Biliary tract emergencies: What the radiologist should know
Images




This article is accredited for one SA-CME credit. Visit appliedradiology.org/SAM2 for full SA-CME information.
The biliary tract is subject to a spectrum of pathologic conditions which require urgent clinical management. Some of these are due to biliary obstruction, such as jaundice and acute cholangitis. Others are traumatic and iatrogenic complications such as biliary leaks, hemobilia, and malfunctioning biliary drains/stents. Selection of the optimal imaging modality and accurate interpretation of imaging findings facilitates timely and accurate diagnosis and helps guide therapeutic interventions. The radiologist and interventional radiologist thus play a crucial role in the evaluation and management of these conditions. This article will focus on the pertinent imaging features of acute biliary tract disorders involving the intra- and extrahepatic bile ducts, excluding the gallbladder, as well as available radiologic interventions for the management of these conditions.
Biliary obstruction, stasis, and infection
Biliary obstruction and biliary dilatation has various etiologies, including choledocholithiasis, biliary strictures, malignancy, and parasitic disease. Evaluation for biliary obstruction is usually prompted by patient symptomatology and/or cholestatic liver enzyme abnormalities (elevation in serum direct bilirubin and disproportionate elevation in alkaline phosphatase relative to aspartate aminotransferase (AST) and alanine aminotransferase (ALT)).
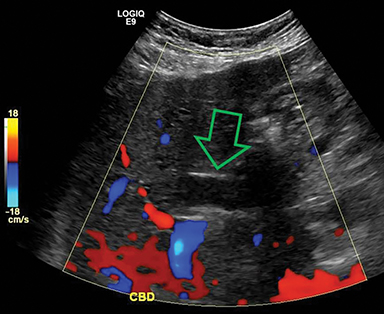
Right upper quadrant transabdominal US can reliably detect biliary duct dilation and in most cases is an appropriate first line examination.1 A common bile duct diameter greater than 7-8 mm is generally indicative of bile duct obstruction in patients without prior cholecystectomy, although some go as low as 6 mm.2 Intrahepatic bile ducts should not exceed 2 mm diameter, or less than 40% of the caliber of the accompanying portal venous branch.2,3,4 Visualization of a common bile duct (CBD) stone on US is the most reliable predictor of choledocholithiasis at subsequent endoscopic retrograde cholangiopancreatography (ERCP) or surgery.5 However, although good for evaluating biliary dilatation, transabdominal US but has relatively poor sensitivity for detection of CBD stones, partly because of difficulty visualizing the CBD.6
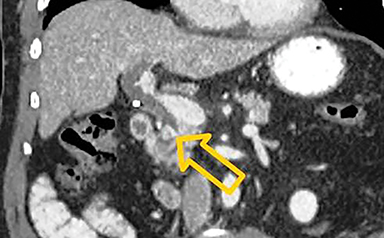
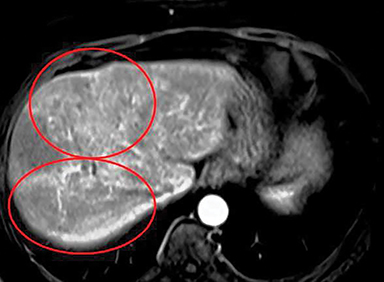
CT is useful for evaluation of biliary ductal dilatation and the measurements used in CT are applicable, but it is only moderately sensitive for detection of choledocholithiasis (with reported sensitivities between 25-90%). Only 20% of stones are high attenuation and up to 24% are isoattenuating to the surrounding bile (Figure 1).7,8 Narrow window settings and coronal reconstructions may help accentuate the stone from adjacent bile or soft tissue.9
Magnetic resonance cholangiopancreatography (MRCP) and abdominal MRI are highly accurate for imaging the biliary tree and is useful in multiple obstruction settings. For instance, it is useful for patients with obstructive jaundice in whom CT and ultrasound findings are inconclusive; when underlying mass or biliary tract neoplasm is suspected; or for evaluation of suspected ascending cholangitis and associated complications (Figure 2).3 Since it is noninvasive, MRCP avoids the potential complications of endoscopic retrograde cholangiopancreatography (ERCP) and is especially useful in patients with surgically altered biliary anatomy not amenable to ERCP (eg, those with biliary-enteric anastomosis).10,11 ERCP is now largely reserved for therapeutic purposes.3,12
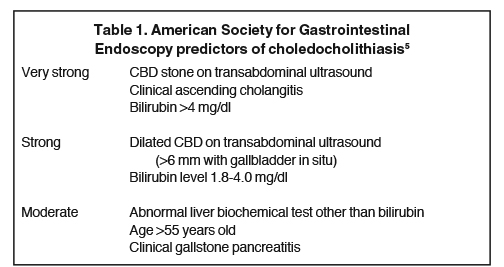
The American Society for Gastrointestinal Endoscopy has proposed a risk-stratified management algorithm to determine which patients with suspected choledocholithiasis would most benefit from further imaging based on clinical predictors at initial evaluation with transabdominal US.5 The risk factors are divided into very strong, strong, and moderate (Table 1). Additional biliary imaging with MRCP or endoscopic ultrasound (EUS) may be most helpful in those at intermediate probability (10-50%) of choledocholithiasis – patients with only one “strong” predictor and/or at least one moderate predictor – to determine potential need for endoscopic stone extraction. Given the frequent need for therapeutic intervention in patients with high probability of choledocholithiasis – those with any “very strong” predictor or both “strong” predictors – preoperative ERCP or operative cholangiography is suggested instead.
Ascending cholangitis
The problem with biliary obstruction is that the decreased biliary flow allows ascent of bacteria from the duodenum. Biliary obstruction may also lead to hepatovenous reflux and subsequent bacteremia.13,14 Ascending cholangitis is associated with high mortality and requires emergent biliary decompression. Imaging in suspected ascending cholangitis helps confirm the presence, level and cause of obstruction and to identify potential complications such as suppurative cholangitis, parenchymal abscess, portal vein thrombosis, and biliary peritonitis.3
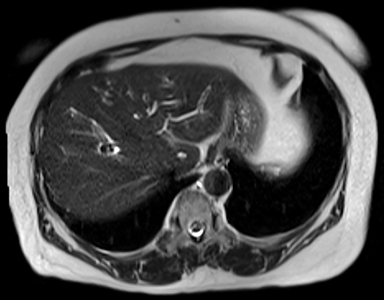
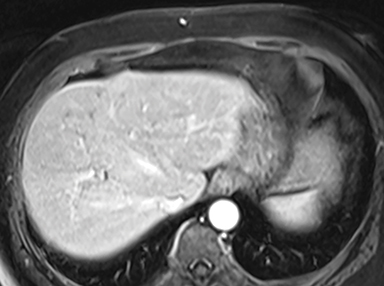
MRI imaging characteristics of ascending cholangitis include central intrahepatic biliary dilation with smooth ductal wall thickening and enhancement. Associated parenchymal inflammatory changes include patchy or peribiliary parenchymal enhancement (most apparent on arterial phase postcontrast imaging) and geographic, wedge-shape T2-hyperintense segments of inflamed tissue around the involved bile ducts (Figure 3). In acute suppurative cholangitis, dilated bile ducts filled with echogenic purulent material are observed on ultrasound; dense biliary contents are seen on CT.10 Biliary contents will appear low signal relative to liver on T2-weighted MRI and intermediate signal on T1-weighted MRI.15 A uni- or multiloculated collection with capsular or rim enhancement is characteristic for abscess formation on CT and MRI; coalescence of adjacent abscesses may result in a cluster sign.16
Biliary injuries: Bile leaks and hemobilia
Biliary complications can result from either traumatic or iatrogenic bile duct injury and encompass a spectrum of often coexisting entities, including retained stones, hemorrhage, hemobilia, bile leaks, bile duct ligation and strictures.
Traumatic bile leaks
Biliary tract injury is a rare complication of abdominal trauma, with a reported prevalence of 2.8–7.4% in patients sustaining blunt hepatic injury.17,18 Injuries to the extrahepatic bile ducts usually result from acute deceleration and tend to occur at sites of anatomic fixation, such as the intrapancreatic portion of the CBD. Injuries to the intrahepatic bile ducts may be seen in the setting of parenchymal liver injury.
Traumatic complications such as biloma or biliary peritonitis, can manifest days to weeks after initial trauma.19 Because bile is sterile and absorbed by the peritoneum, symptoms may not arise until the bile becomes superinfected. Patients frequently exhibit nonspecific progressive symptoms such as abdominal pain, nausea, vomiting, and, rarely, acute abdomen with peritoneal signs. Serum biochemical tests may reveal rising or persistently elevated serum bilirubin levels, sometimes accompanied by jaundice.
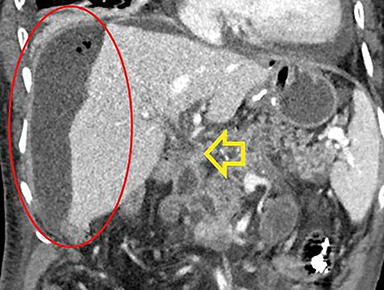
CT is often the first-line imaging modality in the setting of trauma. Findings of bile duct injury are relatively nonspecific, and diagnosis often requires a high level of suspicion on the part of the radiologist. Secondary findings such as liver lacerations, focal peri- or intrahepatic fluid collections, ascites, and associated solid organ injuries may be the only indicators of bile duct injury at initial imaging. Follow-up imaging is often helpful; progressive growth of a well-circumscribed, low-attenuation perihepatic or intraparenchymal fluid collection suggests a biloma; persistent or increasing low-attenuation intraperitoneal fluid raises concern for bile leakage; peritoneal thickening and hyperenhancement may indicate biliary peritonitis20
Ultrasound is primarily utilized for follow-up of findings such as bilomas, but can be used to screen for the presence or absence of perihepatic and intrahepatic fluid collections, and ascites.19,21
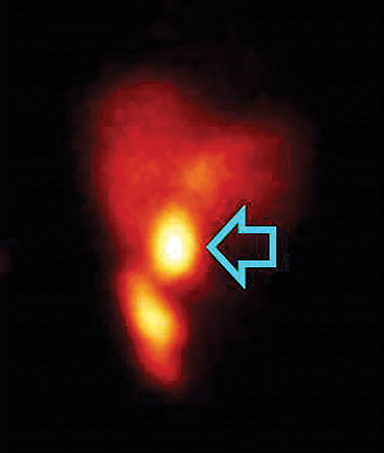
Dynamic hepatobiliary scintigraphy can detect the presence and severity of an active bile leak. Progressive intra-abdominal accumulation of radiotracer that does not conform to the morphologic appearance of the bowel is characteristic (Figure 4).22 Its main limitation is poor spatial resolution, which can be partly overcome with use of SPECT/CT.19.23
Despite the dual therapeutic and diagnostic capabilities of ERCP, the invasive nature and inability to help detect extrabiliary abnormalities limit its diagnostic application as a first-line modality for bile leak detection.24
MRCP with hepatobiliary contrast agents such as gadoxetate disodium (Eovist; Bayer Healthcare Pharmaceuticals, Berlin, Germany) can provide useful functional and anatomic information and in many cases may supersede both scintigraphy (through superior anatomic detail and spatial resolution) and ERCP (by demonstrating peripheral sites of leakage that do not opacify by retrograde injection) in the dynamic evaluation of biliary injury. Delayed hepatocyte phase T1-weighted MR imaging may allow improved characterization of biliary anatomy by providing a higher signal-to-noise ratio in the bile duct than can be achieved with conventional T2-weighted MR imaging.25 Extravasation of contrast material in the liver, perihepatic space, peritoneum, or pleural cavity is indicative of bile leak. Pooling of contrast material within an intrahepatic or perihepatic fluid collection implies direct communication with the biliary tree.26
Iatrogenic bile leaks
Bile leaks have been associated with various surgical procedures, including open and laparoscopic cholecystectomy, hepatic resection, liver biopsy, liver transplantations, ERCP, percutaneous transhepatic cholangiography (PTC), and ablation of hepatic tumors.27,28 Significant postoperative bile leaks have been reported in up to 1% of patients following laparoscopic cholecystectomy, 0.5% of patients after open cholecystectomy and in 2%–25% of patients after orthotopic liver transplantation or hepatic resection.24,29,30 Postoperative bile leaks can go unrecognized due to nonspecific imaging findings and even less specific clinical features, which may be attributed to other more common postoperative complications. Intraperitoneal bile collections may also be difficult to distinguish from other postoperative fluid collections.
Bile leaks typically manifest within one week of surgery, but may not become apparent for up to one month. CT and US may demonstrate free or loculated fluid but cannot reliably distinguish between bile leaks and other postoperative collections. As in the post-traumatic setting, hepatobiliary scintigraphy can provide functional information and demonstrate the presence of free or contained bile leakage. Delayed MRI imaging with hepatobiliary contrast agents may indicate the site of bile leak and help distinguish between fluid collections of biliary and nonbiliary origin by demonstrating contrast accumulation and communication with the biliary tree. MRI/MRCP may also delineate other postoperative complications, such as biliary strictures or retained stones.
Leakage of bile can lead to biloma formation, and these may become encapsulated from inflammation and fibrosis. Although occasionally intraparenchymal, postoperative bilomas tend to form in the gallbladder fossa or porta hepatis and appear as discrete, rounded, hypoechoic (US) or hypoattenuating (CT) fluid collections when uncomplicated (Figure 4).22 On MRI, bilomas appear hypointense on T1W MRI and TW MRI; high T1 and low T2 signal may reflect concentrated layering bile. Identification of a thick enhancing rim or internal complexity should raise suspicion for superinfection or abscess. In the setting of biliary leaks, interventional procedures can facilitate upstream biliary drainage and help stabilize the patient (Figure 5).31-33 They also can provide biliary anatomy proximal to the site of ductal injury for possible surgical intervention. Percutaneous aspiration is also often helpful to confirm a suspected biliary collection.
Hemobilia
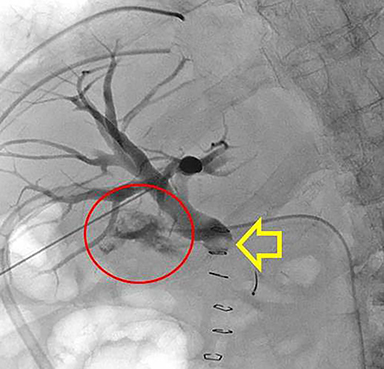
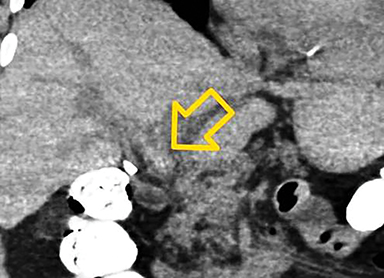
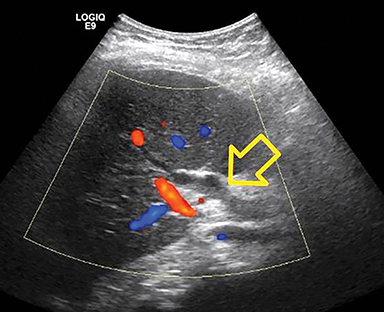
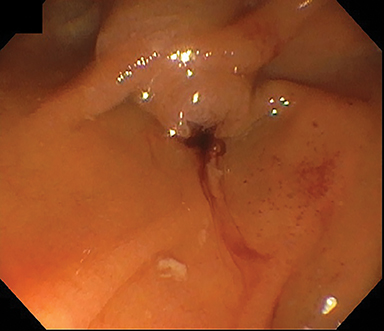
Hemobilia is a rare cause of upper gastrointestinal bleeding which results from a fistulous connection between the hepatic vasculature and biliary ductal system. Most cases develop as a complication of diagnostic or therapeutic hepatobiliary interventions (percutaneous transhepatic biliary drain (PTBD) placement, percutaneous and transjugular liver biopsy, transjugular intrahepatic portosystemic shunt, ERCP, and hepatobiliary surgery).34 Hepatobiliary neoplasms account for the majority of noniatrogenic hemobilia.35 Other etiologies include liver trauma, vascular malformations, inflammatory conditions, calculus disease, hemorrhagic cholecystitis and underlying blood dyscrasias. These patients generally receive an upper gastrointestinal bleeding workup with endoscopy. Visualization of blood arising from the ampulla or the presence of fresh blood in the second portion of the duodenum may indicate a biliary etiology.
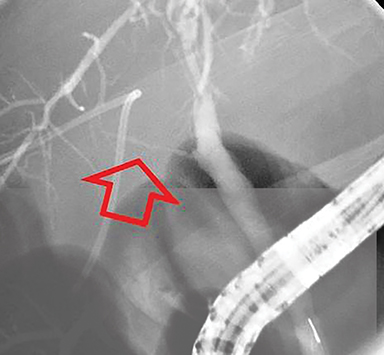
When endoscopy is nondiagnostic, patients often proceed to CT or fluoroscopic angiography. CT angiography (CTA) allows for evaluation of both the arterial anatomy and hepatobiliary parenchyma and is useful in planning endovascular interventions. Direct findings of hemobilia include contrast extravasation into the biliary tract or liver parenchyma.34 Indirect findings may also help localize the bleeding, such as high attenuation hemorrhagic bile or thrombus within bile ducts or gallbladder, pseudoaneurysms, arteriovenous fistulas, vascular malformations, hepatic tumors, or evidence of blunt liver injury.
MRI/MRCP is less frequently indicated in evaluation of hemobilia due to lengthier examination times and suboptimal evaluation of the peripheral vasculature, but can effectively demonstrate blood products within the biliary system. Hemorrhagic bile appears as increased signal on T1-weighted MRI and decreased signal on T2-weighted MR. Blood products within the biliary system usually appear as filling defects on MRCP. Once the site of bleeding is identified, the site can be embolized in the interventional fluoroscopy suite using either microcoils or liquid embolic agents (Figure 6).34 Surgical intervention is often unnecessary, as success of endovascular management at experienced centers approaches 100%.36 Depending on the patient’s situation, percutaneous biliary drainage may also be necessary for successful drainage of biliary obstruction from intraluminal blood products.
Biliary leaks after liver transplant
Biliary complications remain a major source of morbidity after liver transplant, with an incidence of 5-15%, and are usually observed within the early postoperative period (≤3 months after surgery).27,37,38 Potential complications include anastomotic and non-anastomotic strictures, leaks, stones, ampullary dysfunction, biliary necrosis, and cholangitis.
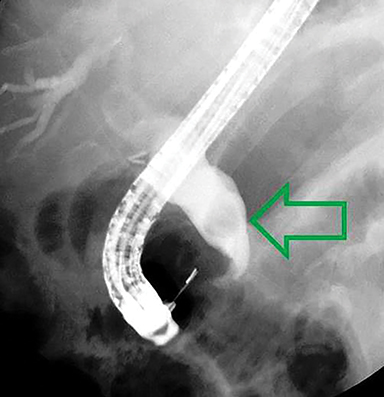
The type of biliary reconstruction is a major determinant of the risk of biliary complications after liver transplant39,40 The most common biliary reconstruction procedure is choledochocholedochostomy: an anastomosis between the donor CBD and the recipient common hepatic duct. With this anastomosis, a T tube is usually left in the duct for approximately six weeks postoperatively. T-tube cholangiography provides better evaluation of the biliary system than MRCP due to better distention of the bile ducts with contrast. The use of T-tubes has been associated with bile leak and cholangitis at the time of their removal, however (Figure 7).38
Choledochojejunostomy, in which the donor CBD is anastomosed directly to the recipient jejunum, is usually performed in patients with pre-existing biliary disease such as primary sclerosing cholangitis, prior history of biliary surgery, or when a size mismatch exists between donor and recipient ducts. Post-transplant bile duct leaks may be due to ischemia, relative downstream obstruction, sphincter of Oddi hypertension, or from T-tube removal, and most commonly occur at the biliary-enteric anastomosis or T-tube exit site. Leaks may manifest as extravasation of contrast material from the T-tube site into the peritoneal cavity on direct cholangiography, or as single or multiple bilomas.41
Initial evaluation of suspected transplant biliary complication should include laboratory evaluation and transabdominal grayscale and Doppler ultrasound. When no T-tube is present, MRI/MRCP, with or without hepatocyte specific gadolinium agents, is the preferred imaging tool for further evaluation of the biliary tree and avoids the potential complications associated with ERCP. ERCP has a high failure rate in patients with Roux-en-Y reconstruction, except when double balloon enteroscopy is available to assess the biliary tree. Percutaneous transhepatic cholangiography is usually reserved for cases in which ERCP cannot be performed.
Conclusion
=Biliary tract emergencies have the potential to result in significant patient morbidity but frequently present with nonspecific and overlapping clinical features, thus presenting unique challenges in diagnosis and management. Imaging in this setting often requires a multimodality approach, particularly in complex or postoperative patients. Ultrasound remains the first-line imaging tool for investigation of suspected biliary obstruction, while MRCP with hepatobiliary contrast agents has emerged as a valuable tool in the evaluation of biliary tract injury. Advances in MRI and MRCP have likewise reduced the requirement for diagnostic ERCP. Appropriate selection and interpretation of imaging studies in acute biliary tract disease can aid in timely and accurate diagnosis and guide management of these conditions.
References
- Lalani T, Couto CA, Rosen MP, et al. ACR appropriateness criteria jaundice. J Am Coll Radiol. 2013;10 (6): 402-409.
- Baron RL, Stanley RJ, Lee JKT, et al. A prospective comparison of the evaluation of biliary obstruction using computed tomography and ultrasonography. Radiology. 1982;145(1):91-98.
- O’Connor OJ, O’Neill S, Maher MM. Imaging of biliary tract disease. AJR Am J Roentgenol. 2011;197(4):W551-8.
- Bowie JD. What is the upper limit of normal for the common bile duct on ultrasound: how much do you want it to be? Am J Gastroenterol. 2000; 95(4):897–900.
- ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9.
- Cooperberg PL, Li D, Wong P, et al. Accuracy of common hepatic duct size in the evaluation of extrahepatic biliary obstruction. Radiology. 1980; 135(1):141–144.
- Patel NB, Oto A, Thomas S. Multidetector CT of emergent biliary pathologic conditions. Radiographics. 2013;33(7):1867-1888.
- Miller FH, Hwang CM, Gabriel H, et al. Contrast-enhanced helical CT of choledocholithiasis. AJR Am J Roentgenol. 2003;181 (1): 125-130.
- Neitlich JD, Topazian M, Smith RC, et al. Detection of choledocholithiasis: comparison of unenhanced helical CT and endoscopic retrograde cholangiopancreatography. Radiology. 1997;203(3):753–757.
- Watanabe Y, Nagayama M, Okumura A, et al. MR imaging of acute biliary disorders. RadioGraphics. 2007; 27(2):477–495.
- Hoeffel C, Azizi L, Lewin M, et al. Normal and pathologic features of the postoperative biliary tract at 3D MR cholangiopancreatography and MR imaging. RadioGraphics. 2006; 26(6):1603–1620.
- Harvey RT, Miller WT Jr. Acute biliary disease: initial CT and follow-up US versus initial US and follow-up CT. Radiology. 1999; 213(3):831–836.
- Siegel JH. Endoscopic sphincterotomy in the management of cholangitits. In: Siegel JH, ed. Endoscopic retrograde cholangio-pancreatography. New York, NY: Raven, 1992:211–215.
- Sung JY, Costerton JW, Shaffer EA. Defense system in the biliary tract against bacterial infection. Dig Dis Sci. 1992;37(5):689-696.
- Håkansson K, Ekberg O, Håkansson HO, et al. MR characteristics of acute cholangitis. Acta Radiol. 2002; 43(2):175–179.
- Haaga JR, Herbener TE. The gallbladder and biliary tract. In: Haaga JR, Lanzieri CF, Gilkeson RC, eds. CT and MR imaging of the whole body. 4th ed. St. Louis, MO: Mosby, 2003:1341–1394.
- Bala M, Gazalla SA, Faroja M, et al. Complications of high grade liver injuries: management and outcomewith focus on bile leaks. Scand J Trauma Resusc Emerg Med. 2012;20:20.
- Kozar RA, Moore JB, Niles SE, et al. Complications of nonoperative management of high-grade blunt hepatic injuries. J Trauma. 2005;59(5):1066–1071.
- Melamud K, LeBedis CA, Anderson SW, et al. Biliary imaging: multimodality approach to imaging of biliary injuries and their complications. Radiographics. 2014;34(3):613-623.
- Yoon W, Jeong YY, Kim JK, et al. CT in blunt liver trauma. Radiographics. 2005;25(1):87-104.
- Chiu WC, Wong-You-Cheong JJ, Rodriguez A, et al. Ultrasonography for interval assessment in the nonoperative management of hepatic trauma. Am Surg. 2005;71(10):841-846.
- Singh AK, Nachiappan AC, Verma HA, et al. Postoperative imaging in liver transplantation: what radiologists should know. Radiographics. 2010;30(2):339-351.
- Banzo I , Blanco I , Gutiérrez-Mendiguchía C , et al. Hepatobiliary scintigraphy for the diagnosis of bile leaks produced after T-tube removal in orthotopic liver transplantation. Nucl Med Commun. 1998;19(3): 229–236.
- Mungai F, Berti V, Colagrande S. Bile leak after elective laparoscopic cholecystectomy: role of MR imaging. J Radiol Case Rep. 2013;7(1):25–32.
- Kantarcı M, Pirimoglu B, Karabulut N, et al. Non-invasive detection of biliary leaks using Gd-EOB-DTPA-enhanced MR cholangiography: comparison with T2-weighted MR cholangiography. Eur Radiol. 2013;23(10):2713–2722.
- Gupta RT, Brady CM, Lotz J, et al. Dynamic MR imaging of the biliary system using hepatocyte-specific contrast agents. AJR Am J Roentgenol. 2010;195(2):405–413.
- Zimmitti G, Roses RE, Andreou A, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg. 2013;17(1): 57–64; discussion 64–65.
- Kapoor V, Baron RL, Peterson MS. Bile leaks after surgery. AJR Am J Roentgenol. 2004;182(2): 451–458.
- Tewani SK, Turner BG, Chuttani R, et al. Location of bile leak predicts the success of ERCP performed for postoperative bile leaks. Gastrointest Endosc. 2013;77(4):601–608.
- Girometti R, Cereser L, Como G, et al. Biliary complications after orthotopic liver transplantation: MRCP findings. Abdom Imaging. 2008;33(5):542–554.
- Lorenz, J M. The role of interventional radiology in the multidisciplinary management of biliary complications after liver transplantation. Tech Vasc Interv Radiol. 2015;18(4):266-275.
- Nikpour, A M, Knebel RJ, Cheng D, et al. Diagnosis and management of postoperative biliary leaks. Semin Intervent Radiol. 2016;33(4):307-312.
- Saad N, Darcy M. Iatrogenic bile duct injury during laparoscopic cholecystectomy. Tech Vasc Interv Radiol. 2008;11(2): 102–110.
- Navuluri R. Hemobilia. Semin Intervent Radiol. 2016; 33(4): 324–331.
- Kim KH, Kim TN. Etiology, clinical features, and endoscopic management of hemobilia: a retrospective analysis of 37 cases. Korean J Gastroenterol. 2012; 59 (4): 296-302.
- Zaydfudim VM, Angle JF, Adams RB. Current management of hemobilia. Current Surgery Reports. 2014; 2(5).
- Friedewald SM, Molmenti EP, DeJong MR, et al. Vascular and nonvascular complications of liver transplants: sonographic evaluation and correlation with other imaging modalities and findings at surgery and pathology. Ultrasound Q. 2003;19(2):71-85.
- Kochhar G, Parungao JM, Hanouneh IA, et al. Biliary complications following liver transplantation. World J Gastroenterol. 2013; 19(19): 2841–2846.
- Davidson BR, Rai R, Kurzawinski TR, et al. Prospective randomized trial of end-to-end versus side-to-side biliary reconstruction after orthotopic liver transplantation. Br J Surg. 1999; 86(4):447-452.
- Pascher A, Neuhaus P. Biliary complications after deceased-donor orthotopic liver transplantation. J Hepatobiliary Pancreat Surg. 2006; 13(6):487-496.
- Fulcher AS , Turner MA. Orthotopic liver transplantation: evaluation with MR cholangiography. Radiology. 1999;211(3):715–722.
Citation
SD F, S K, MA M.Biliary tract emergencies: What the radiologist should know. Appl Radiol. 2019; (4):10-16.
July 31, 2019