Choroid Plexus Papilloma
By Ballur KN, Towbin RB, Schaefer CM, Morgan D, Towbin AJ



Case Summary
An infant presented with increased head circumference, a bulging anterior fontanelle, and a two-day history of downward gaze. Vital signs were significant for bradycardia with a heart rate of 78 bpm and hypertension with a systolic blood pressure of 161 mmHg. On examination, the pupils were 2 cm dilated and sluggish.
Imaging Findings
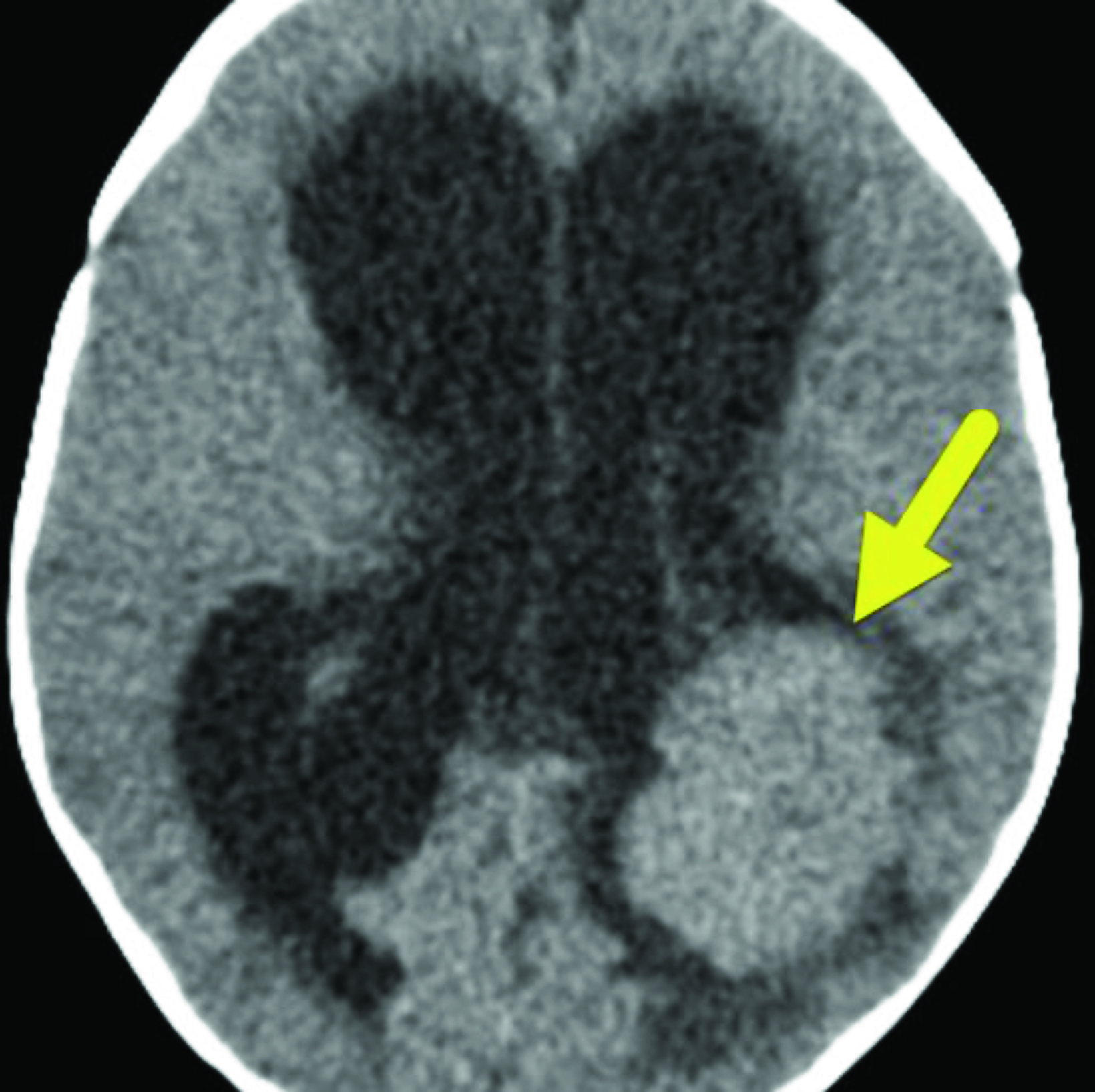
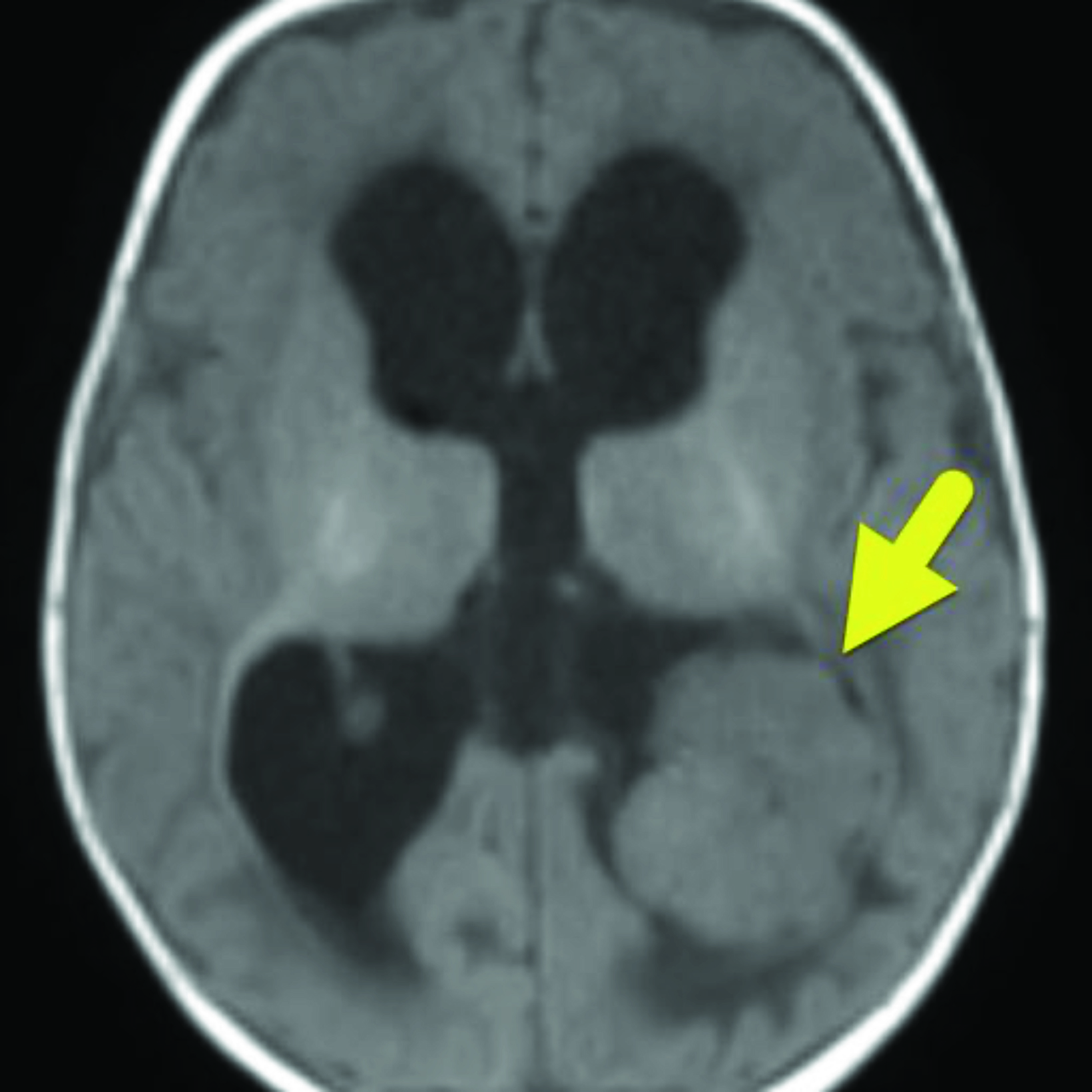
Noncontrast brain CT (Figure 1) showed a 3.2 × 3.7 cm intraventricular mass arising from the choroid plexus in the atrium of the left lateral ventricle. There was moderate hydrocephalus with transependymal CSF flow. Brain MRI (Figure 2) confirmed the intraventricular location of the tumor. On T1 and T2 images, the tumor was isointense with a central vascular pedicle. There was homogeneous contrast enhancement of the tumor. Vasogenic edema was present in the left occipital and posterior temporal lobes.
Diagnosis
Choroid plexus papilloma.
The differential diagnosis includes choroid plexus carcinoma, ependymoma, subependymoma, central neurocytoma, subependymal giant cell astrocytoma, and meningioma.
Discussion
Choroid plexus papillomas (CPPs) are benign tumors that arise from the choroid plexus epithelium.1 They comprise 3% of intra-cranial tumors in the pediatric population, with 48% of patients diagnosed before 10 years and 20% before 1 year.1 In children, CPPs most commonly arise within the lateral ventricles (64%) followed by the fourth (26%) and third ventricles (7%).2 Tumors arising from other locations, such as the cerebellopontine angle, can occur but are rare.2
Patients typically present with signs and symptoms of increased intracranial pressure. These include headache, papilledema, vomiting, cranial nerve deficits, focal deficits, and seizures.3 In infants, increasing head circumference, bulging fontanelle, lethargy, and fussiness are common.1 The increased intracranial pressure is caused by hydrocephalus which results from cerebrospinal fluid (CSF) outflow obstruction and/or CSF overproduction.1
Choroid plexus tumors are classified by the World Health Organization (WHO) according to three grades based on histopathological findings: CPP (grade I); atypical CPP (grade II); and choroid plexus carcinoma (grade 3).4 The atypical CPP was formally defined by the WHO in 2007 and can be histologically differentiated from a standard CPP by its increased cell density, nuclear pleomorphism, increased mitotic activity, and internal necrosis.5
On CT, CPP appears hypodense and lobular.6 Approximately 25% of CPPs have internal calcifications and may appear cystic.3 Owing to their highly vascular nature, the tumors enhance with contrast.3 On MRI, they often appear cauliflower-shaped with an irregular contour and enhance with contrast.3,7 On T1 MRI, CPP appears hypointense or isointense; on T2 images, it appears hyperintense.4
Calcifications appear hypointense, whereas hemorrhage in the tumor may appear hyperintense, depending on its age.3 MR angiography may provide information related to the vascular supply of the tumor, aiding surgical planning.3 While the different types of choroid plexus tumors cannot be distinguished reliably via imaging, features such as large size, indistinct internal morphology, parenchymal invasion, peritumoral edema, and tumor necrosis increase the likelihood of malignancy.8
Patients with CPP typically have good outcomes after total surgical resection, with 5- and 10-year survival rates of 81% and 77%, respectively.3,9 While CPPs are benign, they can recur after resection. Chemotherapy may be considered if the tumor is unresectable, recurs, or disseminates through the CSF.3 Caution should be used in considering radiotherapy for children with CPP owing to the treatment’s long-term consequences.10 Hydrocephalus may persist after surgical resection due to adhesions in the subarachnoid spaces and/or occlusion of arachnoid granulation tissue.7
Conclusion
Choroid plexus papilloma is an uncommon, benign tumor typically found in the lateral ventricles. Diagnostic imaging is vital to identifying and planning surgery for this tumor, as complete surgical resection is the mainstay of treatment.
References
- Kabashi A, Ahmetgjekaj I. Choroid plexus papilloma — case presentation. Curr Health Sci J. 2021;47(2):310-313. doi:10.12865/CHSJ.47.02.24
- Wolff JE, Van Gool SW, Kutluk T,et al. Final results of the choroid plexus tumor study CPT-SIOP-2000. J Neurooncol. 2022;156(3):599-613. doi: 10.1007/ s11060-021-03942-0.
- Safaee M, Oh MC, Bloch O, et al. Choroid plexus papillomas: advances in molecular biology and understanding of tumorigenesis. Neuro Oncol. 2013;15(3):255-267. doi:10.1093/neuonc/nos289
- Lin H, Leng X, Qin CH, Du YX, Wang WS, Qiu SJ. Choroid plexus tumours on MRI: similarities and distinctions in different grades. Cancer Imaging. 2019 Mar 20;19(1):17. doi: 10.1186/s40644-019-0200-1. PMID: 30894223; PMCID: PMC6427869.
- Chen Y, Zhao R, Shi W, Li H. Pediatric atypical choroid plexus papilloma: Clinical features and diagnosis. Clin Neurol Neurosurg. 2021 Jan; 200:106345. doi: 10.1016/j.clineuro.2020.106345. Epub 2020 Nov 4. PMID: 33203591.
- Sethi D, Arora R, Garg K, Tanwar P. Choroid plexus papilloma. Asian J Neurosurg. 2017;12(1):139-141. doi:10.4103/1793-5482.153501
- Jaiswal AK, Jaiswal S, Sahu RN, Das KB, Jain VK, Behari S. Choroid plexus papilloma in children: Diagnostic and surgical considerations. J Pediatr Neurosci. 2009;4(1):10-16. doi:10.4103/1817-1745.49100
- Lin H, Leng X, Qin CH, Du YX, Wang WS, Qiu SJ. Choroid plexus tumours on MRI: similarities and distinctions in different grades. Cancer Imaging. 2019;19(1):17. doi: 10.1186/s40644-019-0200-1.
- Thomas C, Soschinski P, Zwaig M, et al. The genetic landscape of choroid plexus tumors in children and adults. Neuro Oncol. 2021;23(4):650-660. doi:10.1093/neuonc/noaa267
- Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM. Choroid plexus tumours. Br J Cancer. 2002;87(10):1086-1091. doi: 10.1038/sj.bjc.6600609
