CT scanning of the coronary arteries: How to do it and how to interpret it
Images




Dr. Lawler is an Assistant Professor of Cross Sectional and Interventional Radiology, Johns Hopkins University, Baltimore, MD.
Coronary artery disease remains one of the leading killers in the western world. Given that many of those dying of coronary artery disease have no antecedent history and that a large percentage of cardiac catheter interventions do not involve therapy, there is clearly a role for noninvasive imaging. Alhough it certainly has benefits in other areas, the inspiration and development of multidetector-row computed tomography (MDCT) has largely been driven by an interest in developing such noninvasive coronary angiography.
Fundamentally, cardiac imaging is a straightforward extension of the principles underpinning stationary vessel CT angiography (CTA), though the beating heart introduces some new issues for data acquisition and processing. Although the application of mechanical helical CT for coronary imaging as yet lacks definitive outcome and comparative data, it has nevertheless gained a degree of acceptance in daily cardiology and radiology practice. 1 Like many rapidly developing imaging modalities, cardiac CT implementation appears unlikely to pause for the results of long-term, evidence-based data.
With MDCT still in its infancy, there is no monopoly on the correct way to perform and interpret coronary artery CT at this time. This paper will review and illustrate one approach to the current techniques of coronary artery MDCT data acquisition, processing, and clinical application.
Data acquisition
Patient preparation
With most current scanners, coronary CTA should be reserved for those patients with heart rates <65 beats per minute. Even with the temporal resolution of current MDCT scanners, higher heart rates frequently result in significant motion artifact. One should note that a patient's resting prescan heart rate may rise with anxiety on the scanner and also with the administration of iodinated contrast.Patients should be instructed to avoid high doses of caffeine and other chronotropes the morning of the study. A beta-blocker will slow the heart rate and increase the relative duration of the diastolic phase within the cardiac cycle. Short-acting metoprolol is the most commonly prescribed beta-blocking agent. It may be given as a 50-mg oral tablet on the morning of the procedure or as a 5-mg dose intravenously 30 minutes before the procedure.
Multidetector-row CT
Coronary artery CT is one of the most demanding of CT studies, as it requires simultaneously high spatial, contrast, and temporal resolution. Though the in-plane resolution of the 512 matrix has changed little with new detector arrays, the z-axis resolution and coverage speed has increased. Across the vendors, most current detector designs have 0.625- to 0.75-mm detector units. These provide near isotropic (square) voxels where the viewing perspective for interpretation is almost independent of the plane of acquisition. The short scan duration of 12 to 15 seconds permits a breath-hold imaging duration that can capture homogenous contrast opacification around the narrow peak of contrast enhancement. Temporal resolution (TR) may be thought of as the "shutter speed" of the scanner and is the key to recent advancements in MDCT technology. Temporal resolution in the region of 100 msec, which approximates the performance of electron-beam CT (EBCT), is required to create relatively motionless images of the beating heart. This is largely achieved through fast gantry rotation (~0.37 to 0.42 msec) and segmental reconstruction.
ECG triggering and gating
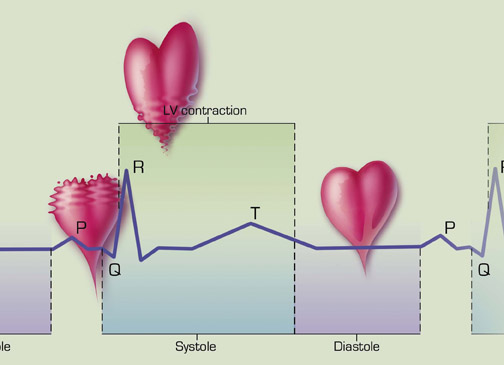
Because of the limitations of current helical mechanical CT, one needs a method to extract the coronary images that are the most diastolic and motionless from a series of complete cardiac cycles (Figure 1). Two methods in use are echocardiographic (ECG) triggering and ECG gating. Using ECG triggering, the scanner acquires data only for a defined period after the signal from the R wave of the ECG trace. This is applied to a nonhelical, translational "step and shoot" scan technique, and an image is acquired every second heartbeat to allow table translation between image generation. Using ECG gating, the scanner acquires data in a nonstop, helical mode while an independent ECG trace is generated at the same time. Images are thus acquired both during systole and diastole. Subsequently, the ECG trace is mapped alongside the acquired image data so that one can deduce the systolic and diastolic images.
To summarize, ECG triggering uses the ECG to acquire data and is prospective, while ECG gating is used to reconstruct data and is retrospective. Also, ECG triggering may be used for coronary calcification scoring and aortic root imaging, whereas ECG gating is required for coronary artery CTA. 2
Contrast
The contrast dynamics within the coronary arteries reflect those in systemic elastic arteries elsewhere, with a rapid rise to peak, short duration plateau, and relatively rapid drop in concentration after the peak. A peak attenuation value of 2 to 300 HU must be achieved in the left ventricular outflow tract for clinically useful coronary CTA images to identify patency and noncalcified plaque (Figure 2). All postprocessing segmentation tools assume a level of contrast differentiation so that the vessel lumen may be defined. In our department, 100 mL of nonionic contrast material (320 mgI/mL) is given by power injection at a unimodal, constant rate of 3.5 to 4 mL/sec through an antecubital vein. With the saline chaser technique, the contrast bolus is followed immediately with a 20-mL bolus of saline by power injection from a second syringe in a dedicated dual-head injector. The underlying principle is that the chaser captures redundant contrast in the arm, innominate vein, and the superior vena cava, washes out the beam-hardening density within the right atrium, and increases the density values within the left heart and coronary arteries by tightening the bolus and raising its concentration. 1,3 There is limited scientific data on the role of the saline chaser, and its use remains under review without universal recommendations. I have found its performance variable with 16-detector scanning, and I am currently looking at its use with 64-channel MDCT.
Although in the past we have used empiric timing of a 25-second delay with 16-detector scanning with good reproducibility and consistent ventricle en-hancement, the shorter data acquisition time of a 64-detector CT requires timing or test-bolus techniques that are the same as those applied to aortic imaging.
Protocols
The main coronary artery protocols in use are calcification scoring and coronary CTA. The former is performed using a low-dose, noncontrast, prospectively triggered, nonhelical technique, with relatively large slice collimation (~3 mm). Coronary CTA is performed with small slice collimation, relatively low pitch, and slow table translation that allow oversampling of data. The smallest slice widths are defined by the smallest detector width chosen. A 0.75- to 1-mm slice collimation produces good coronary 3-dimensional (3D) data sets, though the smaller slice widths may carry a penalty of higher noise. Some institutions advocate performing coronary calcification scoring in all patients and, perhaps, not proceeding to coronary CTA when a heavy burden of calcified plaque will likely make the study uninterpretable.
Patient dose
The ECG-triggered mode is a relatively low-dose technique (~3 mSv), as data is acquired only during the diastolic phase of the cardiac cycle. The ECG-gated mode is a high-dose technique (~7 mSv), as it acquires data throughout the cardiac cycle in both systole and diastole with low pitch and data oversampling. This dose approximates that of conventional digital subtraction coronary angiography. Larger detector arrays do decrease the relative contribution of the wasted penumbra effect at the end of the detector arrays. ECG modulation is a technique that lowers the radiation exposure during the systolic phase of imaging, and then increases the radiation dose during the diastolic phase when clinically useful imaging is being acquired. 1,4 It behooves us to apply the lowest reasonable dose, in particular, when the CT is used as a screening tool.
Data processing
Data reconstruction
Coronary CTA data is reconstructed using multidetector-row interpolation. The entire 360˚ of gantry rotation is not required for image reformation. Using partial scan reconstruction with 180˚ of the rotation, the temporal resolution may be halved. Due to the overlapping data sampling, a smaller arc of gantry rotation from multiple adjacent cardiac cycles may be summed to create a single axial image (ie, segmental reconstruction) with increased temporal resolution. In this setting, the temporal resolution is equal to the gantry rotation time divided by twice the number of segmental reconstructions employed. One should note than when more than 2 cardiac cycles are used, the image quality will deteriorate as one samples data beyond the field-of-view of interest. 2,3
An entire set of axial images of the heart from the base to the apex is made for each of a series of time intervals within the each cardiac cycle: 10%, 20%, 30%, etc., of the R-R interval (Figure 3). Of course, this assumes a sinus rhythm with heartbeats of equal duration, where the 60% R-R image of the top of the heart, made from the first heartbeats, corresponds in time and cardiac cycle to the 60% R-R image of the bottom of the heart constructed from the last heartbeats. Thus, one has images in the most systolic and diastolic phases and those in between. It is worth noting that there is both interpatient and intercoronary variation. That is, the most motionless set of images for 1 patient may be 70%, while this set may be 60% for another patient. Likewise, the left anterior descending (LAD) coronary artery may be most motionless at 60% but the right coronary artery may be most motionless at 70% in the same patient. So there is no "one-size-fits-all," but a routine reconstruction of the 50%, 60%, and 70% reconstructions will suffice for most patients.
Postprocessing
Once the data sets have been generated, postprocessing must be applied to segment the helical volume and harness the information contained therein. All postprocessing tools for coronary calcification scoring detect calcification by choosing those sites within the field-of-view that have density values above that of nonenhanced blood. Region growing seeds then may select adjacent pixels with calcification until all calcification is detected. All platforms allow one to enumerate the number of lesions in each named vessel. Though all produce the Agatston score, this has been largely superseded by the mass and volume of calcification present, which are thought to be more objective and reproducible.
Routine axial planar images still play a vital role in overall review. Multiplanar reconstruction (MPR) and curved multiplanar reconstruction (CMPR) techniques have little role to play in coronary imaging. The coronary arteries do not conform to any single plane, and curved plane construction is too subjective for defining the endoluminal center point for such small vessels. However, combined with tools that automatically find the center of the vessel (center-line tools) and with vessel-straightening tools that undo the tortuous curves, CMPR can have value. 2 We have generally found these tools to be useful only in relatively larger and well-opacified vessels with minimum calcification.
Maximum-intensity projection (MIP) is a simple projectional-type technique that depicts all density values above a certain threshold. It requires interactive real-time motion to generate perspective but does not require intensive computer power. Slab MIPs are a quick and effective means to sequentially review the coronary arteries and depict stenoses. This tool performs well even in the presence of calcification, which can be separated using adjusted window settings (Figures 4 through 6).
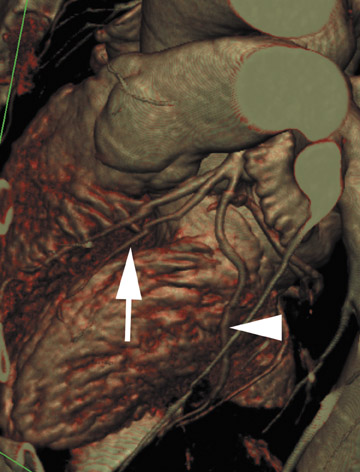
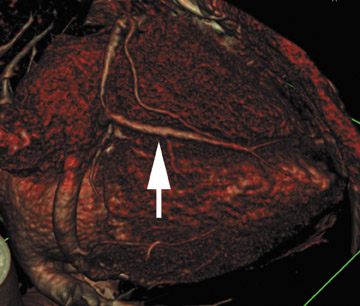
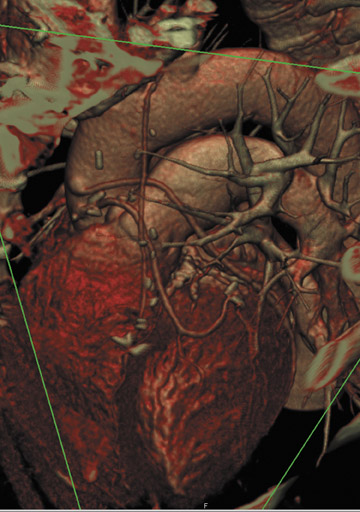
Volume rendering (VR) represents the most advanced form of 3D postprocessing. It is of high fidelity to the acquired data set, preserving all the density values within the voxels. Using histogram trap-ezoids with various user-defined settings of opacity, brightness and color presets may be applied to create attractive coronary images (Figures 7 through 9). However, one must interpret volume rendering with caution, as many of the user-adjusted variables may dramatically alter the size of the vessel lumen. Though VR can be used to illustrate vessel opacification, stenoses, and course, MIP is the better choice to quantify lumen change. 1,5,6
Clinical application and interpretation
Calcium scoring
Although coronary calcification scoring as a surrogate marker for cardiac risk factors has some advocates, it also has many equally loud detractors. 6 Some researchers do not believe in the role of coronary calcification, and some do not believe in the use of mechanical CT for calcification scoring. In the early development of MDCT, there was an argument that calcification scoring should be performed only on EBCT scanners where the original coronary work was done. Such arguments have been largely laid to rest by comparison studies with MDCT and the proven reproducibility of MDCT.
The reality is that scoring use continues to grow rapidly in the cardiology and radiology community as we await the outcome of some large, long-term trials here and in Europe. We know that calcification in the coronary arteries is pathognomonic for the presence of atherosclerotic disease, though its absence does not equate with the absence of plaque. A negative calcification score does suggest that an acute coronary event is unlikely in the near future, and it has been noted that patients presenting with atypical chest pain may be evaluated for noncardiac causes in the setting of a negative coronary calcification scan. When present, the risk of a coronary event is related to the burden of calcification observed.
However, the prevalence of calcification is far greater than the prevalence of coronary events and, at this time, there is no threshold amount of calcification above which coronary events can be accurately predicted. The coronary calcification tells us nothing about plaque stability and the acute event may occur at a site remote from the calcification. 1 A few isolated reports have suggested that coronary calcification may be used to monitor the response of plaque to cholesterol-lowering agents, though the results have never been replicated. Some of the greatest interest has centered on coronary calcification as an independent risk-factor modifier. 7,8 There are those who have suggested that it may have more discriminatory value than age in the Framingham formula when applied for those >55 years of age. I subjectively describe larger burdens of plaque and, when possible, describe when deposits are eccentric or more central. The final score analysis is sent to the referring clinician, and I do not attempt to deduce the clinical or management implications; at this time, these are best handled by those with a comprehensive grasp of the patient's disease.
CTA
First, it is important to appreciate which patients should not have coronary artery CTA. Conventional coronary angiography remains the standard of care for coronary artery evaluation. Time is critical for those presenting with a threat to myocardial viability. Patients presenting with a high pretest probability of unstable disease should still go on to conventional imaging in cases in which catheter-directed therapeutic intervention is highly likely or if emergent surgical intervention is anticipated. Patients who have a coronary calcification study that reveals a large burden of disease should be reconsidered for CTA, as the ability to accurately and comprehensively detect and quantify all stenoses may be limited.
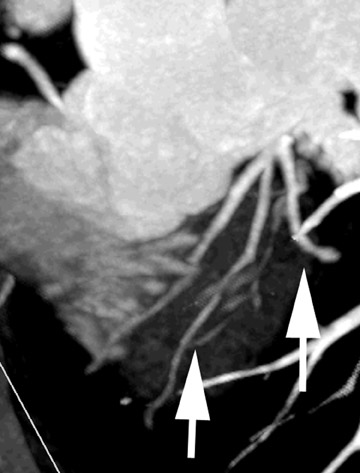
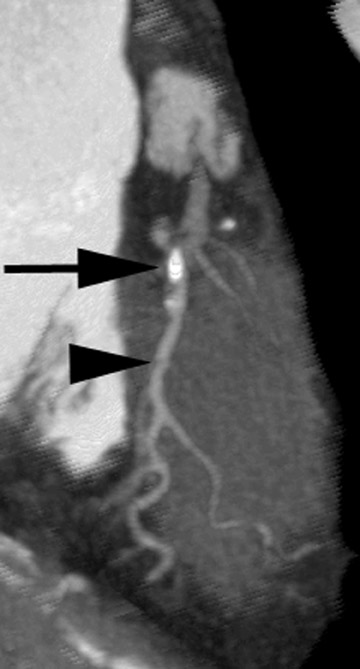
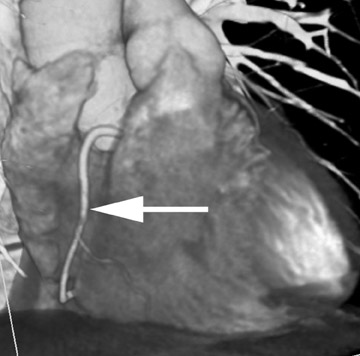
Coronary MDCT is a reasonable test to evaluate stenoses in those with a low pretest probability of disease where the negative-predictive value of the study is very high. It has also been shown to be of value in depicting aberrant coronary artery anatomy by accurately defining their site of origin, size, and course. 3,9 Such vessels often defy definition by conventional projectional technique. It is of proven value in evaluating the patency of bypass grafts (Figure 10), which are relatively motionless vessels and can be imaged with ease, although one should note that we are limited in evaluating the anastamosis and small-vessel disease beyond the anastamosis. 10 A CTA luminogram does not provide information on flow dynamics and usually cannot reveal collateral formation. Its use in establishing coronary stent patency is limited and has been limited by beam hardening in its sensitivity to early restenosis. 5
Based on our experience, 70% to 80% of cases are satisfactory studies with acceptable visualization of 70% of the native vessel lengths using 16-detector CT. Most vessels ≤2 mm can not be routinely visualized. It would appear that though the line pair resolution of 64-detector CT has not significantly changed, the improved temporal resolution and bolus capture may increase reproducibility, accuracy, and vessel visualization.
As with all CTA, there is not as yet any standardization of coronary artery CTA technique or interpretation. The following discussion reflects only one approach. There are, however, American Heart Association and American College of Cardiology guidelines on conventional angiography interpretation that may serve as a guide, since conventional angiography is as yet the gold standard, albeit an imperfect one. 11 It is important that the basic anatomy is understood and the vernacular of cardiology interpretation is followed.
Initial image review is directed at noncardiac pathology with axial planar images. Though the heart images are reconstructed with a smaller field-of-view, it is important to study the entire field-of-view images in the axial plane to exclude incidental lung or mediastinal neoplasms. Initial cardiac review is directed at noncoronary pathology, including pericardiac disease, cardiac masses, and valvular changes. The shape and size of ventricles is commented upon as well as any attenuation changes. Starting with 3D VR, coronary artery interpretation begins with documenting the vessel origins, course, and dominance. With knowledge of the vessel course, slab MIP is applied to each vessel, in turn, to assess for stenotic disease. As with barium studies, readers will quickly develop their own systematic way of reviewing all of the vessels in turn. The printed images include the standard cardiologist views of the right coronary, LAD, and circumflex arteries. These are supplemented with unique 3D views that depict the individual patient's disease to best effect. There are no proven tools that accurately measure coronary artery stenosis, and as with conventional angiography, subjective percentages may be applied. One approach is to subjectively describe lesions <50%, 50% to 75%, and >75%. With larger and well-opacified vessels, one can apply diameter measurement tools. The site, length, and multiplicity of the lesions may be estimated, along with the proximity to major branch points. With high-grade disease, the presence of distal vessel opacification is noted. A full cardiac evaluation takes an average of 20 to 30 minutes to interpret.
The final report includes a description of the data acquisition and postprocessing tools that were employed. There is a sequential description of noncardiac, noncoronary cardiac, and coronary artery findings. Referring clinicians receive a photographic printout or digital image of calcium scores and coronary artery CTA.
Newer developments
Recently, CT has been moving into some traditional areas for MRI, including plaque imaging and functional cardiac imaging. Some early work has suggested that coronary artery plaque may be characterized by CT attenuation values with potential to discriminate sites of stable and unstable disease. Such findings have been correlated with intravascular ultrasound, but the work remains in its early stages. 3,12
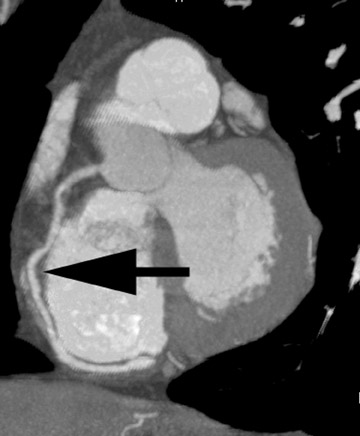
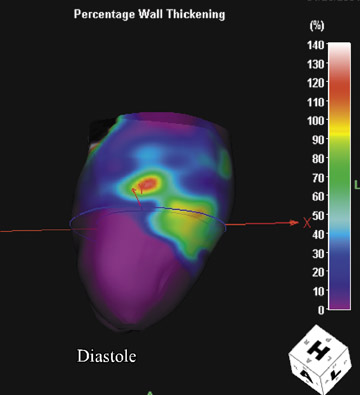
Information on the entire cardiac cycle is contained within the retrospective data set. From this data, one may obtain dynamic chamber volumes, wall thickness, and wall thickening information. Using cine-loops and so-called 4-dimensional images, one may depict the chamber and valve changes throughout the cardiac cycle. 5 One may qualitatively assess regional wall motion and dyskinesis and objectively quantify ejection fraction and stroke volume. Such findings have found good correlation with MRI and provide useful supplemental information in patients presenting for cardiac coronary artery evaluation (Figures 11 through 13). 10
Conclusion
The advent of MDCT has introduced an exciting dimension to existing radiology practice. With the latest hardware and software refinements, cardiac CT imaging is relatively straightforward and simple to perform and interpret. Perhaps this is best seen by the rapid progress of nonradiologists in this area. Though it remains an emerging technology, it is being applied and developed in clinical practice at both academic and private centers. As sites implement MDCT technology, coronary CTA should be a part of routine body imaging for all radiologists. One cannot, of course, assume the new role of coronary artery imaging without challenges. It requires a special investment of time and interest as we break new ground, and it has not reached the fluidity and workflow efficiency of routine body imaging. It does stretch existing manpower shortages, and any future application in the emergency room on-call will present further challenges. However, scanner manufacturers are working hard to provide more user-friendly tools for scanning and interpretation and are slowly moving from qualitative, subjective assessment to objective, quantitative assessment.
Related Articles
Citation
CT scanning of the coronary arteries: How to do it and how to interpret it. Appl Radiol.
October 6, 2005