Complications of Anorexia Nervosa
Images




Case Summary
A young adult presented to the emergency department following a fall from bed. On examination, the patient was noted to be severely cachectic with a body mass index (BMI) of 12.9 and a visible deformity of the distal left femur. Patients with a BMI <15 are characterized by the DSM-5 as having extreme anorexia nervosa (AN).1
The patient complained of distal left thigh pain and bilateral foot pain. They reported recently experiencing bilateral foot edema, for which they poked their feet with sewing needles in an attempt to relieve the pressure. Per the patient’s parent, they had an extensive history of hospitalizations for AN-related medical complications. During workup, the patient underwent lower extremity and pelvic radiography, noncontrast CT of the head, chest, abdomen, and pelvis; and MRI of the feet to assess for osteomyelitis.
Imaging Findings
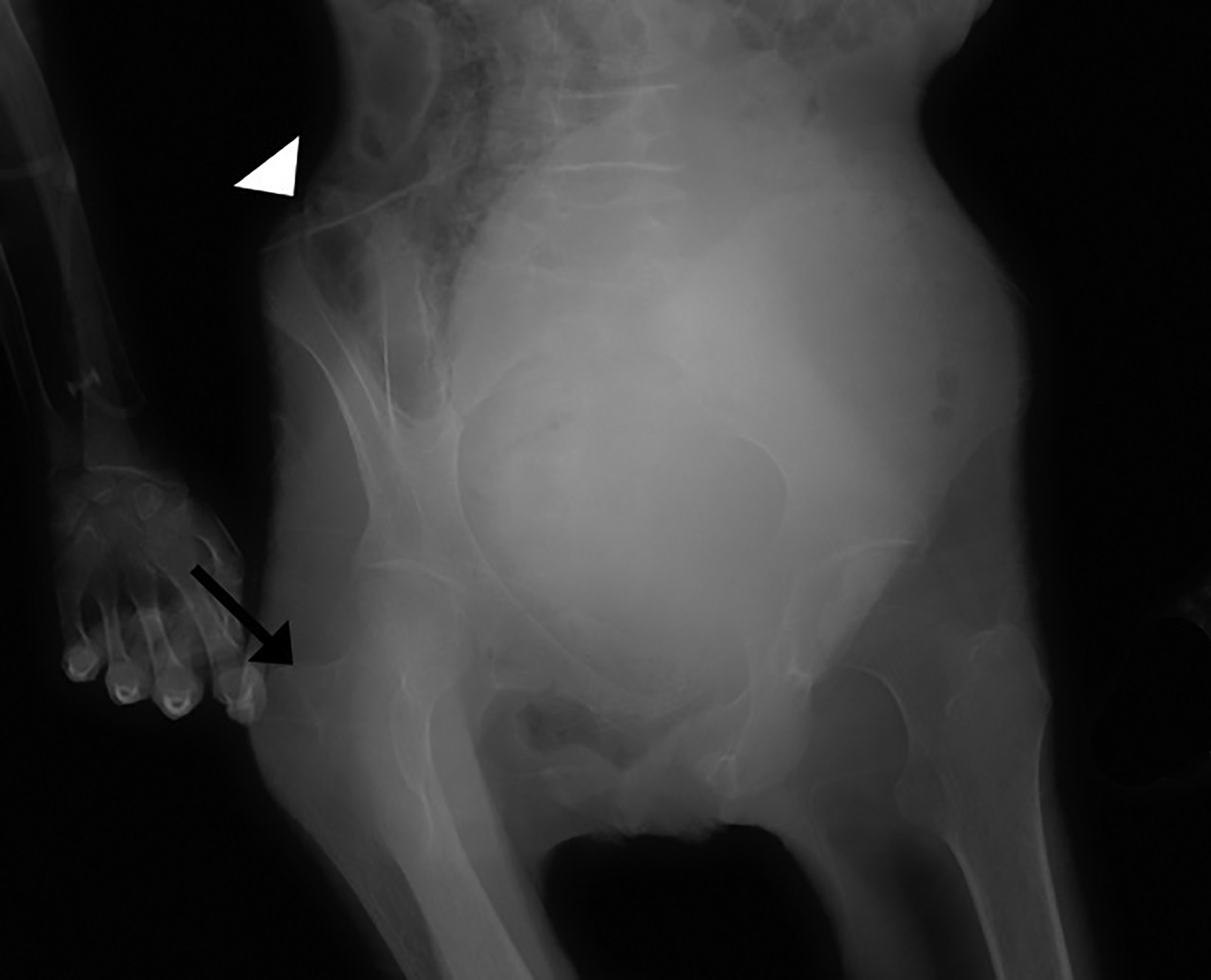
Knee radiography demonstrated an oblique, impacted fracture of the distal femoral metaphysis superimposed on diffuse bony demineralization. Pelvis radiography revealed an acute, comminuted fracture of the right greater trochanter, as well as remote fractures of the bilateral superior pubic rami (Figure 1). Additionally, Rigler sign, air outlining both sides of the colon wall was also seen (Figure 1). Sagittal CT of the spine revealed multiple vertebral body compression fractures (Figure 1).
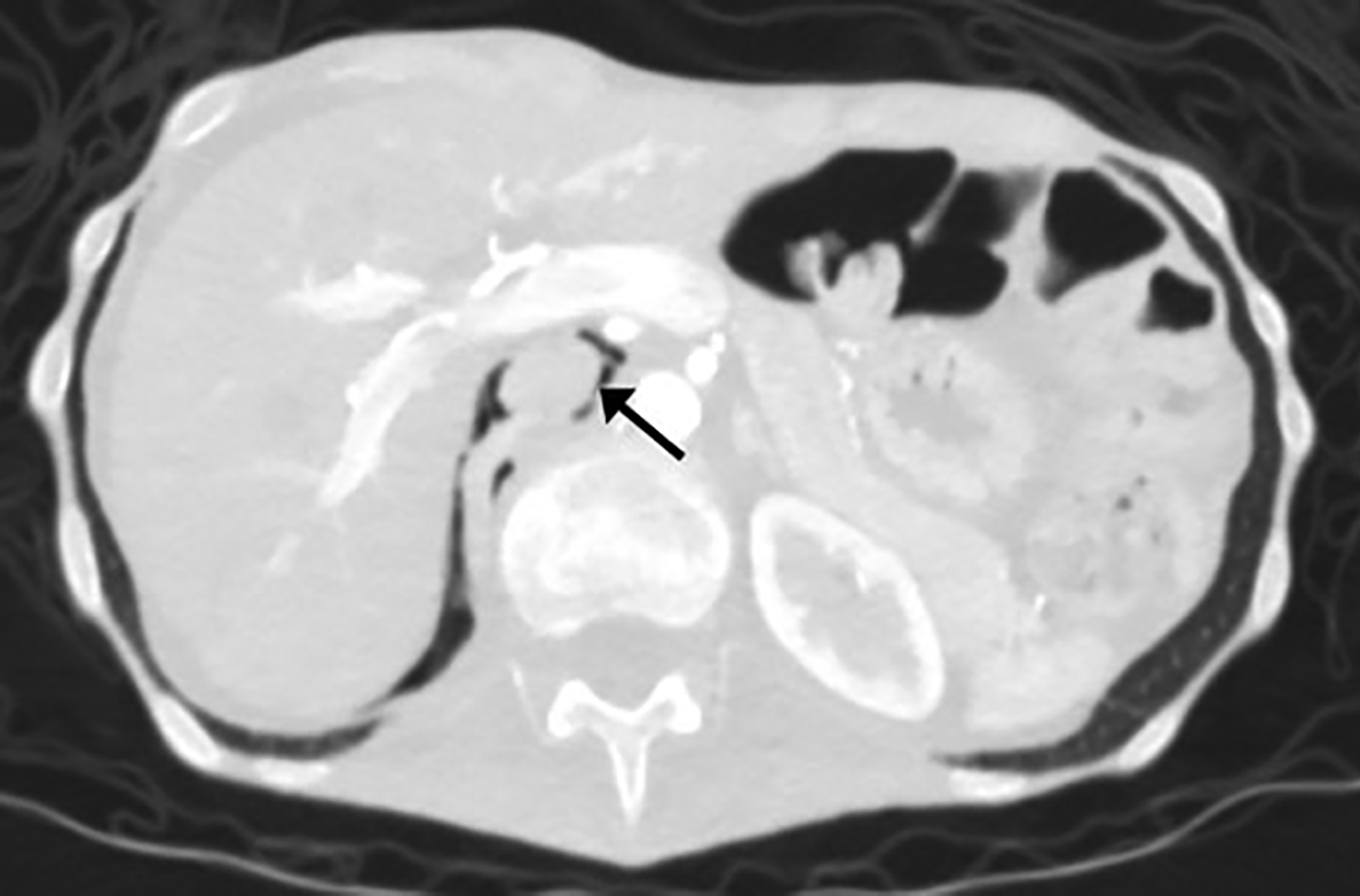
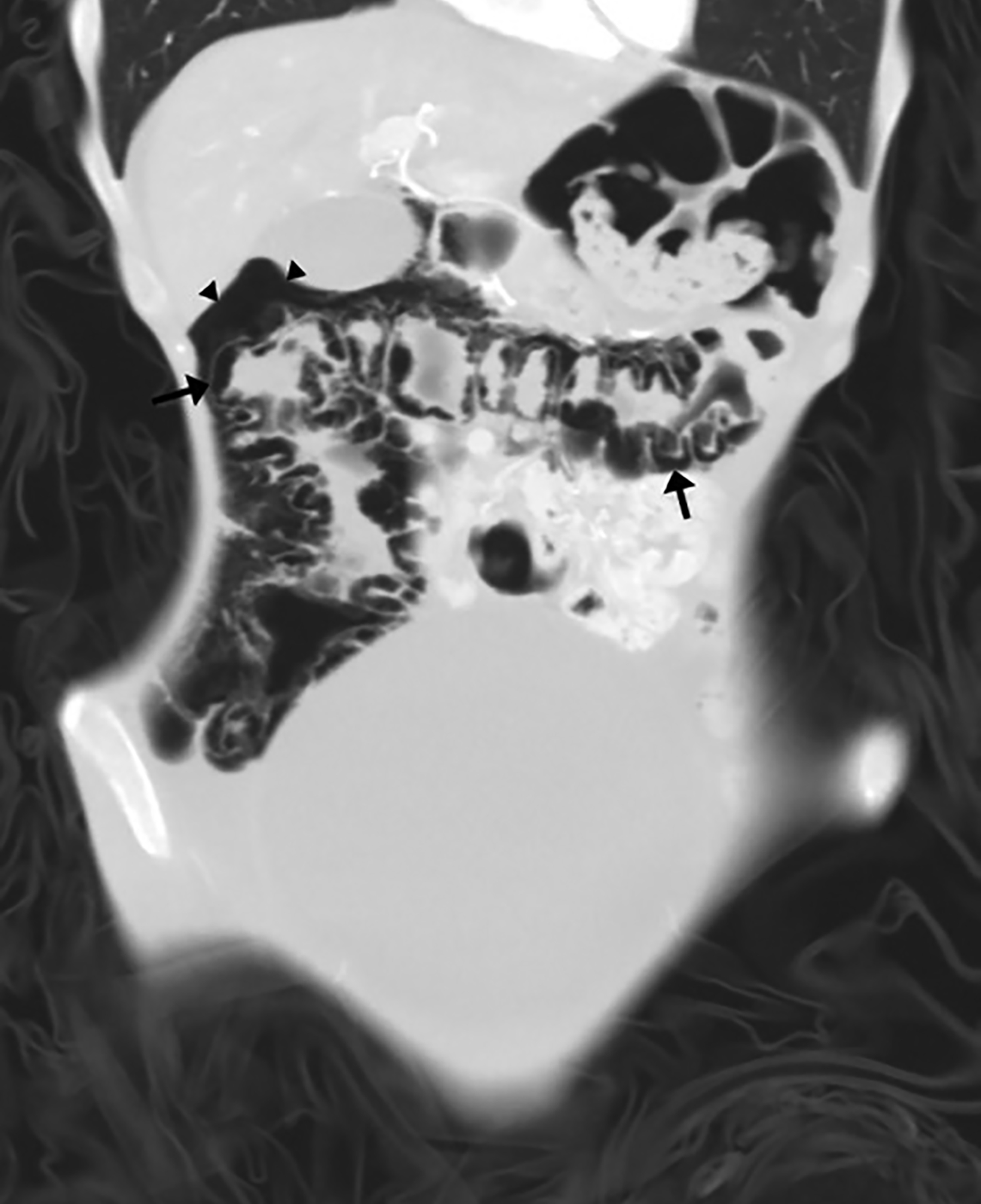
Axial non-contrast brain CT demonstrated diffuse prominence of the ventricles and sulci, out of proportion to the patient’s age (Figure 2). Axial abdominal CT revealed retroperitoneal gas dissecting along the inferior vena cava and into the inferior mediastinum as well as significant bowel-wall pneumatosis of the ascending and transverse colon, and free air within the peritoneal cavity (Figure 3).
Magnetic resonance imaging of the feet revealed premature conversion of red marrow to yellow marrow (Figure 4) but no osteomyelitis.
Diagnosis
Anorexia nervosa complicated by severe bony demineralization, pathological fractures, and pneumatosis intestinalis with pneumoperitoneum.
Discussion
Anorexia nervosa is a unique psychological disorder that leads to severe physiologic derangements across nearly every body system. The sequelae of such alterations can present with a variety of radiographic findings.
The neurological system is quarterbacked by the brain, whose main fuel source is glucose. Without adequate carbohydrate intake, the brain is starved of glucose, leading to overall decreased brain volume. Multiple MRI studies have demonstrated that gray matter volumes are primarily affected in AN; this volume loss has been shown to be reversible with weight restoration.
In cases of AN, malnutrition leaves the body in a constant “fight or flight” state, leading to excessive and continuous release of cortisol. This blocks calcium absorption and disrupts calcium homeostasis, causing decreased bone cell growth and ultimately leading to bone reabsorption and decreased bone mineral density. The earlier the onset of disease before peak bone density is achieved, the more severe the osteoporosis.2 This leads to increased incidence of pathologic fractures. Our patient reportedly fell from a height of no more than three feet and developed multiple acute left lower extremity fractures with more age-indeterminate vertebral compression fractures.
Anorexia nervosa has also been linked to abnormalities in osteoblast and osteoclast progenitor cells in bone marrow. Hormonal alterations with disruption of the hypothalamic-pituitary axis and amenorrhea leads to adipocyte over osteoblast differentiation within the mesenchymal stem cell pool.3 This results in fat deposition and premature conversion from red marrow to yellow marrow.
Severe protein and electrolyte derangements lead to impaired synthetic liver function, which can result in coagulopathy and abnormally low albumin levels. This causes large fluid shifts from intravascular to extravascular spaces, resulting in anasarca, ascites, and pleural effusions, all of which this patient experienced during their hospital stay.
Very few cases of pneumatosis intestinalis have been reported in the setting of AN. As in this patient, the condition is typically found incidentally. It is theorized that the combination of electrolyte imbalance, anasarca, and large fluid shifts in the setting of a low-flow mesenteric circulation state causes nonocclusive bowel ischemia and eventually pneumatosis intestinalis and pneumoperitoneum.4
Conclusion
The images presented in this case demonstrate the unique and multisystem sequelae of extreme AN. Knowledge of such findings form a link behind the body’s physiological response to severe malnourishment and the downstream consequences, some of which are reversible, such as bony demineralization. Careful attention must be paid in identifying such findings to help these patients receive the most appropriate care.
References
- Biller B M, Saxe, V, Herzog D B, Rosenthal, D I, Holzman S, Klibanski A. Mechanisms of osteoporosis in adult and adolescent women with anorexia nervosa. J Clin Endocrinol Metab. 1989; 68(3): 548-554. doi:10.1210/jcem-68-3-548
- Clarke B. Bone marrow changes in adolescent girls with anorexia nervosa. Yearbook of Endocrinology. 2010: 238-240. doi:10.1016/s0084-3741(10)79490-7
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). (2000). doi:10.1176/appi.books.9780890423349
- Hudson J L, Hiripi E, Pope H G, Kessler R C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psych. 2012; 72(2): 164. doi:10.1016/j.biopsych.2012.05.016
- Neychev V, Borruso J. Bowel ischemia and necrosis in anorexia nervosa: a case report and review of the literature. Intl J Surg Case Rep. 2015; 8:141-143. doi:10.1016/j.ijscr.2015.01.035
- Roberto, C A, Mayer L E, Brickman A M, et al. Brain tissue volume changes following weight gain in adults with anorexia nervosa. 2010; Intl J Eating Dis. 44(5): 406-411. doi:10.1002/eat.20840
- Sachs K V, Harnke B, Mehler P S, Krantz M. J. Cardiovascular complications of anorexia nervosa: A systematic review. Intl J Eating Dis. 2015; 49(3): 238-248. doi:10.1002/eat.22481
Citation
RM E, C M, Tahawi, A, KR C. Complications of Anorexia Nervosa. Appl Radiol. 2024;(1):48d-48f.
January 24, 2024