Sternoclavicular Physeal Separation
Images


Case Summary
A teenager presented with a brief history of right neck and trapezius pain after colliding with a classmate. On physical examination, the right sternoclavicular joint was tender to palpation and the right sternoclavicular joint was slightly depressed compared with the left side. The radial pulses were symmetric bilaterally, peripheral nerve function was intact.
Imaging Findings
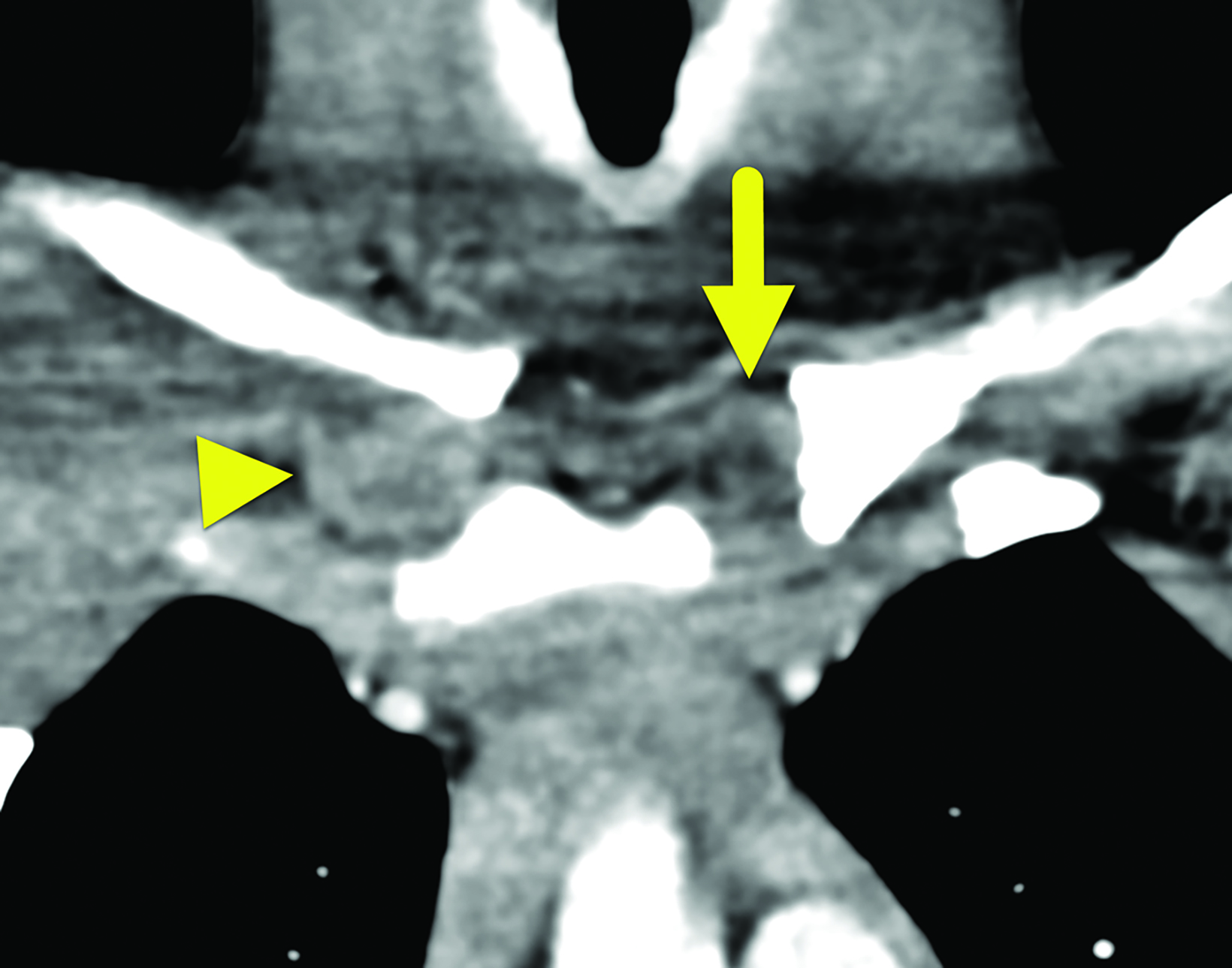
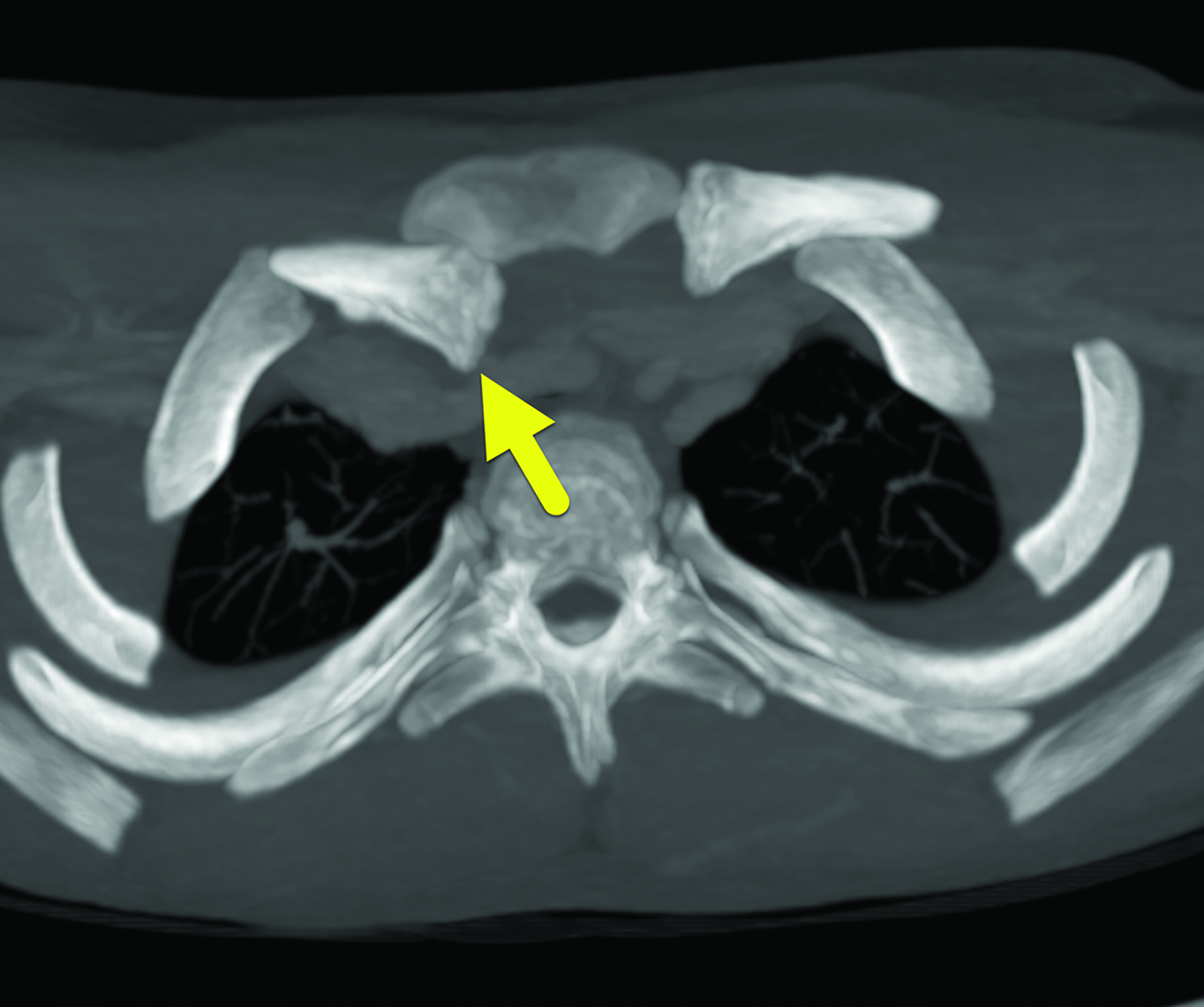
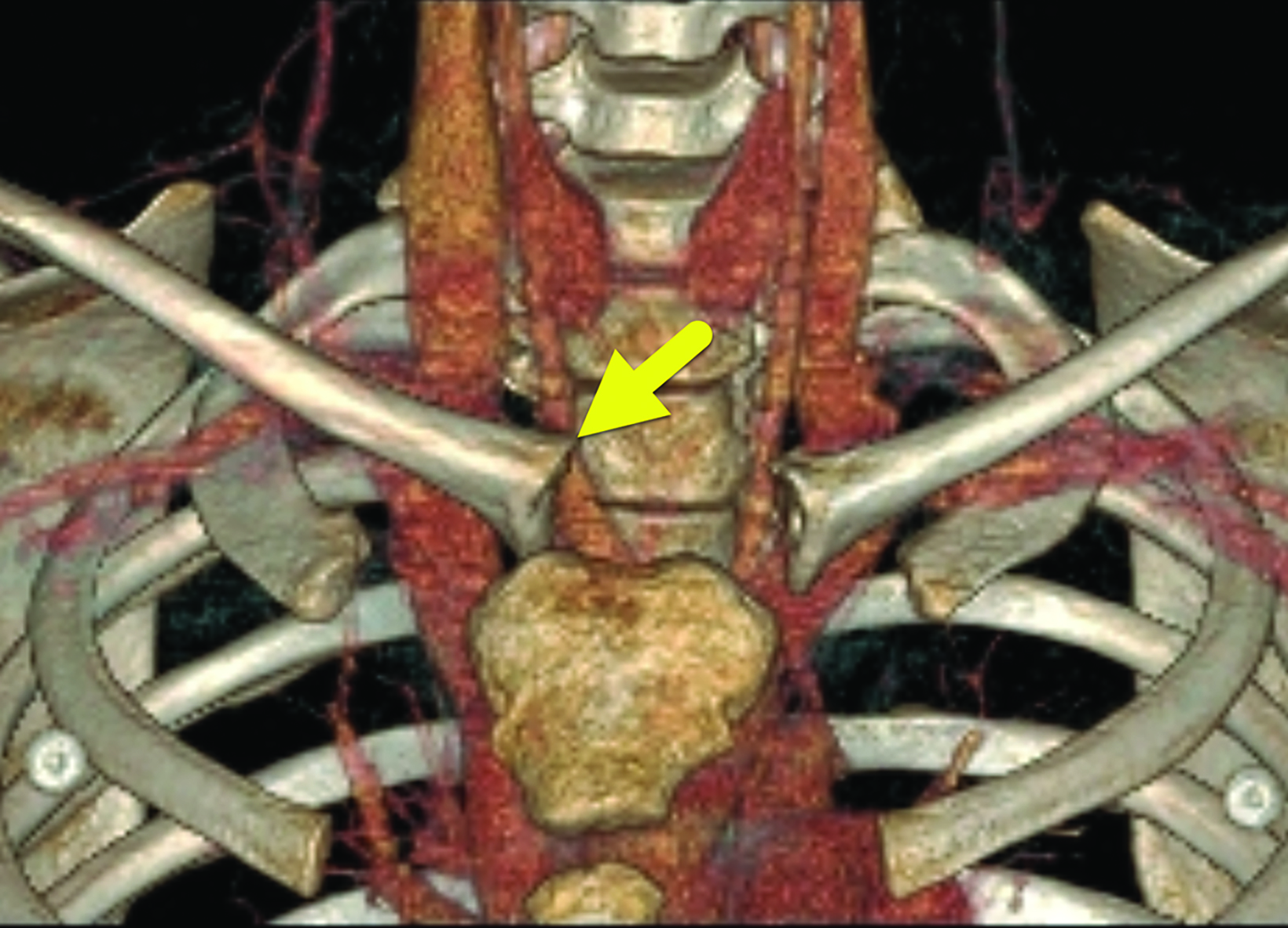
An AP radiograph of the cervical spine (Figure 1) best showed the asymmetry in the appearance of the right and left sternoclavicular joints. A contrast-enhanced chest CT (Figure 2) showed the medial head of the right clavicle to be displaced posteriorly without fracture. There was no narrowing or disruption of the adjacent vessels.
Diagnosis
Sternoclavicular physeal separation
Discussion
Sternoclavicular joint (SCJ) dislocations are rare shoulder girdle injuries that comprise about 3% of all upper limb dislocations.1–3 Because the medial aspect of the clavicle at the SCJ does not fully ossify until 23 to 25 years of life, most injuries are more correctly classified as physeal separations or fractures rather than true dislocations.2,4,5 SCJ injuries are mostly seen in young, physically active males, engaged in contact sports.4
In older patients, anterior dislocation is 9 times more common.However, the incidence of anterior positioning in physeal separation is not known. The most common mechanisms causing posterior dislocations involve lateral compression of a flexed shoulder or direct force to the anteromedial aspect of the clavicle.5
A high degree of clinical suspicion is needed to make the diagnosis of an SCJ dislocation in a timely fashion.2 In general, affected patients present with focal SCJ pain. They classically hold their arm in an adducted position with the elbow flexed and have limited ability to abduct the affected shoulder.2,6 Additionally, patients prefer to rest with a flexed neck on the ipsilateral side and hold their elbow flexed with their contralateral arm.6 Both maneuvers reduce strain on the affected SCJ.
Posterior SCJ dislocations are associated with injuries to mediastinal structures and subclavian vessels.6,7 Knowledge of these injuries is used to help guide imaging protocols. Typically, imaging begins with chest and/or shoulder radiographs.2 Supplemental views are often required for a diagnosis to be made with radiography.
Potentially useful views include the serendipity, Heinig, and Hobbs views.6,8 The serendipity view is the most commonly performed of the three. In this view, a radiograph of the clavicles is obtained with 40 degrees of upward/cephalic tilt of the X-ray beam. If a posterior dislocation of the SCJ is present, the medial aspect of the dislocated clavicle is displaced inferiorly.6 The Heinig view is a lateral view centered on the involved SCJ while the Hobbs view is obtained from an oblique posteroanterior approach.
Today, a contrast-enhanced CT of the chest should be performed whenever a SCJ dislocation is suspected clinically. CT is a sensitive modality to confirm the diagnosis and the extent of injury.2 If there is a high degree of concern for a mediastinal injury, contrast-enhanced CT is used to assess the adjacent vasculature. Multiplanar and 3D reformatting can help distinguish sternoclavicular joint dislocations from physeal separations and can be used to guide surgical planning.2 On CT, the cartilage appears slightly hypodense compared to soft tissue. In a separation, the cartilage remains next to the manubrium while in dislocations, the cartilage appears next to the medial aspect of the clavicle.
Most SCJ dislocations and physeal separations are treated with closed reduction within 7 to 10 days of injury.1,5 Closed reduction requires the patient to be sedated to alleviate muscle spasms and intense pain.1 During reduction, the patient lies supine with a foam pad positioned beneath the injured shoulder to position the shoulder posteriorly.1 As the arm lies perpendicular to the body, sustained pressure is applied until the arm fully extends.1 After treatment, the patient should avoid contact activities for 3 to 4 months.1 Although closed reduction is more frequently recommended, open reduction is recommended if the patient presents outside of the 7-to-10-day window following injury, if there is neurovascular compression, or if the trachea or esophagus are injured.1,5,7
Complications including post-traumatic joint instability, osteoarthritis, and general joint dysfunction may occur.3,8,9 These complications are less common in patients with posterior SCJ dislocations as compared to those with anterior dislocations.1 Our patient was treated with open reduction and internal fixation to stabilize the physeal separation.
Conclusion
The diagnosis of posterior SCJ dislocations requires a high degree of clinical suspicion to make the diagnosis. Chest and sterno-clavicular radiographs are the often the initial step, but CT scans are the diagnostic modality of choice. Early intervention can help prevent long term disability.
References
Citation
KN N, RB T, CM S, D M, AJ T.Sternoclavicular Physeal Separation. Appl Radiol. 2024; (3):17-19.
May 7, 2024