Traumatic cervical spine distraction injury
Images


Case Summary
A 3-year-old boy presented as a Level 1 trauma patient after a high-speed, rollover motor vehicle accident in which he was an unrestrained passenger. He received cardiopulmonary resuscitation for 15 minutes in the field for pulseless electrical activity and was brought to our institution in critical condition.
Imaging Findings
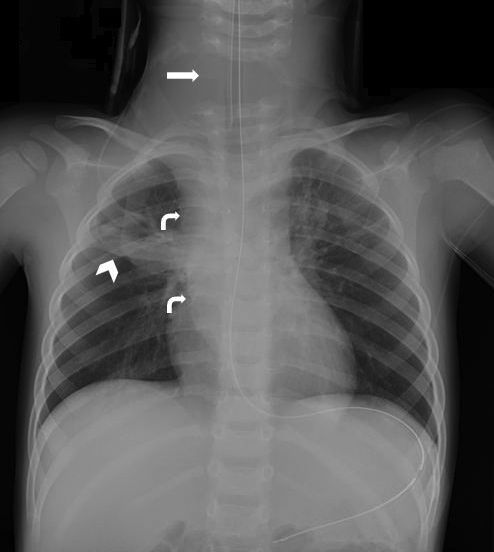
In the initial trauma workup, a portable AP radiograph of the chest revealed separation of the lower cervical vertebral bodies at the C6-C7 level, a widened mediastinum concerning for hematoma or CSF leak, and multifocal atelectasis (Figure 1).
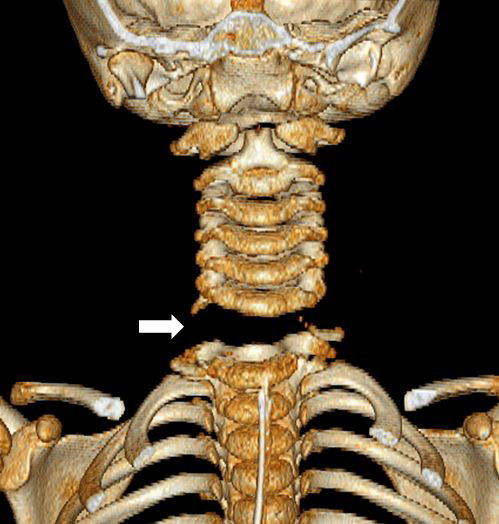
A coronal CT image demonstrated diffuse soft-tissue edema in the neck (Figure 2). A sagittal reformat (Figure 3) and 3D reconstruction in the coronal plane (Figure 4) revealed a C6-C7 distraction injury. Associated injuries not shown included complete transection fractures of the inferior endplates of C6 and the C6-C7 facets, diffuse cerebral edema and multiple facial fractures. Vascular injury was later excluded with CT angiography.
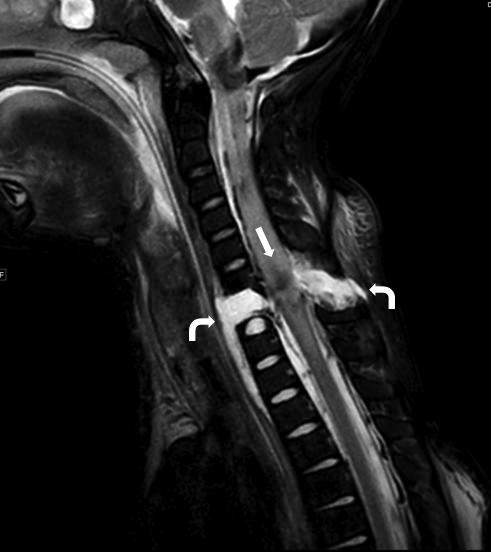
MRI of the neck was then performed to evaluate the cervical ligaments and spinal cord. A sagittal TSE T2 MR image of the neck showed severe cervical spine injury with a large area of edema secondary to the C6-C7 distraction (Figure 5). MRI of the brain showed multiple areas of cortical and central gray ischemic injury and intracranial hemorrhage consistent with severe traumatic brain injury (not shown).
Diagnosis
Traumatic cervical spine distraction injury at C6-C7.
The differential diagnoses for this injury include facet dislocation and pseudosubluxation.
Discussion
The pediatric cervical spine is very vulnerable to traumatic injuries. Cervical spine injuries account for 60-80% of all vertebral injuries in the pediatric population, with a mortality rate between 16 and 35%.1,2 Injury patterns include fracture, dislocation, distraction or a combination injury pattern. Children are more prone than adults to spinal cord injury without radiographic abnormality (SCIWORA).3 The most common mechanism of injury is motor vehicle accidents, with the majority of patients riding as unrestrained passengers.4
The level of cervical injury is often characteristic of the patient’s age. Younger children have disproportionately large heads and comparatively weak neck muscles; therefore. the fulcrum of cervical motion is at the C2-C3 level, which leads to upper cervical injuries. In adolescents, injuries are more common at the lower cervical levels because the fulcrum of cervical motion lies at C5–C6.5,6 Thus, the location of a C6-C7 distraction injury in a 3-year-old, as seen in our patient, is exceedingly rare.
Ligamentous and bony fractures of distraction injuries typically result in severe spinal cord injury, which can present as neurogenic shock. The classic triad of neurogenic shock includes hypotension, bradycardia and hypothermia. Due to the high-velocity mechanism, traumatic brain injury and associated fractures elsewhere in the body are common.7 Our patient suffered severe traumatic brain injury as well as neurogenic shock at presentation, requiring vasopressor support for several days after admission.
Imaging workup of traumatic cervical spine injury in the pediatric patient includes immediate radiographs with anteroposterior (AP), cross-table lateral, and open-mouth views. Care must be taken when positioning a baby on a backboard not to hyperflex the neck and further displace an unstable cervical spine. Malalignment of the spinous processes on the AP view is highly suspicious of a jumped facet and increased interspinous distance is suspicious of a posterior ligamentous injury. CT is used to further evaluate an abnormal radiographic finding to better delineate fractures, vascular injury, and associated injuries like hematoma. MRI is used to assess ligamentous injuries, the intervertebral discs and SCIWORA.3
Most pediatric cervical spine injuries can be managed nonoperatively with external immobilization; however, as surgical options for internal fixation improve, more surgeons are opting for early operative intervention when indicated. Indications for surgery include nonreducible deformities, unstable injuries requiring stabilization, progressive deformity, and decompression of neural structures.3
Conclusion
Cervical spine injuries are common in the pediatric population due to the unique biomechanics of the head and neck in children. Upper cervical injuries are more common in infants and young children while the lower cervical spine is more often injured in adolescents. The most common mechanism of injury is motor vehicle accidents, and the mortality rate of these injuries is not insignificant. A multi-imaging modality workup is often necessary to fully evaluate the extent of injury. Treatment is typically nonoperative, though there are indications for prompt surgical intervention.
References
- Cirak B, Ziegfeld S, Knight V, et al. Spinal injuries in children. J Pediatr Surg. 2004; 39:607-612.
- Silverman A, Amed N. (2009) Traumatic pediatric cervical spine craniocaudal distraction injury. Injury Extra. 2009; 40:4-5.
- Mccall T, Fassett D, Brockmeyer D. Cervical spine trauma in children: A review. Neurosurg Focus. 2006;20(2):E5 http://www.medscape.com/viewarticle/527718_7.
- Dogan S, Safavi-Abbasi S, Theodore N, et al. Pediatric subaxial cervical spine injuries: Origins, management, and outcome in 51 patients. Neurosurg Focus. 2006; February 2:1-7.
- Hill S, Miller C, Kosnik E, et al. Pediatric neck injuries. A clinical study. J Neurosurg. 1984; 60:700-706.
- Nitecki S, Moir CR. Predictive factors of the outcome of traumatic cervical spine fracture in children. J Pediatr Surg. 1994; November 29:1409-1411.
- Carreon L, Glassman S, Campbell M. Pediatric spine fractures: a review of 137 hospital admissions. J Spinal Disord Tech. 2004;17:477-482.
- Ghanem I, El Hage S, Rachkidi R, et al. Pediatric cervical spine instability. J Child Orthop. 2008;2:71-84.
Citation
K R, S J, A T.Traumatic cervical spine distraction injury. Appl Radiol. 2015; (5):26-28.
May 29, 2015