Traumatic diaphragmatic hernia
Images
Prepared by Ephrain Coronado, MD, from the Department of Radiology, St. Cloud Hospital, St. Cloud, FL.
Case Summary
The patient is a 48-year-old white woman who developed acute onset of indigestion-type burning discomfort 1 hour after dinner, as well as chest, left shoulder, and left arm pain. This was associated with nausea, shortness of breath, and sweating. The patient could not stand the pain and was brought to the emergency room.
On physical examination, the patient's blood pressure was 137/60 mm Hg with a pulse of 108 bpm, and a respiratory rate of 25; she was afebrile. She was given nitroglycerin with no relief. Initially, promethazine hydrochloride 12.5 mg (Phenergan, Wyeth Pharmaceuticals, Madison, NJ) and meperidine hydrochloride 25 mg (Demerol, Sanofi-Synthelabo, Inc., New York, NY) were given with no significant relief. Then, she received ketorolac tromethamine 30 mg IV (Toradol, Syntex Laboratories, Palo Alto, CA) and, finally, morphine sulfate 3 mg IV (Astramorph, Astra Pharmaceuticals, Wayne, PA). These medications resulted in some improvement in her chest discomfort. She had no history of myocardial infarction or coronary disease.
Diagnosis
Traumatic diaphragmatic hernia
Imaging Findings
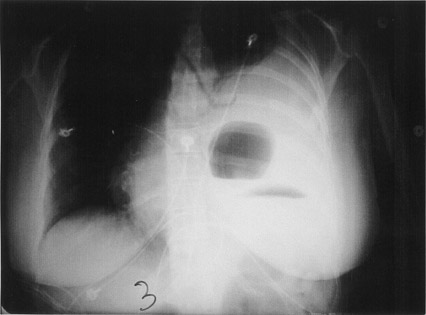
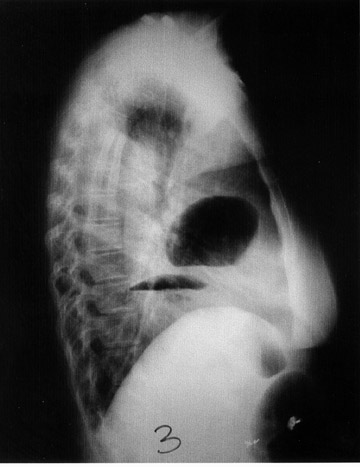
The initial posteroanterior and lateral views of the chest show a moderate left pleural effusion and an air-fluid level within the left lower chest (Figure 1).
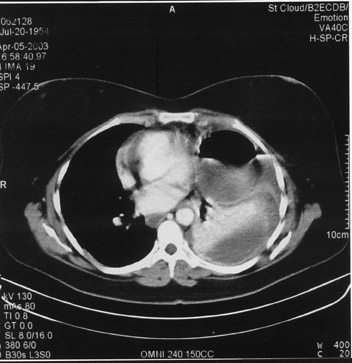
A second set of chest radiographs taken the following day once again showed a moderate left pleural effusion and a well-defined air-fluid cavity within the lower chest. A computed tomography (CT) of the chest revealed a moderate left pleural effusion, compression of the left lung, and a rounded air-fluid cavity anteriorly (Figure 2A). With all these findings, along with a clear history of previous trauma from a motor vehicle accident (MVA) 2 years previously, a presumptive diagnosis of traumatic diaphragmatic hernia was made.
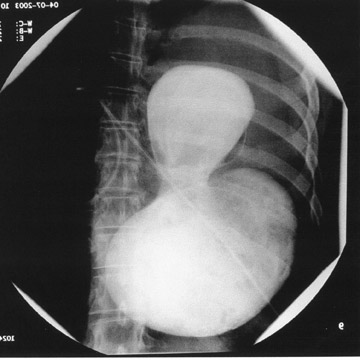
This diagnosis was confirmed with an upper gastrointestinal (GI) series, using a water-soluble contrast (Figure 2B). The study showed herniation of at least one-third of the stomach into the lower chest with moderate constriction at the orifice of the diaphragm.
Surgical Findings
The patient was taken to surgery and a diaphragmatic rupture was found centrally and very close to the pericardium. There was herniation of one-third of the stomach into the lower chest and a bloody pleural effusion. The stomach was reduced back into the peritoneal cavity and a partial gastrectomy was performed due to strangulation and necrosis along the greater curvature side. The diaphragmatic rupture was repaired.
Discussion
Traumatic disruption of the diaphragm can result from either penetrating (knife and bullet wounds), or blunt (MVA or falls), or crush injuries. The left hemidiaphragm is more often affected in cases of blunt trauma, especially within the posterior lateral aspect medial to the spleen. Although most traumatic hernias are seen immediately, some have a long latent period before symptoms are recognized. They can enlarge over time and have a risk of incarceration and strangulation. Herniation usually involves the stomach, but it can also involve the small and large bowel, omentum, spleen, liver, and gallbladder. The findings on plain chest radiographs are often suggestive of traumatic diaphragmatic herniation.
In such cases, imaging findings include: elevation of the hemidiaphragm, abrupt discontinuity, nonvisualization of the diaphragm (absent diaphragmatic sign), pleural effusion, atelectasis, and, at times, shift of the mediastinum away from the injured side. Gas bubbles and air-fluid levels above an irregular diaphragm are strong indications of injury. 1,2
Visualization of a hollow viscus above the hemidiaphragm with a focal constriction from compression of the bowel at the site of the tear in the diaphragm (known as the collar sign) is a diagnostic finding of visceral herniation by chest radiography.
The CT findings are discontinuity of the diaphragm (73% of patients); the collar sign (which is very specific [100%], but of limited sensitivity [36%]) 3 ; and intrathoracic herniation of solid abdominal viscera or omentum. In patients with chest radiography findings suggestive of diaphragmatic injury, scans are obtained through the lower chest to the inferior margin of the liver using a collimation of 5 mm and a table speed of 5 mm/sec (pitch = 1). Overlapping reconstructed images are obtained every 3 mm to perform sagital and coronal reformations. 4 Using this protocol, the overlapping reconstruction and volumetric acquisition capability of spiral CT results in higher quality coronal reformation images to evaluate the diaphragm. Magnetic resonance imaging has also been used to visualize the entire diaphragm. Tears can be visualized due to its ability to obtain coronal and sagital images with T1 spin-echo sequences.
Conclusion
Traumatic diaphragmatic hernia has always been a diagnostic challenge to both the radiologist and surgeon. More than 90% of blunt traumatic diaphragmatic ruptures result from motor vehicle accidents, as was the case in this patient. Multiple imaging modalities are available to evaluate the diaphragm following trauma. Chest radiographs are the initial and most commonly performed imaging study. Correlating a good clinical history with the imaging findings and a high index of suspicion will result in prompt diagnosis and treatment.
Related Articles
Citation
Traumatic diaphragmatic hernia. Appl Radiol.
May 6, 2004