Exophthalmos caused by an ethmoidal mucocele
Images

Prepared by Erini Makariou, MD and Nouredine Guaouguaou, MD, Department of Radiology, Georgetown University Hospital, Washington, DC.
Case Summary
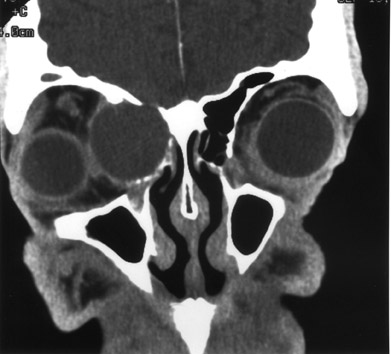
A 55-year-old man presented with chronic headaches. He had right orbital pain for several months and right exophthalmos. Otherwise, he did not have any significant medical history. Physical examination revealed right exophthalmos and a palpable mass in the right medial canthus, which prompted a computed tomography (CT) scan of the orbits/sinuses (Figures 1 and 2).
Diagnosis
Exophthalmos caused by an ethmoidal mucocele
Imaging Findings
The CT examination of the orbits/sinuses showed a well-defined ovoid mass that was homogenous in appearance, expanding and obliterating the right ethmoid cells. The lesion was predominantly hypo-dense and measured 3.5 × 2.7 × 2.7 cm. There was erosion of the medial wall of the right orbit and extension of the mass into the orbit with lateral displacement of the medial rectus muscle and optic nerve. The lesion caused exophthalmos (Figure 1). It extended superiorly through an erosion of the orbital roof into the frontal sinus, which was opacified. There was also erosion of the cribriform plate but no involvement of the brain parenchyma (Figure 2).
Discussion
A mucocele is an epithelial-lined, mucus-containing sac that is the most common cause of paranasal sinus expansion. Accumulation of mucoid secretions behind an obstructed paranasal sinus ostium is the primary etiology. This accumulation expands the sinus cavity and produces thinning or erosion and remodeling of the bony wall. The obstruction of the sinus cavity can be due to many causes, such as chronic sinusitis, nasal polyposis, neoplasia, postsurgical changes, or any other abnormality or trauma. They occur most frequently in the fronto-ethmoidal region. The frontal sinuses are involved approximately in 60% of cases, the ethmoidal complex in 30%, the maxillary in 10%, and the sphenoid sinuses are involved only rarely. 1 There is an increased incidence in patients with cystic fibrosis.
Mucoceles are usually observed during adulthood. In most cases, patients have a clinical history of chronic nasal polyposis or panasinusitis. The leading symptoms are unilateral proptosis with ophthalmalgia, double vision or decreased acuity, a palpable mass in the superior medial aspect of the orbit or medial canthus with the fronto-ethmoidal mucoceles, and headaches. 2
On plain X-ray films, a soft-tissue density mass may be seen obliterating the sinus with associated expansion of the involved sinus. Bony changes, such as erosion or thinning, may also be seen, especially with frontal mucoceles. These findings are better visualized on CT. Surrounding zone of bone thickening due to chronic infection is another manifestation. After intravenous contrast administration, there is uniform lack of enhancement with only a rim of enhancement from the infected mucosal membrane. Macroscopic evidence of calcifications may suggest superimposed fungal infection as seen in 5% of the cases. On magnetic resonance imaging (MRI), mucoceles are of low signal intensity on T1-weighted and of high signal intensity on T2weighted images. But a mixed type of signal may also be seen based on the presence of blood or inspissated secretions. Postgadolinium-enhanced MRI shows no enhancement of the mucocele. 3
Sinus cavity expansion differentiates mucoceles from uncomplicated chronic sinusitis (a finding never seen with sinusitis). It may be impossible to separate a long-standing mucocele producing bony erosions or remodeling from a sinus malignancy or aggressive infection, without the benefit of postcontrast images. A benign rim of enhancement is identified in the case of a mucocele and a nodular or solid enhancement in the case of malignancy.
Mucoceles may protrude into the orbits and cause vision problems and proptosis. Intracranial extension may produce optic nerve damage and blindness, involvement of the cavernous sinus with neurological symptoms, or hormonal changes in case of involvement of the sellar turcica/pituitary gland. Superimposed infections may also occur leading to pyoceles. 4
Surgical complete removal of the sinus mucocele lining is the traditional treatment. However, in recent years, there has been a trend toward transnasal endoscopic management because of its low morbidity rates and recurrence rates at or close to 0%. 5
Conclusion
Mucoceles are the most common benign lesions that produce expansion of the paranasal sinuses. Approximately 90% occur in the fronto-ethmoidal sinuses. Appropriate therapy of the mucocele may correct the associated complications, such as exophthalmos, and may prevent visual loss.
Related Articles
Citation
Exophthalmos caused by an ethmoidal mucocele. Appl Radiol.
May 6, 2004