The Inadvertant Aortopexy




CASE SUMMARY
A 66-year-old male initially presented as a stroke activation for left upper extremity weakness. Medical history was significant for laryngeal squamous cell carcinoma, including prior neck dissection and chemoradiation. In addition, he was fully anticoagulated with IV heparin.
A carotid stenosis was discovered, which was amenable to intravascular stenting by neurointerventional radiology (NIR). General anesthesia was required because the case was classified as a difficult intubation. The primary service and anesthesiologist requested interventional radiology (IR) to place a push-type gastrostomy tube (PEG) at the same sitting so that multiple intubations and extubations could be avoided. Heparin could not be terminated for the PEG tube procedure, owing to the recent stroke and the stent placement.
CLINICAL AND IMAGING FINDINGS
Per standard protocol, the stomach was insufflated and the overlying soft tissues anesthetized with 1% lidocaine.
Under fluoroscopy, a T-fastener needle was advanced, the deflection of the gastric bubble observed, and contrast injected to confirm position.
However, contrast extravasation and blood return from the needle were observed. The needle was withdrawn and a repeat contrast injection confirmed intraluminal location. The T-fastener was deployed. Under fluoroscopy a distortion of the gastric bubble was noted.
The second T-fastener needle was advanced. Fluoroscopy again demonstrated blood return and contrast extravasation. Multiple re-directed attempts were made to gain access into the stomach. When it was judged that an intraluminal location was confirmed, a second T-fastener was deployed. A third was placed in similar fashion.
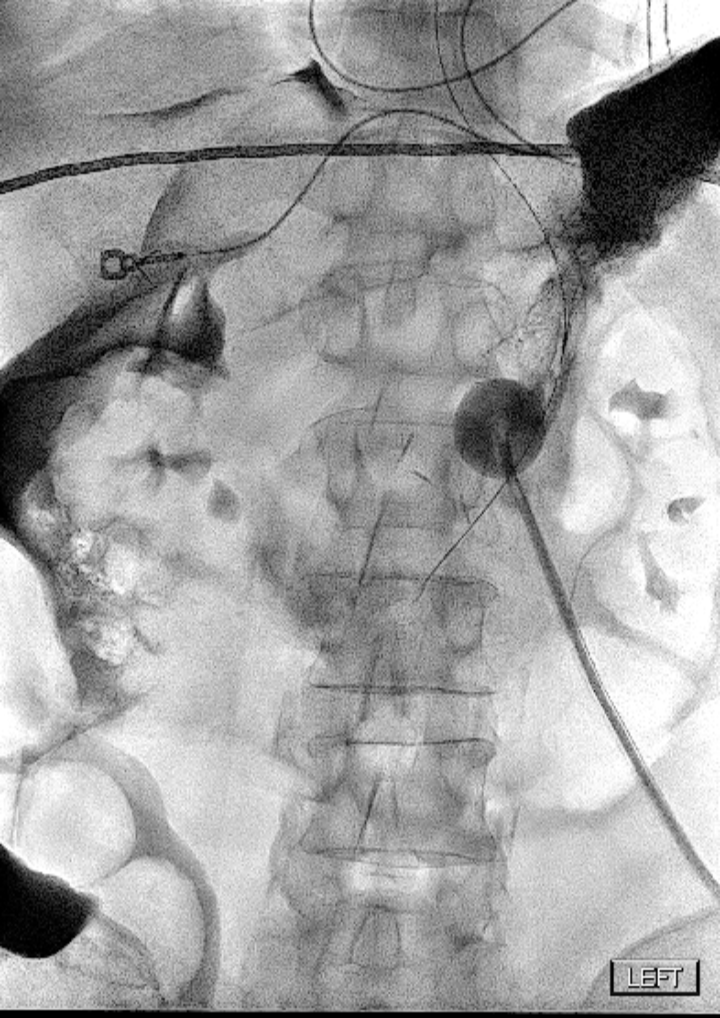
Following dilatation over an Amplatz wire, a 16 Fr, balloon-retained gastrostomy tube was advanced and contrast injected. Gross extravasation of contrast was seen with the presumption that the balloon was inflated anterior to the gastric wall (Figure 1).
A new gastrostomy tube subsequently was placed and contrast imaging confirmed appropriate position with no further extravasation.
At this time, the patient experienced a sudden drop in blood pressure, owing to suspected hemorrhage because the patient was fully anticoagulated and there was known puncture of the posterior wall of the stomach. The patient was immediately transferred from IR to the CT suite for emergent computed tomography angiography (CTA).
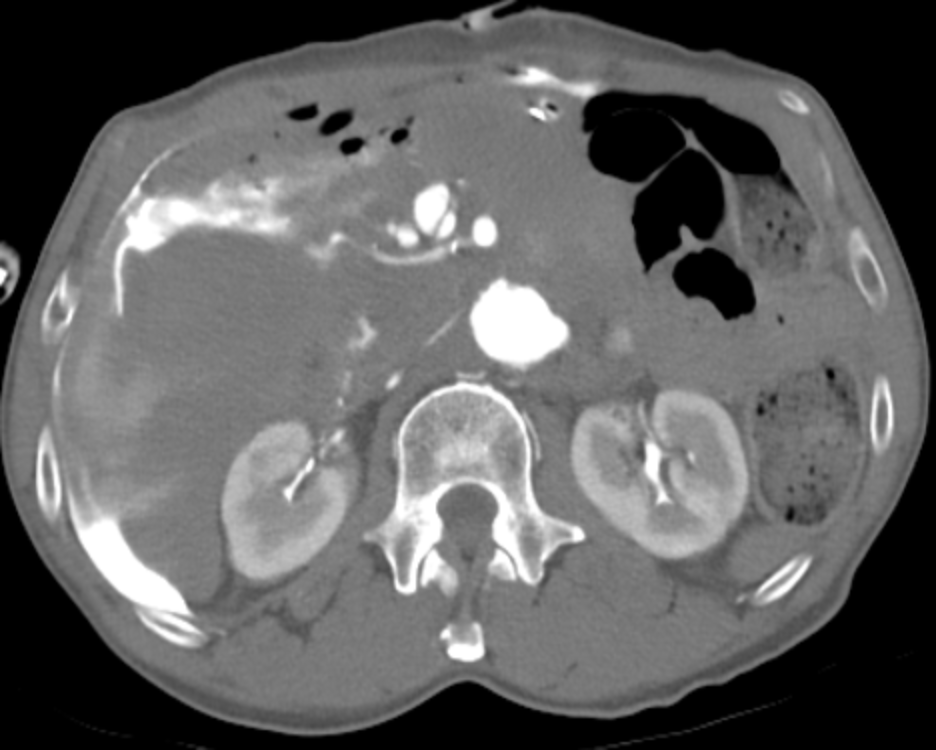
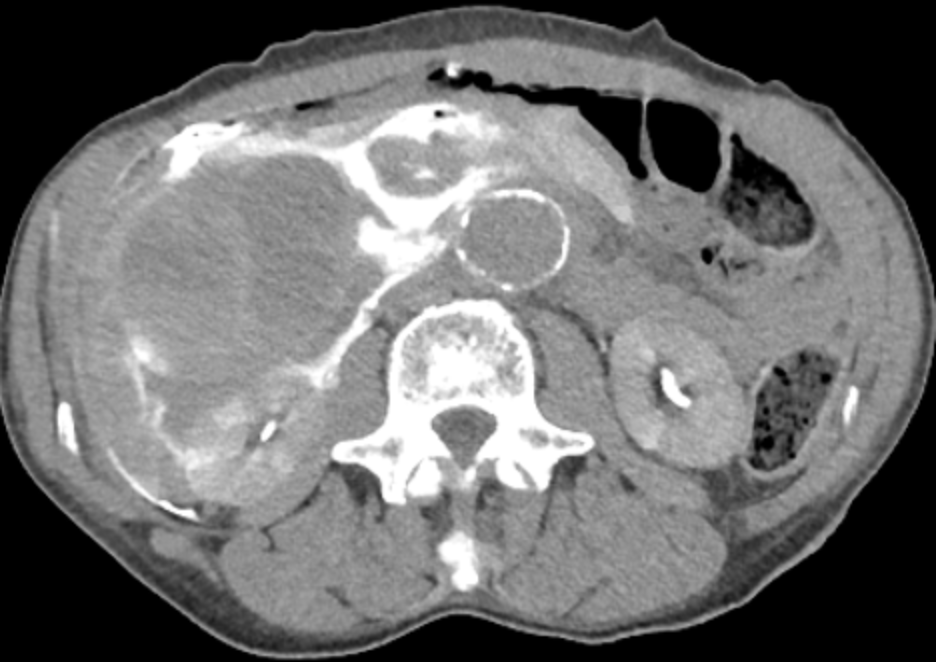
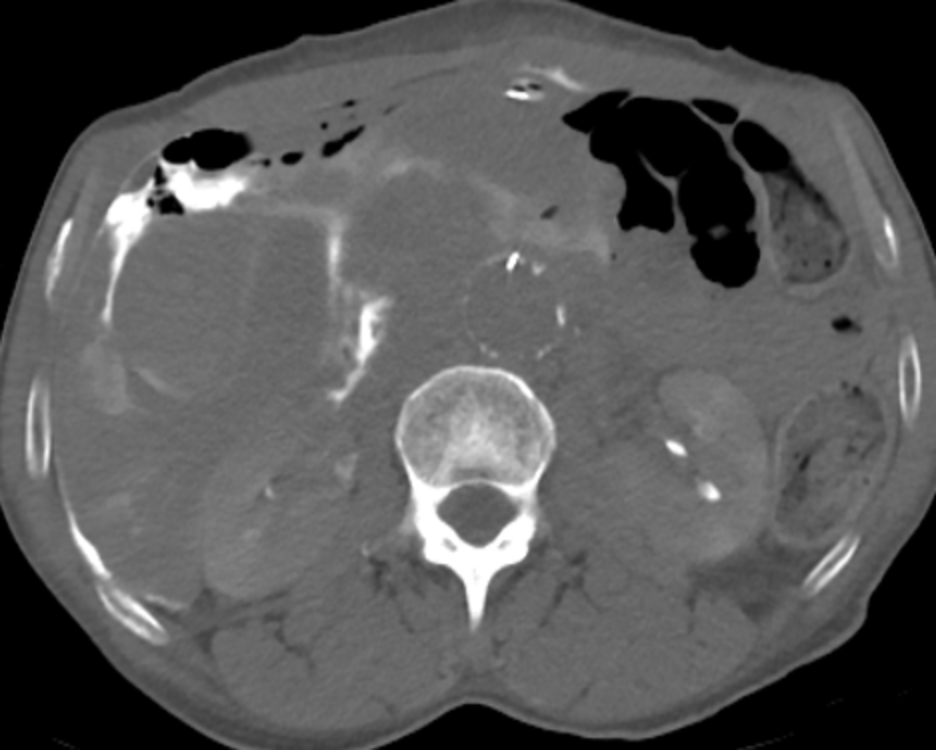
CTA revealed active extravasation from a large, unusually ectatic superior mesenteric artery, which coursed posteriorly to the stomach (Figures 2,3). This was associated with a large hematoma posterior to the stomach.
Also noted was aneurysmal dilatation of the abdominal aorta measuring 3.5 cm in diameter (Figure 4). A T-fastener was seen near, if not within, the aorta itself (Figure 5). The patient was immediately transferred back to IR to the 4D-CT hybrid suite, which was made available for emergent angiogram and embolization.
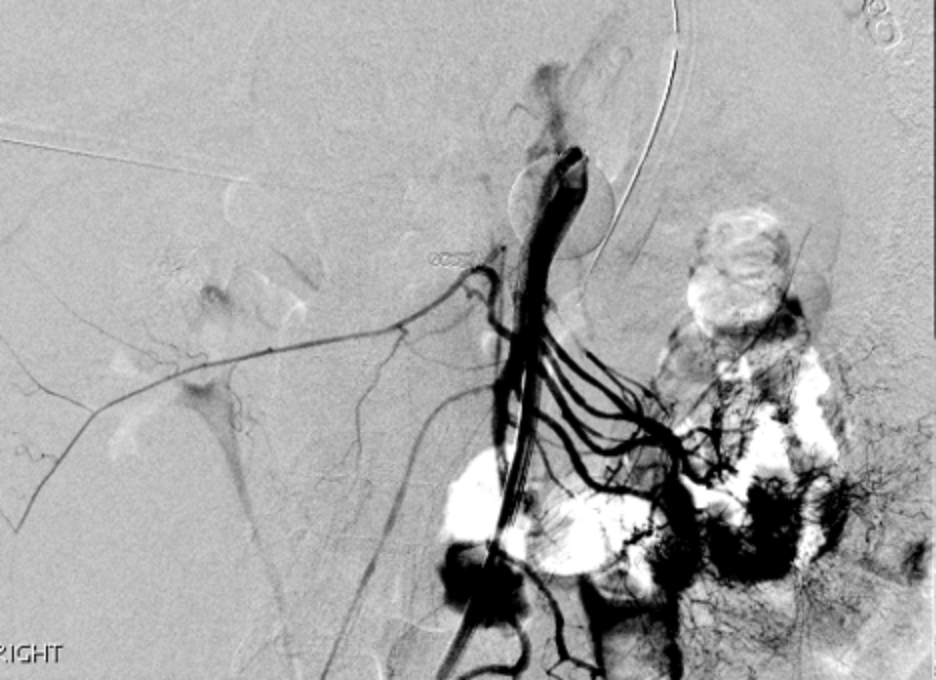
Angiogram revealed gross extravasation from an enlarged middle colic artery (Figure 6). This was successfully embolized with multiple micro-coils (Figure 7).
Repeat angiogram revealed continued extravasation from the proximal-most main descending superior mesenteric artery (Figure 8). A covered stent graft was successfully placed, with repeat angiogram revealing excellent stent positioning with no further extravasation (Figure 9).
The attending anesthesiologist reported immediate improvement in hemodynamic status. The hemodynamically stable patient was transferred to the surgical intensive care unit with no signs of peritonitis.
Although the patient’s clinical status remained stable, the attending surgeon performed exploratory laparotomy the following day, which uncovered neither active bleeding nor gastric perforation. Consistent with the CTA findings, a suture representing part of the T-fastener arose from the aortic aneurysm. The surgeon affixed the string so that the metal portion of the “T” was tethered to the aortic wall and would not embolize. Gastropexy and evacuation of the hematoma were also performed. The patient recovered without further sequelae.
DIAGNOSIS
Vascular injury during PEG placement
DISCUSSION
Surgical gastrostomy, first described in the 1800s,1 remained the principal method of enteral feeding until percutaneous endoscopic gastrostomy was introduced in 1980.2 Subsequently, percutaneous fluoroscopic placement of gastrostomy tubes was proven to be both safe and effective.3
Also well documented are data showing that endoscopic and fluoroscopic placement of gastrostomy tubes have significantly lower complication rates than surgical placement.4-7 Bleeding, in particular, is rare.8-13
Contraindications to percutaneous gastrostomy tube placement include ascites, gastric malignancy, overlying peritoneal metastasis, altered gastric anatomy, and coagulopathy.4
As a result, patient selection plays a critical role in maintaining a low complication rate of percutaneous techniques.14 Herein we encounter the first error in this case.
Regardless of extenuating circumstances---including cases of “difficult intubation” and requests by clinical service and anesthesiologists for both procedures to be performed concomitantly, gastrostomy tube placement is not an emergent procedure. Considering the neurologic requirement for full anticoagulation, the safer route would have been surgical placement.
Nevertheless, the procedure should have been performed in the 4D-CT suite given the patient’s significantly elevated risk of bleeding.
Because the PEG tube was placed in the NIR suite, the patient had to be transported to another suite for the CTA and then returned to an IR suite, resulting in a delay of at least one hour in treatment of the patient, who was now in hemorrhagic shock. Further, had CT and/or CTA not been immediately available, imaging would have been performed after the first puncture of the stomach, when fluoroscopy alone demonstrated an unusual distortion of the gastric bubble.
This distortion represented a developing hematoma, posterior to and compressing the mid-body of the stomach. Had the patient already been in the 4D-CT suite, immediate angiography and intervention could have been performed. Fortunately, the delay in diagnosis and treatment did not result in a worse outcome.
CONCLUSION
This case illustrates both the critical importance of patient selection in percutaneous gastrostomy tube placement, as well as the usefulness of the ability to perform both conventional angiography and CT in the same procedure room.
REFERENCES
- Walker LG. L. L. Staton, M.D., and the first successful gastrostomy in America. Surg Gynecol Obstet. Apr 1984;158(4):387-8.
- Gauderer MW, Ponsky JL, Izant RJ. Gastrostomy without laparotomy: a percutaneous endoscopic technique. 1980. Nutrition. Sep 1998;14(9):736-8. doi:10.1016/s0899-9007(98)00073-2
- Wollman B, D'Agostino HB, Walus-Wigle JR, Easter DW, Beale A. Radiologic, endoscopic, and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology. Dec 1995;197(3):699-704. doi:10.1148/radiology.197.3.7480742
- Silas AM, Pearce LF, Lestina LS, et al. Percutaneous radiologic gastrostomy versus percutaneous endoscopic gastrostomy: a comparison of indications, complications and outcomes in 370 patients. Eur J Radiol. Oct 2005;56(1):84-90. doi:10.1016/j.ejrad.2005.02.007
- Cosentini EP, Sautner T, Gnant M, Winkelbauer F, Teleky B, Jakesz R. Outcomes of surgical, percutaneous endoscopic, and percutaneous radiologic gastrostomies. Arch Surg. Oct 1998;133(10):1076-83. doi:10.1001/archsurg.133.10.1076
- Walton GM. Complications of percutaneous gastrostomy in patients with head and neck cancer--an analysis of 42 consecutive patients. Ann R Coll Surg Engl. Jul 1999;81(4):272-6.
- Möller P, Lindberg CG, Zilling T. Gastrostomy by various techniques: evaluation of indications, outcome, and complications. Scand J Gastroenterol. Oct 1999;34(10):1050-4. doi:10.1080/003655299750025174
- Lee SH, Moon HS, Park JH, et al. Percutaneous endoscopic gastrostomy tube Insertion-induced superior mesenteric artery injury treated with angiography. Korean J Gastroenterol. Dec 2018;72(6):308-312. doi:10.4166/kjg.2018.72.6.308
- Sekmenli T, Gündüz M, Akbulut H, Emiroglu H, Koplay M, Ciftci I. Massive hemorrhage: a late complication of replacement percutaneous endoscopic gastrostomy: case report. Arch Argent Pediatr. Apr 2018;116(2):e315-e318. doi:10.5546/aap.2018.eng.e315
- Lau G, Lai SH. Fatal retroperitoneal haemorrhage: an unusual complication of percutaneous endoscopic gastrostomy. Forensic Sci Int. Feb 2001;116(1):69-75. doi:10.1016/s0379-0738(00)00366-2
- Schurink CA, Tuynman H, Scholten P, et al. Percutaneous endoscopic gastrostomy: complications and suggestions to avoid them. Eur J Gastroenterol Hepatol. Jul 2001;13(7):819-23. doi:10.1097/00042737-200107000-00010
- Chong C, Derigo L, Brown D. Massive gastric bleeding: a rarely seen subacute complication of percutaneous endoscopic gastrostomy. Intern Med J. Nov 2007;37(11):787-8. doi:10.1111/j.1445-5994.2007.01505.x
- Ubogu EE, Zaidat OO. Rectus sheath hematoma complicating percutaneous endoscopic gastrostomy. Surg Laparosc Endosc Percutan Tech. Dec 2002;12(6):430-2. doi:10.1097/00129689-200212000-00008
- Ahmed O, Jilani D, Sheth S, Giger M, Funaki B. Radiologically guided placement of mushroom-retained gastrostomy catheters: Long-term outcomes of use in 300 patients at a single center. Radiology. Aug 2015;276(2):588-96. doi:10.1148/radiol.15141327
