Pseudotumoral Sarcoidosis of the Spleen
Sarcoidosis is a nonneoplastic condition characterized by noncaseating granulomas, primarily in the lungs. This condition is usually asymptomatic; however, extrapulmonary manifestations may exist, including noncaseating granulomas in other organs such as the spleen. On imaging, these lesions may resemble cancer, such as lymphoma, necessitating a biopsy for further histological workup. In patients with a history of malignancy, this workup is absolutely indicated to rule out more ominous conditions compared to the relatively benign condition of sarcoidosis. Once lymphoma and other neoplastic conditions are ruled out, a splenectomy may be performed if the patient is experiencing splenomegaly or pancytopenia to resolve symptomology. In our patient with a cancerous history and confirmed sarcoidosis of the lungs who was experiencing splenomegaly and pancytopenia, radiograph imaging and further histological analysis were absolutely necessary to rule out neoplastic conditions, and a splenectomy was performed to resolve her symptoms.
Keywords: sarcoidosis, pseudotumor, splenic lesions
CASE SUMMARY
An elderly patient presented for a routine checkup, with recent lab work demonstrating progressive anemia. The patient’s medical history included breast cancer treated with chemotherapy/radiation and lumpectomy; Hodgkin lymphoma and non-Hodkin lymphoma treated with chemotherapy; sarcoidosis; obstructive sleep apnea; and asthma. Other notable history included multiple packed red blood cell transfusions required for the previous surgeries.
Clinical blood work demonstrated low hemoglobin, hematocrit, and red blood cell levels. The physical exam demonstrated splenomegaly on palpation.
IMAGING FINDINGS
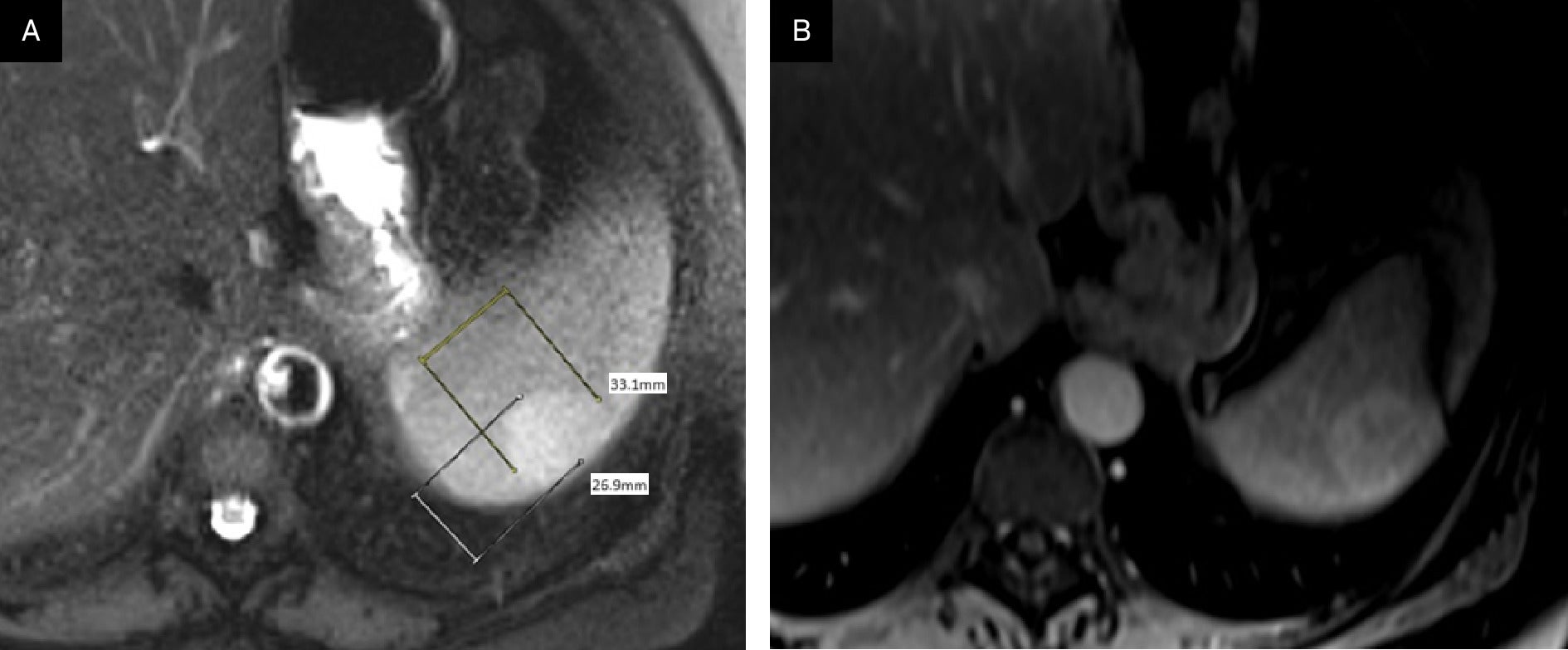
Given the patient’s cancer history and anemia, CT imaging was performed, demonstrating a mildly hyperdense 13.1 cm lesion in the portal venous phase ( Figure 1 ), with no other significant findings. Multiphasic, multiplanar MRI demonstrated a 3.3 cm × 2.7 cm mildly T2 hyperintense, enhancing lesion in the posterior aspect of the spleen ( Figure 2 ).
Axial CT abdomen demonstrates a mildly hyperdense solitary 3.1 cm lesion in portal venous phase.

(A) T2 axial MRI demonstrates a mildly hyperintense 3.3 cm × 2.7 cm solitary lesion in the periphery of the spleen. (B) Post-contrast MRI scan in the portal venous phase demonstrates mildly heterogeneous enhancement.
Pathology demonstrated noncaseating granulomas without evidence of malignancy, ruling out breast cancer or lymphoma metastasis. Acid-fast bacilli and Grocott methenamine silver stains were negative for microorganisms. No foreign material was seen under polarizable light. The findings were deemed consistent with splenic involvement of sarcoidosis.
DIAGNOSIS
Pseudotumoral sarcoidosis of the spleen.
Differential diagnoses included lymphoma, metastasis, and sarcoidosis.
DISCUSSION
Sarcoidosis was first reported in 1877 by Jonathan Hutchinson, who described unusual skin nodules of unknown pathophysiology.1 The exact etiology of sarcoidosis remains unknown, but it is theorized to involve genetic components as well as possible exposure to substances and infectious agents.2 However, sarcoidosis is known to be a nonneoplastic condition characterized by the development of noncaseating granulomas in various organs and systems, most commonly the lungs and lymph nodes. Other areas are less commonly involved, with manifestations in the spleen and other organ systems reported in approximately 10-50% of patients.3
Presentation is often asymptomatic,4 and the condition is often discovered incidentally on imaging. However, patients may experience constitutional symptoms such as cough, dyspnea, weight loss, and fever, with up to 30% experiencing extrapulmonary symptoms. Patient morbidity is often due to pulmonary complications; therefore, thoracic imaging findings are used to stage severity.
The most common scoring system for sarcoidosis is the Scadding staging system, which uses chest radiography to stage disease progression.5 However, extrapulmonary manifestations found on imaging may present a diagnostic challenge. The typical presentation of extrapulmonary sarcoidosis in the abdomen includes multiple small and often hypoenhancing nodules in the liver and spleen.6
Solitary, solid-appearing, enhancing masses are uncommon7 and present a diagnostic conundrum, given that more ominous and potentially malignant etiologies, such as lymphoma, are to be considered, especially in patients with a history of malignancy.
In the absence of a concerning history of such conditions as immunocompromise or malignancy, a less aggressive approach can be considered when abdominal manifestations of sarcoid present with typical imaging findings of multiple hypoenhancing nodules. These cases often follow a benign clinical course and, absent systemic symptoms or significant pancytopenia, conservative management with steroids and patient monitoring is appropriate; splenomegaly tends to regress within one year.8
However, the presence of atypical features on imaging, such as a large, solitary, solid mass, raises concern for and typically necessitates histopathological confirmation to rule out malignancy. This is particularly important, as the radiologic appearance of sarcoid lesions can closely mimic that of splenic lymphoma or other metastatic processes, especially in patients with an oncologic history.9
Additionally, some splenic sarcoidosis patients experience pancytopenia, which may also mirror lymphoma. Moreover, if symptoms such as abdominal pain, splenomegaly, and pancytopenia are present, a splenectomy may be considered.10 In our patient, a history of malignancy and pancytopenia was present, requiring an aggressive histological approach to rule out malignancy. A splenectomy was performed, resulting in complete resolution of symptoms.
Although extrapulmonary lesions are common in sarcoidosis, ominous findings may require further investigation. Imaging is necessary to identify possible masses in sarcoidosis patients with splenomegaly and prior malignancies; histological sampling is further indicated to diagnose the cause of the masses, and splenectomy may be considered to resolve any associated symptoms. This stepwise process is essential for diagnosis, guiding treatment options, and reduction of morbidity and mortality.
CONCLUSION
Sarcoidosis is a nonneoplastic condition with the development of noncaseating granulomas, most commonly in the lungs and less commonly in extrapulmonary locations such as the spleen. Unusual imaging manifestations of sarcoidosis, including pseudotumoral presentation with a solitary mass, can present significant diagnostic challenges. Recognition of this presentation is essential, as the condition impacts treatment options and management decisions.
References
Citation
Shah S, Fast A, Roudenko A.Pseudotumoral Sarcoidosis of the Spleen. Appl Radiol. 2025;
doi:10.37549/AR-D-25-0085
October 1, 2025