. Once the catheter was beyond this point, and the rectum was distended, the fistula began to opacify. The second factor that made it difficult to identify the fistula in this patient was the large meningocele distending and distorting the bladder. Typically, when the bladder is at midline, the rectovesicular or rectourethral fistula is seen extending anteriorly from the rectum. Imaging the patient in the left lateral decubitus position helps to best display the fistula. In our patient, the anterior meningocele displaced the bladder anteriorly, laterally, and superiorly. This made it impossible to view the entire fistula in the left lateral decubitus position; instead, the patient was placed in the right posterior oblique position to image the entire fistula.
The major risk of performing an HPDC is bowel perforation. While enough hydrostatic pressure must be created during the distal colostogram to evaluate for the presence of a communicating fistula, the fluoroscopist must be wary of over-distending the colon. Thus, contrast injection should continue until the rectal vault appears rounded in its distal-most portion on the lateral view. If a fistula is not present at this time, the study should be aborted. Typically, the risk of bowel perforation increases with increasing length of the distal colon. Given the length of the distal bowel in this patient, we were aware of the possibility for perforation during the procedure. When contrast began to pool in the right lower quadrant, we were concerned that a small perforation had occurred. Review of the preprocedural MRI, along with rotating the patient, helped to confirm that the pool of contrast was within the bladder and caused by the rectourethral fistula.
The MRI scan was used to help define the altered anatomy. It showed the anterior sacral meningocele displacing the bladder anteriorly, laterally, and superiorly distorting the bladder neck and proximal urethra. Once contrast started pooling in the right lower quadrant, knowledge of the appearance and location of the bladder was useful to confirm that the distal colon had not ruptured.
The location of the rectourethral or rectovesicular fistula is crucial for surgical planning. The high-pressure distal colostogram helps to define the patient’s anatomy and provides the colorectal surgeon with a detailed roadmap prior to surgery. This roadmap allows the surgeon to determine if the definitive surgical repair should be performed via intra-abdominal incision or a posterior sagittal anorectal pull-through approach. Although many ARMs can be safely repaired via posterior sagittal approach, in patients with anterior sacral meningoceles, repair of the meningocele is performed first. This helps to prevent meningitis, which can occur when the surgeries are performed simultaneously.3
CONCLUSION
Patients with a Currarino triad present with a spectrum of anomalies, including a sacral defect, a presacral mass, and an anorectal malformation. Pelvic MRI and a high-pressure distal colostogram are often needed to effectively diagnose the condition and care for these patients.
REFERENCES
- Levitt, MA. , and Pena, A. Anorectal malformations. Orphanet J Rare Dis. 2007 Jul 26; 2:33. PMID: 17651510.
- Zwink N, Jenetzky E, Brenner H. Parental risk factors and anorectal malformations: systematic review and meta-analysis. Orphanet J Rare Dis. 2011 May 17; 6:25. PMID: 21586115.
- Lee, SC, Chun, YS, Jung, SE, Park, KW, and Kim, WK. Currarino triad: Anorectal malformation, sacral bony abnormality, and presacral mass—a review of 11 cases. J Pediatr Surg. 1997 Jan; 32(1): 58-61. PMID: 9021570.
- Orphanet Report Series. Prevalence of Rare Diseases: Bibliographic Data 2014 http://www.orpha.net/orphacom/cahiers/docs/GB/Prevalence_of_rare_diseases_by_alphabetical_list.pdf. Accessed February 24, 2015.
- Emans PJ, van Aalst J, van Heurn EL, et al. The Currarino triad: neurosurgical considerations. Neurosurgery. 2006 May; 58(5):924-9.PMID: 16639328.
- Samuel M, Hosie G, Holmes K. Currarino triad-diagnostic dilemma and a combined surgical approach. J Pediatr Surg. 2000; 35(12):1790-4. PMID: 11101738.
- Kavalcova L, Skaba R, Kyncl M, Rouskova B, Prochazka A. The diagnostic value of MRI fistulogram and MRI distal colostogram in patients with anorectal malformations. J Pediatr Surg. 2013 Aug; 48(8):1806-9. PMID: 23932626.
- Peña A, Grasshoff S, Levitt M. Reoperations in anorectal malformations. J Pediatr Surg. 2007;42(2):318-25. PMID: 17270542.
