Diagnosis and Endovascular Management of Life-threatening Rectal Bleeding
Images
CASE SUMMARY
A 61-year-old was admitted for management of ascites related to alcoholic cirrhosis. The patient also reported a history of lower gastrointestinal (GI) bleeding from colonic angiodysplasia. During the inpatient stay, they experienced mild bleeding from rectal varices, which were successfully banded at endoscopy.
Forty-eight hours after endoscopy, the patient developed massive lower GI bleeding with hypotension, requiring initiation of the hospital’s massive infusion protocol. Interventional radiology (IR) was consulted for arterial embolization.
The patient had ongoing massive lower GI hemorrhage and was on multiple vasopressors. The medical intensivists felt the patient would not survive two separate transfers and requested to bypass an initial CT angiography and bring the patient directly to the IR suite.
This patient had known cirrhotic liver disease with portal colopathy and recently banded rectal varices that were thought to be an unlikely source for the current hemorrhage because they were believed to have been successfully treated. Given their history of colonic angiodysplasia, this was suspected as the current source of hemorrhage.
With the patient on his way to the IR suite and ongoing life-threatening hemorrhage, identifying the etiology of the bleed became critical, as the approach would be angiography/embolization or placement of a transjugular intrahepatic portocaval shunt (TIPS) for an arterial or venous bleed, respectively.
By utilizing our 4DCT Angiography suite, we immediately performed a CTA on the same table as the intervention. Noncontrast, arterial, venous, and delayed phases were obtained.
IMAGING FINDINGS
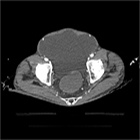
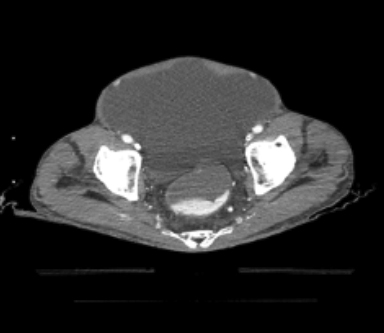
CT angiography of the abdomen and pelvis demonstrated no active contrast extravasation on the arterial phase (Figure 1). Venous- and delayed-phase images revealed contrast extravasation in the rectum adjacent to prominent rectal varices (Figure 2).
A TIPS procedure was emergently performed based on the CTA finding of active venous bleeding from large rectal varices.
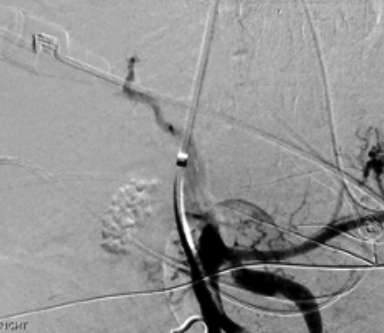
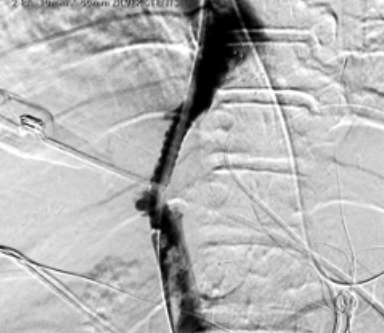
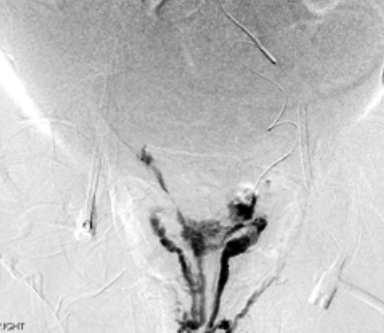
Initial venogram of the portal vein demonstrated hepatofugal flow with retrograde flow down both the superior and inferior mesenteric veins (Figure 3). The portal system was successfully decompressed following TIPS placement (Figure 4). While hepatopetal flow was restored in both the portal vein and superior mesenteric vein, flow in the interior mesenteric vein (IMV) remained retrograde and sluggish.
INTERVENTION
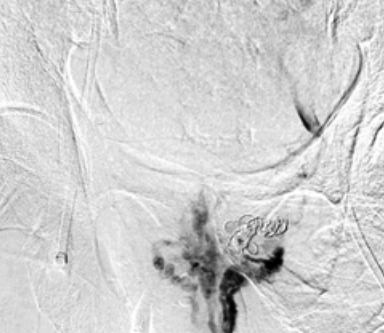
Selective catheterization of the IMV was performed and venogram was obtained demonstrating robust rectal varices with small-volume active extravasation in the vicinity of the left rectal wall (Figure 5), correlating to the findings on initial CTA. The actively bleeding varix was successfully embolized with coils (Figure 6). Proceeding in this fashion and eliminating the need to transfer a hemodynamically unstable patient to multiple locations saved a minimum of 30 minutes, allowing rapid and efficient treatment this critically ill patient.
DISCUSSION
Identifying the exact source and location of lower GI bleeding can often prove challenging. The most common causes for hemorrhage include diverticulosis, angiodysplasia, and internal hemorrhoids. Bleeding from these sources will typically arrest spontaneously. Intervention may be necessary in cases of recurrent, refractory, or hemodynamically significant hemorrhage. These interventions include endoscopy, angiography with embolization, and/or surgery.
Initial assessment should include a clinical history and physical exam. While patients with previous episodes of hemorrhage will likely re-bleed from the same source, care should be taken to assess all potential sites of bleeding to avoid the “satisfaction of search” phenomenon. Differentiating between an arterial source versus bleeding from gastrointestinal ectopic varices or portal colopathy can also prove challenging.
Dilated portosystemic varices outside of the gastroesophageal junction account for only 2-5%1-3 of variceal bleeds, yet they carry a mortality rate as high as 40%.4, 5 Of these, over 60% are rectal varices.6 Rectal varices occur as a result of communication between the superior rectal vein and the middle or inferior rectal veins. These veins dilate owing to high pressure from reversed flow in the draining veins of this region.
Although rectal variceal rupture is rare (0.5-3.6%),7-10 life-threatening hemorrhage can result when it does occur. In addition to rectal varices, portal colopathy can result in hemorrhage. This pathology is defined by mucosal changes that can produce telangiectasias and angiodysplastic-like lesions.
Lower endoscopy remains the gold standard for initial assessment and localization of bleeding in stable patients. This changes in the setting of massive, life-threatening lower GI hemorrhage. Bleeding is often so brisk that it cannot be identified or controlled endoscopically. At our institution, the next step is to obtain a CTA followed by embolization.
Conclusion
Identifying the source of massive lower GI hemorrhage can prove challenging, especially in patients with multiple potential etiologies. Good outcomes can be achieved, however, with rapid triage, diagnosis, and the flexibility to quickly change the treatment approach when warranted.
References
- Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. Oct 1998;28(4):1154-8. doi:10.1002/hep.510280434.
- Sato T, Akaike J, Toyota J, Karino Y, Ohmura T. Clinicopathological features and treatment of ectopic varices with portal hypertension. Int J Hepatol. 2011;2011:960720. doi:10.4061/2011/960720.
- Sharma B, Raina S, Sharma R. Bleeding ectopic varices as the first manifestation of portal hypertension. Case Reports Hepatol. 2014;2014:140959. doi:10.1155/2014/140959.
- Almadi MA, Almessabi A, Wong P, Ghali PM, Barkun A. Ectopic varices. Gastrointest Endosc. Aug 2011;74(2):380-8. doi:10.1016/j.gie.2011.03.1177.
- Saad WE, Lippert A, Saad NE, Caldwell S. Ectopic varices: anatomical classification, hemodynamic classification, and hemodynamic-based management. Tech Vasc Interv Radiol. Jun 2013;16(2):158-75. doi:10.1053/j.tvir.2013.02.004.
- Romano-Munive AF, Tellez-Ávila FI. Bleeding from gastrointestinal ectopic varices is not associated with haemorrhage from oesophageal or gastric varices. Prz Gastroenterol. 2020;15(1):60-64. doi:10.5114/pg.2020.93632.
- Herman BE, Baum S, Denobile J, Volpe RJ. Massive bleeding from rectal varices. Am J Gastroenterol. Jun 1993;88(6):939-42.
- Johansen K, Bardin J, Orloff MJ. Massive bleeding from hemorrhoidal varices in portal hypertension. Jama. Nov 7 1980;244(18):2084-5.
- McCormack TT, Bailey HR, Simms JM, Johnson AG. Rectal varices are not piles. Br J Surg. Feb 1984;71(2):163. doi:10.1002/bjs.1800710236
- Wilson SE, Stone RT, Christie JP, Passaro E. Massive lower gastrointestinal bleeding from intestinal varices. Arch Surg. Oct 1979;114(10):1158-61. doi:10.1001/archsurg.1979.01370340064011.
Further Reading
- Chawla Y, Dilawari JB. Anorectal varices--their frequency in cirrhotic and non-cirrhotic portal hypertension. Gut. Mar 1991;32(3):309-11. doi:10.1136/gut.32.3.309.
- Fantin AC, Zala G, Risti B, Debatin JF, Schˆpke W, Meyenberger C. Bleeding anorectal varices: successful treatment with transjugular intrahepatic portosystemic shunting (TIPS). Gut. Jun 1996;38(6):932-5. doi:10.1136/gut.38.6.932
- Ganguly S, Sarin SK, Bhatia V, Lahoti D. The prevalence and spectrum of colonic lesions in patients with cirrhotic and noncirrhotic portal hypertension. Hepatology. May 1995;21(5):1226-31.
- Garrido M, GonÁalves B, Ferreira S, Rocha M, Salgado M, Pedroto I. Treating Untreatable Rectal Varices. GE Port J Gastroenterol. Oct 2019;26(6):420-424. doi:10.1159/000496121
- Goenka MK, Kochhar R, Nagi B, Mehta SK. Rectosigmoid varices and other mucosal changes in patients with portal hypertension. Am J Gastroenterol. Sep 1991;86(9):1185-9.
- Helmy A, Al Kahtani K, Al Fadda M. Updates in the pathogenesis, diagnosis and management of ectopic varices. Hepatol Int. 09 2008;2(3):322-34. doi:10.1007/s12072-008-9074-1
- Henry Z, Uppal D, Saad W, Caldwell S. Gastric and ectopic varices. Clin Liver Dis. May 2014;18(2):371-88. doi:10.1016/j.cld.2014.01.002
- Katz JA, Rubin RA, Cope C, Holland G, Brass CA. Recurrent bleeding from anorectal varices: successful treatment with a transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. Jul 1993;88(7):1104-7.
- Kochar N, Tripathi D, McAvoy NC, Ireland H, Redhead DN, Hayes PC. Bleeding ectopic varices in cirrhosis: the role of transjugular intrahepatic portosystemic stent shunts. Aliment Pharmacol Ther. Aug 2008;28(3):294-303. doi:10.1111/j.1365-2036.2008.03719.x
- Okada M, Nakashima Y, Kishi T, et al. Percutaneous transhepatic obliteration for massive variceal rectal bleeding. Emerg Radiol. Aug 2012;19(4):355-8. doi:10.1007/s10140-012-1032-5
- Ory G, Spahr L, Megevand JM, Becker C, Hadengue A. The long-term efficacy of the intrahepatic portosystemic shunt (TIPS) for the treatment of bleeding anorectal varices in cirrhosis. A case report and review of the literature. Digestion. 2001;64(4):261-4. doi:10.1159/000048871
- Sakib SM, Kobayashi K, Jawed M. Potential Pitfalls in Transjugular Portosystemic Shunt Placement for Bleeding Rectal Varices. Case Rep Gastroenterol. 2015 May-Aug 2015;9(2):296-301. doi:10.1159/000439164
- Shibata D, Brophy DP, Gordon FD, Anastopoulos HT, Sentovich SM, Bleday R. Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Colon Rectum. Dec 1999;42(12):1581-5. doi:10.1007/bf02236211
- Then E, Lund C, Uhlenhopp DJ, Sunkara T, Gaduputi V. Cirrhosis Is Associated With Worse Outcomes in Ischemic Colitis: A Nationwide Retrospective Study. Gastroenterology Res. Dec 2020;13(6):253-259. doi:10.14740/gr1339
- Vangeli M, Patch D, Terreni N, et al. Bleeding ectopic varices--treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. Oct 2004;41(4):560-6. doi:10.1016/j.jhep.2004.06.024
- Watanabe N, Toyonaga A, Kojima S, et al. Current status of ectopic varices in Japan: Results of a survey by the Japan Society for Portal Hypertension. Hepatol Res. Aug 2010;40(8):763-76. doi:10.1111/j.1872-034X.2010.00690.x
- Wu X, Xuan W, Song L. Transjugular intrahepatic portosystemic stent shunt placement and embolization for hemorrhage associated with rupture of anorectal varices. J Int Med Res. Apr 2018;46(4):1666-1671. doi:10.1177/0300060517730720
- Yoshino K, Imai Y, Nakazawa M, et al. Therapeutic strategy for patients with bleeding rectal varices complicating liver cirrhosis. Hepatol Res. Oct 2014;44(11):1088-94. doi:10.1111/hepr.12232
Citation
Diagnosis and Endovascular Management of Life-threatening Rectal Bleeding. Appl Radiol.
May 5, 2021