Ureterosciatic hernia
Images

CASE SUMMARY
A 71-year-old woman with a history of hypertension, hyperlipidemia, and atrial fibrillation presented to the emergency department with acute, severe left flank and pelvic pain, nausea, and emesis. She denied hematuria, dysuria, and NSAID use. Vital signs were normal. She had pain with abdominal palpation. Urinalysis demonstrated 1+ leukocytes, 2+ blood, and no casts or infection. Creatinine was elevated from 1.1 to 3.17 mg/dL. Noncontrast CT abdomen and pelvis confirmed the etiology of her pain. One year prior to this admission, she had a similar presentation and was diagnosed with ureteral obstruction causing unilateral hydroureteronephrosis. She was treated conservatively as her symptoms resolved without intervention. On this recent admission, urology recommended cystoscopy and ureteral stenting. Retrograde pyelography demonstrated a tortuous left ureter near the sacroiliac joint. Purulent fluid was drained with guidewire insertion, and a double-J stent was placed. The creatinine declined postoperatively, and her pain resolved.
IMAGING FINDINGS
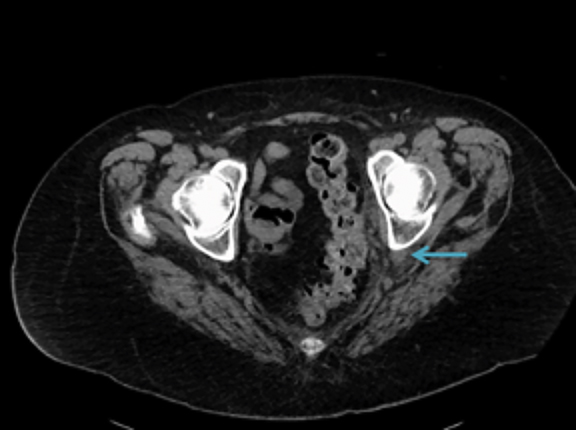
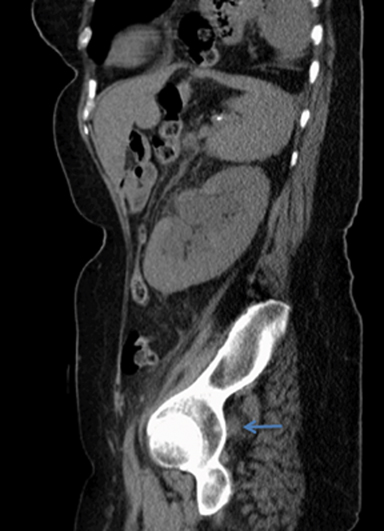
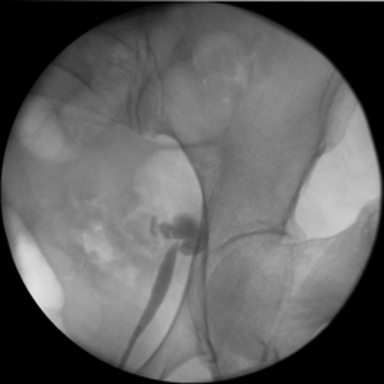
Noncontrast-enhanced CT demonstrated moderate left hydroureteronephrosis and left ureter coursing laterally into the sciatic notch ventral to neurovascular structures with an abrupt change in caliber suggesting impingement (Figures 1). CT three-dimensional reconstruction demonstrated the course of the ureter and its entrapment in the sciatic notch (Figure 3). Retrograde pyelography demonstrated horizontally redundant ureter in the sciatic notch (Figure 2).
DIAGNOSIS
Ureterosciatic hernia
DISCUSSION
Sciatic hernias are the rarest type of pelvic floor herniation with 99 total cases identified through 2008.1 The sacrospinous and sacrotuberous ligaments divide the sciatic notch into the greater and lesser sciatic foramina.1,2 The piriformis divides the greater sciatic foramen into the suprapiriform foramen and infrapiriform foramen.1,2 Sciatic hernias are more commonly suprapiriform, but can also arise in the infrapiriform foramen or the lesser sciatic foramen. Of the reported sciatic hernias, 77% were in women and 37% were in patients 60 years or older.1 Organs that can herniate into the greater or lesser sciatic foramen include ovary (28%), ureter (25%), small intestine (23%), and colon (18%).1,2
The most common location of ureteral herniation is inguinal, whereas sciatic, thoracic, and parailiac hernias are seldom reported.2 Ureterosciatic hernia is exceedingly rare with fewer than 40 cases reported in the literature. Atrophy of the piriformis secondary to hip pathology or neuromuscular diseases likely contributes to this etiology of ureterosciatic hernia.2
Presentation typically includes acute abdominal pain, flank pain, nausea/vomiting, and possible renal pathology secondary to the ureteral obstruction.3,4 The patient described in this case developed acute renal failure and pyelonephritis secondary to the obstruction. However, patients may also be asymptomatic.5
Ureterosciatic hernias cannot reliably be diagnosed with physical examination.2,4 Imaging with CT or pyelography is essential for diagnosis. Anterograde or retrograde pyelography reveals horizontally redundant ureter posterolateral and inferior to the ischial spine.3 This presentation is known as the “curlicue” sign and is pathognomonic for ureterosciatic hernia.3 CT demonstrates the ureter posterior, lateral, and craniad to the ischial spine.6 CT can also reveal hydroureteronephrosis proximal to the hernia secondary to obstruction, which was demonstrated in this case. CT with three-dimensional reconstruction and volume rendering can also be used to confirm the diagnosis and appreciate hernia location before surgical intervention.4
There are various treatment options, depending on the patient’s presentation. The asymptomatic patient can be treated conservatively with observation.5 The symptomatic patient can be treated with ureteral stenting to maintain patency of the affected ureter.5 The stent can be removed after symptoms resolve. If stenting is not successful, symptomatic patients can be treated with ureteropexy or ureteroureterostomy.5
CONCLUSION
Sciatic hernias are a very rare type of pelvic floor hernia. Ureterosciatic herniation should be in the differential when the patient presents with the acute onset nausea/vomiting, colicky flank pain, abdominal pain, and reduced renal function. CT imaging with or without contrast confirms the diagnosis by demonstrating the ureter in the greater sciatic foramen posterolateral to the ischial spine and anterior to the piriformis. Pyelography demonstrating the “curlicue” sign is pathognomonic. This patient had resolution of symptoms and acute renal failure after ureter displacement from the greater sciatic foramen and double-J stent placement.
REFERENCES
- Losanoff JE, Basson MD, Gruber SA, et al. Sciatic hernia: a comprehensive review of the world literature (1900-2008). Am J Surg. 2010; 199:52–59.
- Pollack HM, Popky GL, Blumberg ML. Hernias of the ureter: An anatomic roentgenographic study. Radiology. 1975; 117: 275-281.
- Beck WC, Baurys W, Brochu J, et al. Herniation of the ureter into the sciatic foramen (“curlicue ureter”). J Am Med Assoc. 1952:149: 441–442.
- Loffroy R, Bry J, Guiu B, et al. Ureterosciatic hernia: A rare cause of ureteral obstruction visualized by multislice helical computed tomography. Urology. 2007; 69:385.e1-3.
- Singh I, Patel B, Hemal AK. Robotic repair of a rare case of symptomatic “Ureterosciatic Hernia”. Indian J Urol. 2013; 29:136-138.
- Spring DB, Vandeman F, Watson RA. Computed tomographic demonstration of ureterosciatic hernia. AJR Am J Roentgenol. 1983; 141:579-580.
Citation
D S, K C, AS B, W G, R A.Ureterosciatic hernia. Appl Radiol. 2019; (1):42-44.
February 5, 2019