Video Radiology Reports May Improve Communication with Patients
 Using video radiology reports may improve radiologists’ communication with patients, further highlighting the importance of imaging in patient-centered care, according to a study published in the American Journal of Roentgenology (AJR).
Using video radiology reports may improve radiologists’ communication with patients, further highlighting the importance of imaging in patient-centered care, according to a study published in the American Journal of Roentgenology (AJR).
“Patient-centered video radiology reports are a useful tool to help improve patient understanding of imaging results,” explained lead researcher Michael P. Recht, MD, the Louis Marx professor and chair of radiology at New York University’s Grossman School of Medicine. “The mechanism of creating the video reports and delivering them to patients can be integrated into existing informatics infrastructure.”
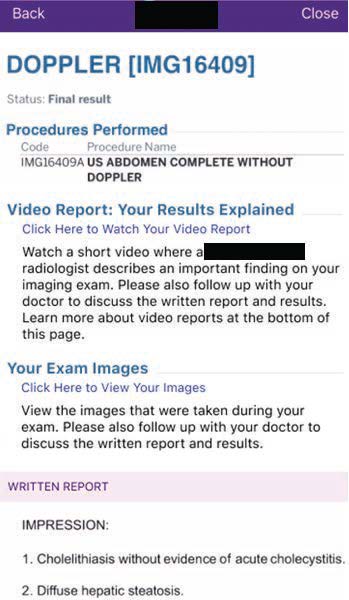
Dr. Recht and colleagues collaborated with Visage Imaging GmbH to build an integrated video reporting tool inside the diagnostic viewer, allowing for both image and voice capture. To aid patient understanding of cross-sectional images, cinematic rendered images were automatically created. For their incorporation into video reporting, these images were immediately available at the workstation. Video radiology reports were then uploaded to the institutional health portal, alongside clinical notes and examination images. Finally, a 10-question survey was administered to patients, assessing their perception of the video reports and requesting feedback.
From September 20, 2021 to January 22, 2022, 105 out of 227 faculty radiologists created a total of 3,763 video radiology reports, with patients viewing 864 unique videos. Based on 101 survey respondents, patients rated their overall experience with video radiology reporting a 4.7 out of 5. Specifically, video radiology reports using lay language and annotated images helped improve patients’ understanding of their results.
Pointing out that the mean time to create a video radiology report was under 4 minutes, “continued development is necessary to further shorten the creation time, so that use of video reports can expand from limited use in selected cases to more widespread use in daily clinical practice,” the authors added.
Related Articles
Citation
. Video Radiology Reports May Improve Communication with Patients. Appl Radiol.
April 20, 2022