Ultrasound Predicts Ovarian Cancer
 Ultrasound is an effective predictor of ovarian cancer based on the appearance of lesions and may help women avoid unnecessary surgery, according to a published study in Radiology.
Ultrasound is an effective predictor of ovarian cancer based on the appearance of lesions and may help women avoid unnecessary surgery, according to a published study in Radiology.
Ovarian cancer is the deadliest of the gynecologic cancers, killing about 15,000 women every year in the United States. Characterization of adnexal lesions, or lumps near the uterus, on ultrasound examination is crucial for appropriate patient management, as some adnexal lesions can progress to cancer, while many others are benign and do not require treatment.
“Based on the characteristics that we see on ultrasound, we try to evaluate if a finding needs further workup and where the patient should go from there,” said study lead author Akshya Gupta, M.D., from the University of Rochester Medical Center in Rochester, N.Y. “There is a lot of nuance to it because the lesions can be challenging to assess.”
Current risk stratification systems perform well, but their multiple sub-categories and multifaceted approach may make them difficult for radiologists in busy clinical practices to master.
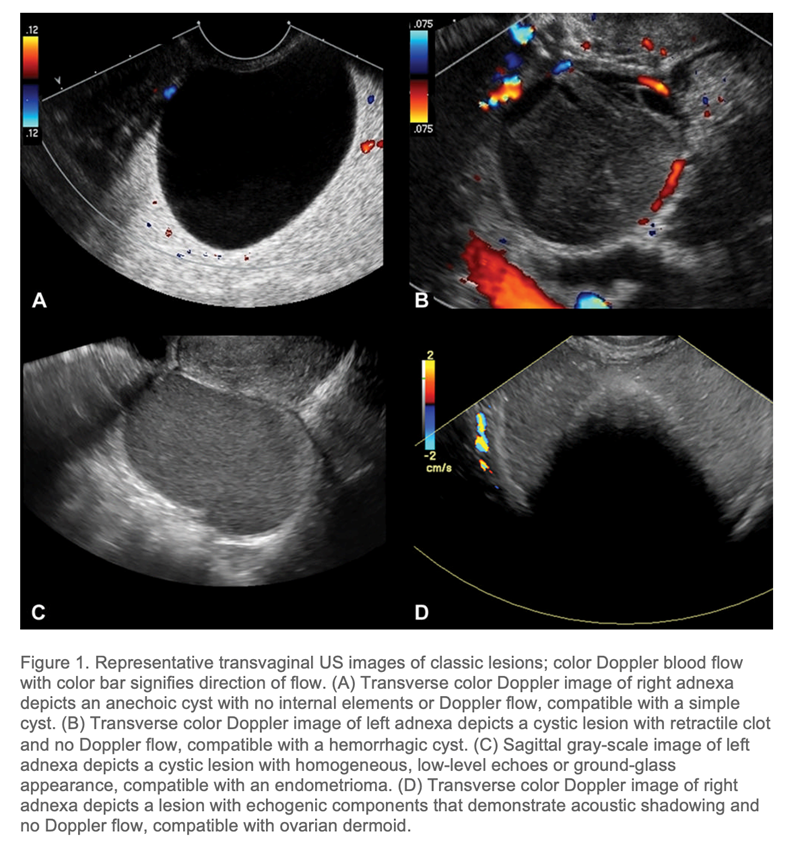
In the new study, Dr. Gupta and colleagues assessed a method that uses ultrasound images to classify adnexal lesions into one of two categories: classic or non-classic. Classic lesions are the commonly detected ones such as fluid-filled cysts that carry a very low risk of malignancy. Non-classic lesions include lesions with a solid component and blood flow detected on Doppler ultrasound. A classic versus non-classic approach to these lesions could help radiologists in a busy clinical practice more quickly assess a lesion.
The researchers looked at 970 isolated adnexal lesions in 878 women, mean age 42 years, at average risk of ovarian cancer, meaning they had no family history or genetic markers linked with the disease.
Of the 970 lesions, 53 (6%) were malignant. The classic versus non-classic ultrasound-based categorization approach achieved a sensitivity of 92.5% and a specificity of 73.1% for diagnosing malignancy in ovarian cancer.
The frequency of malignancy was less than 1% in lesions with classic ultrasound features. In contrast, lesions that had a solid component with blood flow had a malignancy frequency of 32% in the overall study group and 50% in study participants who were more than 60 years old.
“If you have something that follows the classic imaging patterns described for these lesions, then the risk of cancer is really low,” Dr. Gupta said. “If you have something that’s not classic in appearance, then the presence of solid components and particularly the presence of Doppler blood flow is really what drives the risk of malignancy.”
When a classic benign lesion is encountered, patients may be reassured a benign lesion is present, avoiding extensive further work-up. If additional research supports the study findings, then the system could end up being a useful tool for radiologists that would spare many women the costs, stress and complications of surgery.
“Ultimately, we’re hoping that by using the ultrasound features we can triage which patients need follow-up imaging with ultrasound or MRI and which patients should be referred to surgery,” Dr. Gupta said.
While these findings on diagnostic ultrasound exams offer valuable triaging information, ultrasound has not been proven beneficial specifically as a screening exam for ovarian cancer.
Related Articles
Citation
Ultrasound Predicts Ovarian Cancer. Appl Radiol.
March 22, 2022