Primary Small Cell Carcinoma of the Tonsil
Case Summary
A middle-aged patient presented to the otolaryngologist with a progressive sore throat and cough. The patient’s medical history included ischemic cardiomyopathy with automatic implantable cardioverter defibrillator placement, coronary artery disease with myocardial infarction and coronary artery bypass graft, cerebrovascular accident, atrial fibrillation, mitral valve regurgitation, diabetes mellitus, and dyslipidemia. They denied any history of smoking or alcohol use.
On exam, the patient was found to have a right tonsillar mass, which was subsequently biopsied.
Pathology demonstrated the proliferation of crowded malignant cells. Neoplastic cells were found to be positive for OSCAR pancytokeratin, CD56, synaptophysin, and chromogranin. P16 was found to be positive. P40, CK5/6, and P63 were negative.
Imaging Findings
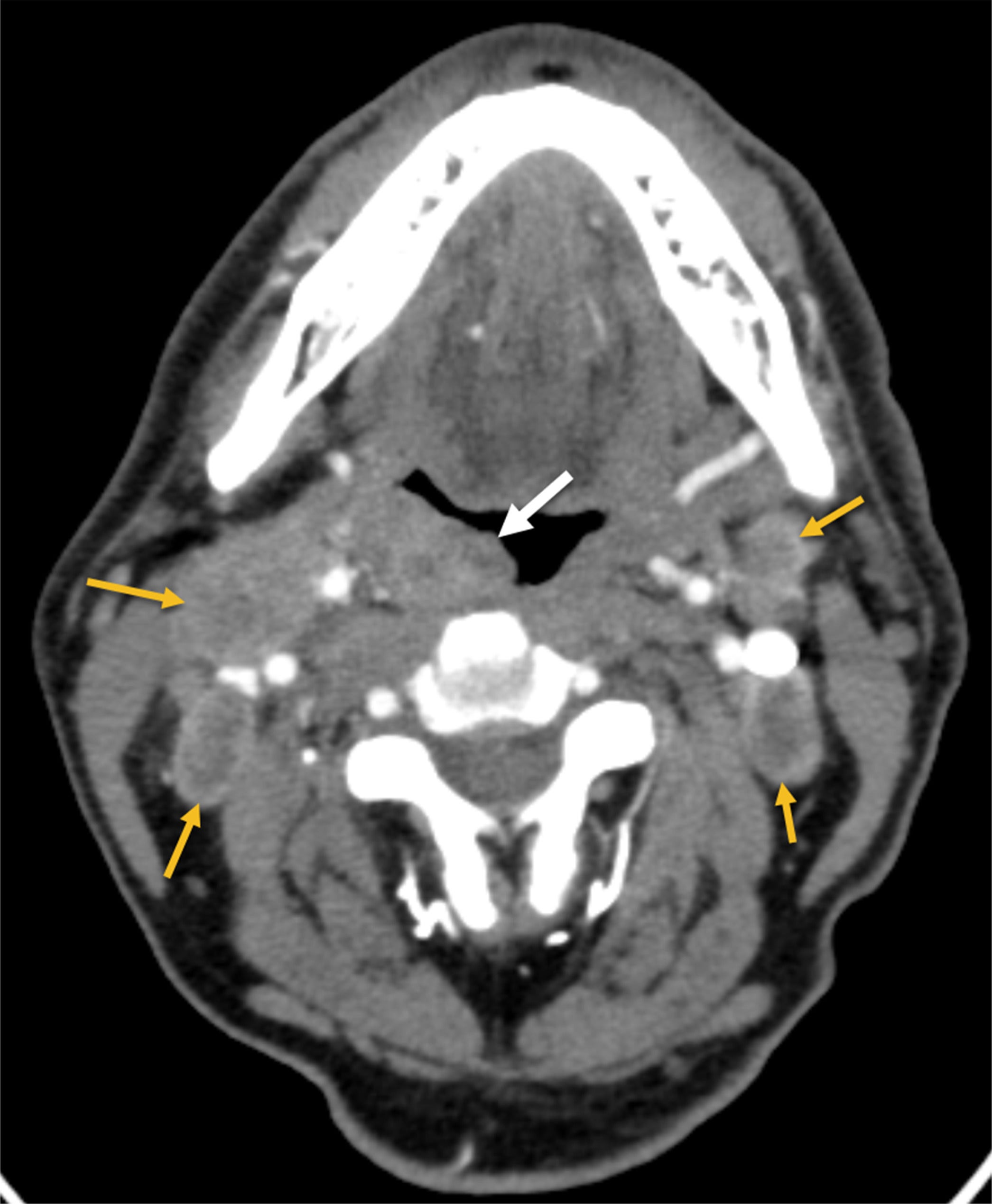
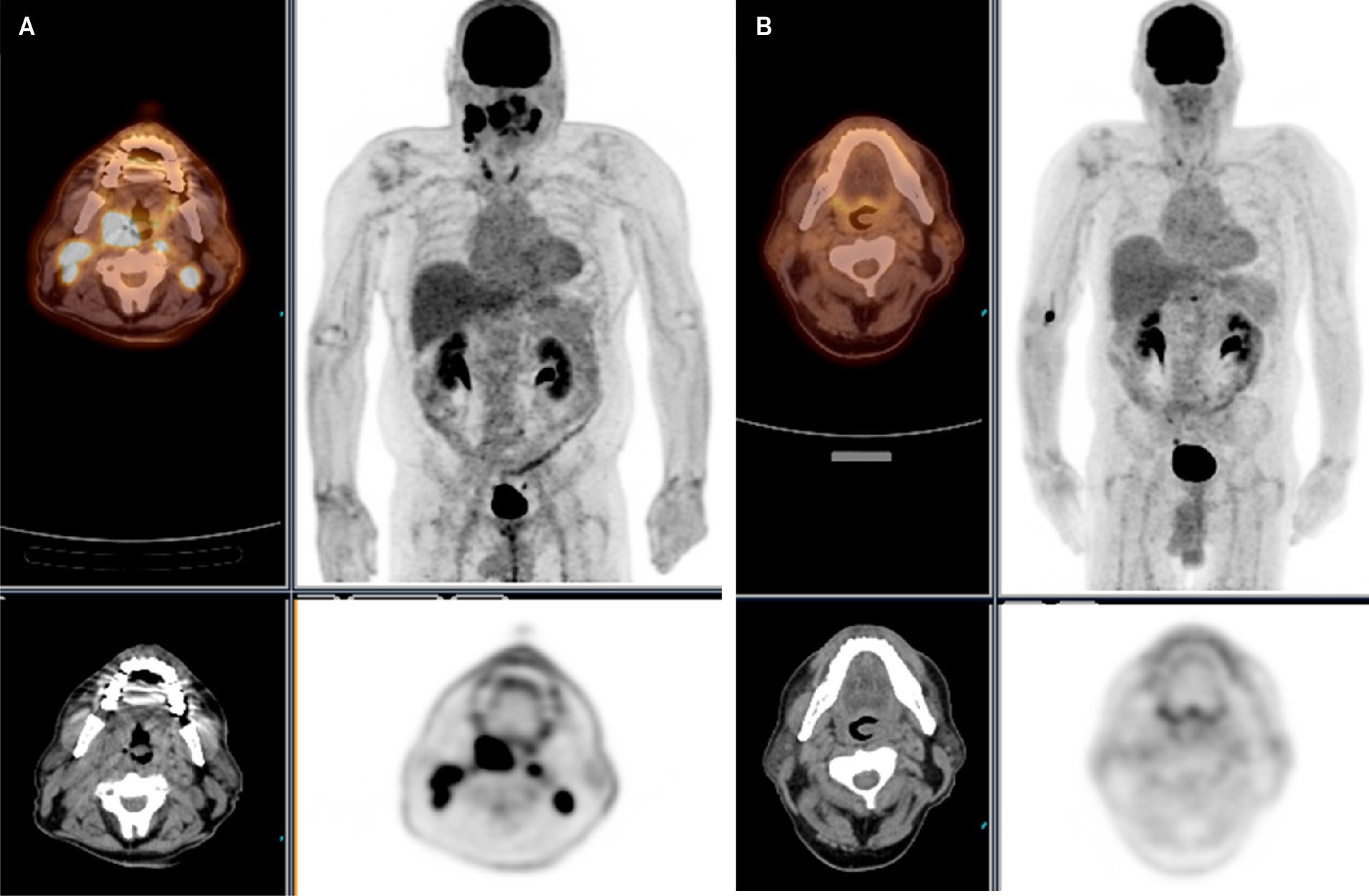
Contrast-enhanced CT of the neck ( Figure 1 ) demonstrated bilateral neck lymphadenopathy and a right palatine tonsil mass. Initial18 F fluorodeoxyglucose PET/CT scan ( Figure 2 ) demonstrated significant uptake in right palatine tonsil mass (Standardized Uptake Value (SUV) max 22) and bilateral neck lymph nodes (SUV max 11). The scan revealed no other FDG-avid masses specifically in the lungs. Following 4 cycles of cisplatin/etoposide chemotherapy and radiation therapy (60 Gy, Figure 2 ) and 5 months after the patient’s initial presentation, PET/CT demonstrated complete metabolic response with resolution of abnormal metabolism in right palatine tonsil mass and bilateral neck lymphadenopathy
CT scan of the neck with intravenous contrast demonstrates a right palatine tonsil mass (white arrow) and bilateral neck lymphadenopathy (yellow arrows).
(A) An F-18 fluorodeoxyglucose ( 18F FDG) PET/CT scan with significant uptake in the right palatine tonsil and bilateral neck lymph nodes. (B) 18F FDG PET/CT scan demonstrates complete metabolic response and resolution of abnormal metabolism in the right palatine tonsil and bilateral neck lymph nodes.
Diagnosis
Primary small cell carcinoma (SCC) of the tonsil
Discussion
SCCs are poorly differentiated tumors most commonly seen in the lungs, with extrapulmonary SCCs occurring in only 5% of all cases.1 Tonsillar tumors are most often diagnosed as squamous cell carcinomas, which are associated with risk factors such as smoking, alcohol consumption, and human papilloma virus (HPV) infection.2 Primary tonsillar SCC is extremely rare, with approximately 30 cases reported since it was first described in 1972.2 - 5 Symptoms of tonsillar SCC include neck mass, tonsil pain, odynophagia, cervical lymphadenopathy, sore throat, and metastasis.2 - 5 It has been suggested that HPV may play a role in the pathogenesis of tonsillar SCC.3 There have also been reports of tonsillar SCC mixed with SqCC,3, 6 and it has also been suggested that SCC may represent a form of disease progression of SqCC.3
SCC is primarily diagnosed pathologically with H&E staining, although diagnosis is often aided by immunohistochemical analysis. These entities commonly stain positive for CD56, chromogranin, and synaptophysin.1 CT often demonstrates a tonsillar mass with cervical lymphadenopathy.2, 4, 5 SCC of the tonsil should prompt investigation for metastasis from other sites, particularly from the lung.
Paraneoplastic syndromes have a well-known association with SCC of the lung.5 While previous reviews have not reported paraneoplastic syndromes with tonsillar SCC,5 Mineta et al reported ectopic antidiuretic hormone (ADH) production, while Omakobia et al reported a likely case of paraneoplastic syndrome associated with cerebellar signs and diplopia.7
Given the rarity of the disease, there is no standard treatment protocol for tonsillar SCC. However, treatment typically combines chemotherapy (platinum-based regimens with etoposide), radiation therapy, and resection.2, 8 These treatments are guided mostly by previously established treatment standards in SCC of the lung or larynx.2 While the initial response may appear promising, primary disease resolution is often followed by the discovery of distant metastases.2, 6 Common sites of metastasis include the liver, lungs, bones, brain, and skin.2, 4, 9, 10 Primary tonsillar SCC carries a dismal prognosis, with one recent review reporting recurrence or distant metastasis in 66.7% of cases and a median survival of 18 months.2
Conclusion
Primary SCC of the tonsil is exceedingly rare and has a significant mortality rate despite chemotherapy, radiation therapy, and tumor resection. Patients may present with a sore throat, odynophagia, cough, neck mass, cervical lymphadenopathy, and metastasis. Imaging commonly demonstrates a tonsillar mass with local cervical lymph node spread. Discovery of tonsillar SCC should prompt investigation to exclude other sites of primary SCC, such as the lungs. Although initial treatment may appear successful, clinicians should proceed with careful and recurrent evaluation of patients owing to the significant risk for metastasis.
References
Citation
Cunningham JE, Kalapparambath T.Primary Small Cell Carcinoma of the Tonsil. Appl Radiol. 2025; (4):
doi:10.37549/AR-D-25-0098
October 1, 2025