Retroperitoneal seminoma
Images

Retroperitoneal seminoma
Findings
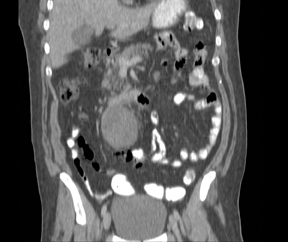
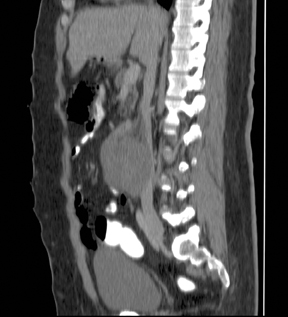
Contrast-enhanced CT of the abdomen and pelvis with coronal and sagittal reconstructions (Figures 1, 2 and 3) revealed a 7-cm homogeneous, well-circumscribed, soft-tissue mass just caudal to the third portion of the duodenum to the right of the midline with marked compression of the inferior vena cava. No lymphadenopathy was identified. A diagnosis of pure seminoma, likely metastatic, was made by on image-guided biopsy. A testicular ultrasound was performed after to diagnosis and showed only a small right hydrocele with no focal masses or calcifications. The mass was surgically resected, and the patient declined an orchiectomy. After 3 cycles of platinum-based chemotherapy, the patient’s tumor markers have normalized.
Discussion
Between 2% and 5% of malignant germ-cell tumors in men arise at extragonadal sites. Whether these tumors develop primarily at extragonadal sites or represent metastases of a primary testicular tumor remains uncertain. Most extragonadal germ-cell tumors (EGCTs) are likely metastases of a viable or burned-out testicular tumor.1 They typically arise at or near the midline presenting as brain, mediastinal, retroperitoneal, spinal, or sacrococcygeal masses.2 Seminomas account for 30% to 40% of EGCTs, and the retroperitoneum is the second most common site after the mediastinum.3
Extragonadal seminomas usually appear as large, lobulated, well-marginated, and homogeneous masses on CT and magnetic resonance (MR). Although invasion of adjacent organs is rare, metastases to regional lymph nodes and bone can be seen. Calcifications are uncommon, and it is very rare for these tumors to have a cystic component.4
Patients with retroperitoneal germ cell tumors usually present after their tumors have reached large dimensions.
Symptoms are nonspecific and may include a palpable abdominal mass with or without pain, backache, and weight loss.3 Beta-human chorionic gonadotropin hormone is elevated in 5% to 10% of patients. Scrotal ultrasound and urologic exam is important since burned-out testicular tumors have been detected in 76% of cases of EGCT.1
Survival of patients with extragonadal seminoma is generally good with 5-year survival rates of 90% following treatment with platinum-based chemotherapy.5
The differential diagnosis of a homogeneous, soft-tissue mass in the retroperitoneum includes lympho ma, metastasis, soft-tissue sarcoma, malignant fibrous histiocytoma, and neurogenic tumor. Diagnosis is based on biopsy with adequate tissue for microscopic examination, flow cytometry, immunostaining, and other molecular studies.
Conclusion
Extragonadal germ cell tumor in the retroperitoneum is rare. Although imaging of this tumor is somewhat nonspecific, this rare entity should be considered in the differential diagnosis of a male patient presenting with a single, homogeneous, soft-tissue mass occurring at or near the midline, especially if in the mediastinum or retroperitoneum.
- Scholz M, Zehender M, Thalmann GN, et al. Extragonadal retroperitoneal germ cell tumor: Evidence of origin in the testis. Ann Oncol. 2002;13:121-124.
- Dubey RB, Sachdev YP, Hegde AN. Varied appearances of extragonadal germ cell tumors on radiographs and CT: A Pictorial Essay. Ind J Radiol Imag 2004;14:3:273-278.
- Sachdeva K, Makhoul I, Curti B. Extragonadal germ cell tumors. Medscape.com. http://emedicine.medscape.com/article/278174-overview. Updated December 2, 2011. Accessed February 28, 2012.
- Ueno T, Tanaka YO, Nagata M, et al. Spectrum of germ cell tumors: From head to toe. RadioGraphics. 2004;24:387-404.
- Comite CV, Renshaw AA, Benson CB, Loughlin KR. Burned-out primary testicular cancer: Sonographic and pathological characteristics. J Urol. 1996;156:85-88.