Pulmonary Artery Pseudoaneurysm
Pulmonary artery pseudoaneurysm (PAP) is a rare complication of trauma or infection. They grow unpredictably and, therefore, are often discovered incidentally or after massive hemoptysis. Hemoptysis due to PAP rupture is often fatal due to the risk of asphyxiation and exsanguination. PAPs are typically diagnosed via CT pulmonary angiogram and are treated endovascularly.
Keywords: thorax, vascular, infection
Case Summary
A teenager with a history of type 1 diabetes was admitted to the hospital for diabetic ketoacidosis after becoming infected with the SARS-CoV-2 virus and subsequent superimposed bacterial pneumonia. Ten days after discharge, she was readmitted to the hospital due to new-onset hemoptysis. She continued to have symptoms of fever, cough, fatigue, dyspnea, labile blood glucose levels, and emesis. One week later, she had massive hemoptysis and was readmitted with hypotension. Pulmonary biopsy revealed superinfection with Zygomycete, a mucor-like fungal organism.
Imaging Findings
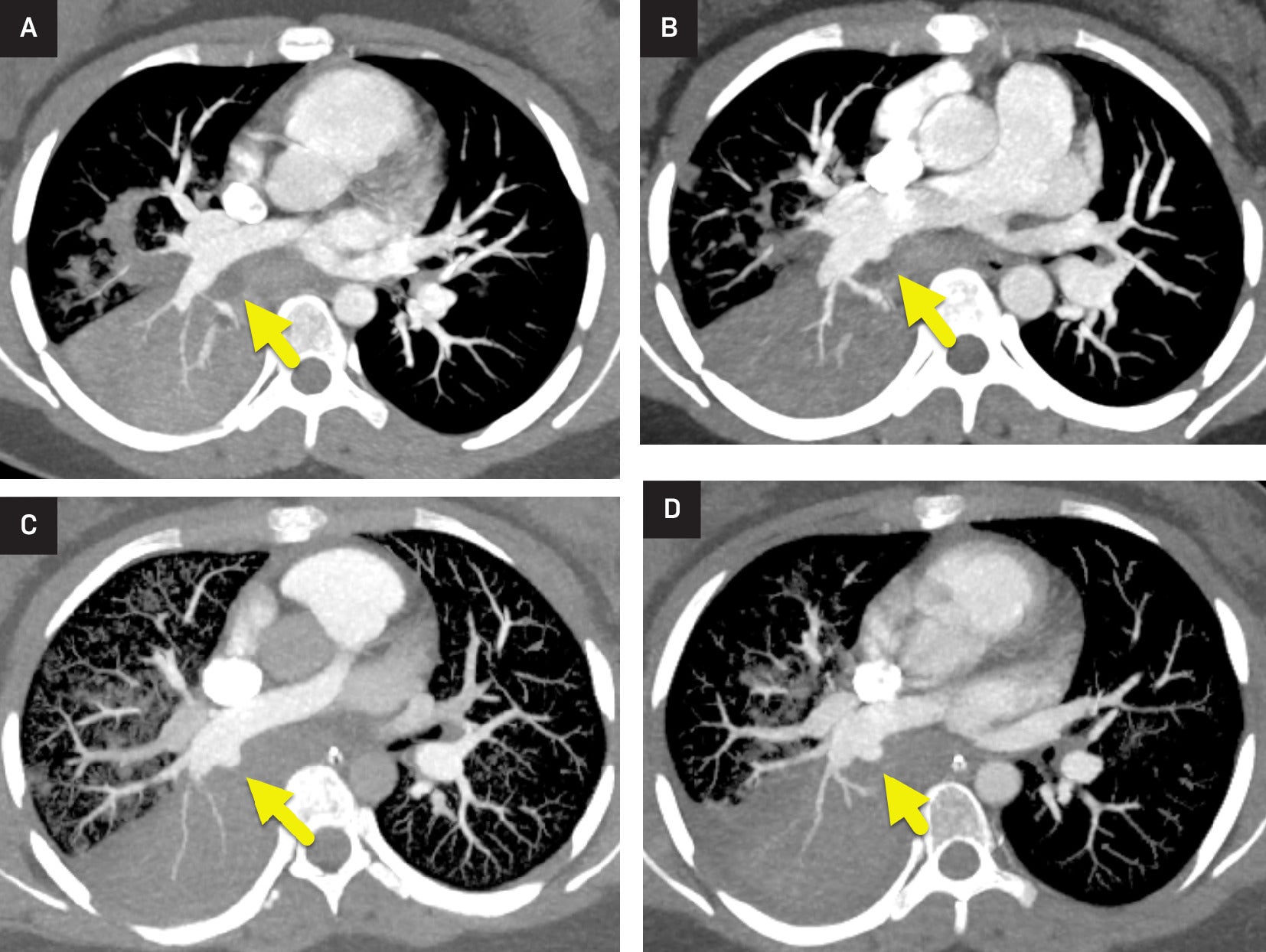
Sequential CT pulmonary angiograms ( Figure 1 ) showed right lower lobe consolidation with patchy opacities in all lobes. On the first CT, there was a focal hypodense region within the right lower lobe adjacent to the right pulmonary artery. Over time, a pseudoaneurysm developed along the posterior wall of the right pulmonary artery and became progressively larger.
(A) Axial maximum intensity projection images from CT pulmonary angiogram performed at admission during the initial onset of hemoptysis, (B) 7 days later, at the onset of massive hemoptysis, (C) 9 days after the initial CT, and (D) 11 days after the initial CT. All scans show consolidation of the right lower lobe and patchy areas of opacity in other lobes. On the first image, there is a local, more hypodense region (arrow in A) within the right lower lobe consolidation, posterior to the right pulmonary artery. Later images show a pseudoaneurysm (arrow in B-D) forming and growing at this location.
Diagnosis
Pulmonary artery pseudoaneurysm.
Differential for clinical presentations of hemoptysis: Pulmonary artery aneurysm, pulmonary tuberculosis, malignancies involving the lungs, bronchiectasis, infections (chronic bronchitis and pneumonia), and conditions of vasculitis.1 Imaging differential includes pulmonary nodules, malignancy, true aneurysm, pulmonary arteriovenous malformation, and septic embolism.2 Hematemesis may be difficult to distinguish from hemoptysis. The differential diagnosis for hematemesis includes peptic ulcers, esophageal varices, gastritis, and esophageal tears.
Discussion
PAP is an extremely rare entity in the pediatric community that can result from trauma, infection, malignancies, and congenital heart diseases.3 - 5 Radiologic diagnosis of PAPs typically occurs via CT pulmonary angiogram or pulmonary arteriography.2, 4 Due to the rarity of occurrence, the incidence of PAPs in the pediatric community remains unknown.
An aneurysm is defined as the abnormal dilation of all three layers of a vessel wall beyond the normal capacity of the vessel wall. A pseudoaneurysm occurs following vessel injury, leading to extravasation of blood from the vessel and containment of blood by vascular or perivascular tissue. In comparison to a true aneurysm, a pseudoaneurysm occurs with abnormal dilation of the artery and disruption of at least one of the three vessel layers. The disruption inherently weakens the vessel wall, leading to an increased risk of rupture.2 - 4 In many instances of PAP, the inciting vascular injury goes unrecognized. Because pseudoaneurysm formation does not follow a predictable timeline, PAP is typically not diagnosed until the patient is symptomatic or imaged for another cause.6 Hemoptysis is the most common presenting symptom in patients with PAP. However, many patients are asymptomatic.4 Late diagnosis leads to a mortality rate of >50% due to the risk of significant hemoptysis, asphyxiation, and exsanguination.2 - 9
PAPs are classified by their location within the pulmonary arterial tree as either proximal or peripheral. Proximal PAP affects the main pulmonary artery, the right or left pulmonary artery, or the right interlobar pulmonary artery. A PAP occurring on a more distal vascular branch is peripheral.10
PAP may occur as a result of infection or trauma (either blunt, penetrating, or iatrogenic).8, 11 Pulmonary infections are increasingly a cause of PAP in the pediatric population.2, 4 - 6 Pathogens associated with the formation of PAP include Mycobacterium tuberculosis (Rasmussen aneurysm), Staphylococcus aureus, Candida albicans, Streptococcus viridans , and enterococcal species.4 - 6
PAP can be diagnosed via imaging. Peripheral PAP may appear as a pulmonary nodule on chest radiograph, while proximal PAP may not be visible unless the pseudoaneurysm is very large.2 CT pulmonary angiogram is the most used modality to diagnose PAP ( Figure 1 ). The CT shows a focal outpouching of a proximal pulmonary artery or a hyper-enhancing nodule in direct communication with a peripheral pulmonary artery ( Figure 1 ).2 Pulmonary angiography is the gold-standard modality for diagnosis and treatment. However, its use in diagnosis has fallen from favor due to its invasive approach.2
PAP can be treated via open surgical and endovascular approaches.11 Endovascular methods, such as placement of covered stents or stent grafts, are currently favored as they have been shown to decrease mortality and morbidity as compared to the open approaches.11 Peripheral PAP may be treated with embolization of the involved pulmonary artery branch.9 When surgery is performed, the PAP is ligated or resected as part of a wedge resection or lobectomy.6, 9 Our patient was treated with covered stents. Unfortunately, her infection was severe and ultimately led to her death.
Conclusion
PAP is a rare complication of trauma or infection. They grow unpredictably and, therefore, are often discovered incidentally or after massive hemoptysis. Hemoptysis due to PAP rupture is often fatal due to the risk of asphyxiation and exsanguination. PAPs are typically diagnosed via CT pulmonary angiogram and are treated endovascularly.
References
Citation
Borsa JA, Towbin RB, Schaefer CM, Towbin AJ.Pulmonary Artery Pseudoaneurysm. Appl Radiol. 2025; (1):1 - .
doi:10.37549/JPCR-25-0003
October 1, 2025