Spinal Giant Cell Tumor
Images

Case Summary
A child presented with a two-month history of worsening back pain. Two days prior to presentation the pain intensified. Patient has difficulty walking due to the pain.
Imaging Findings
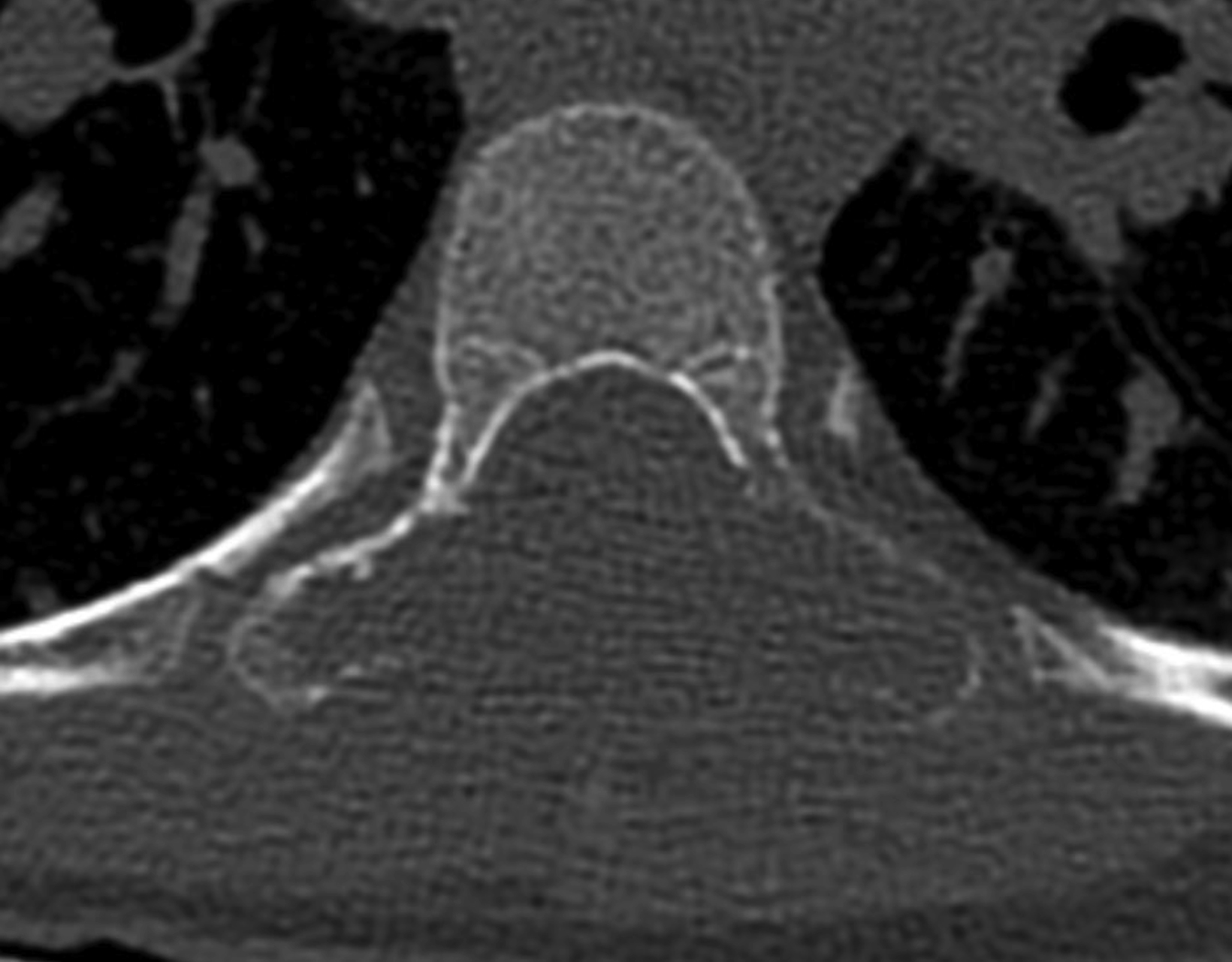
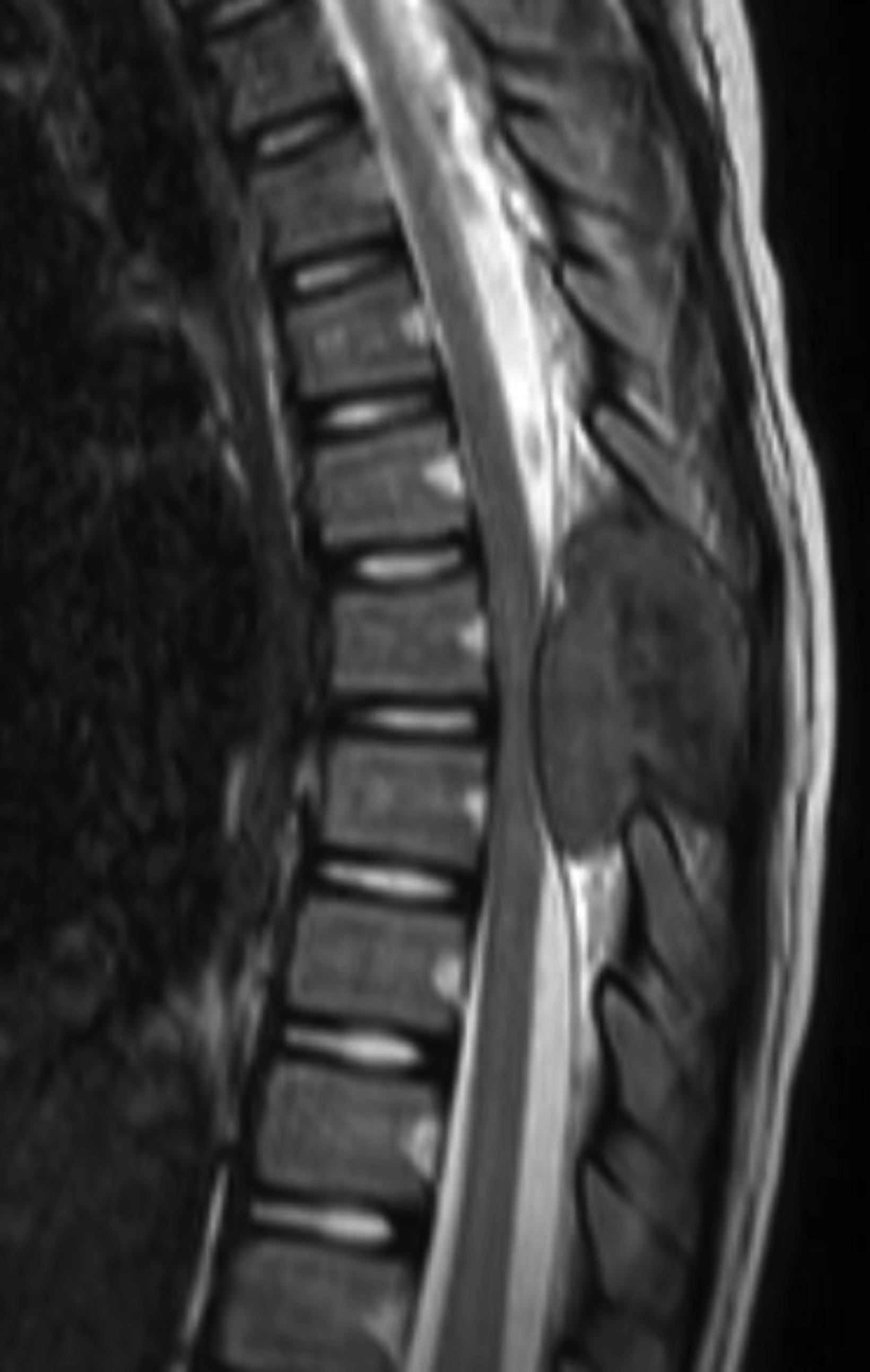
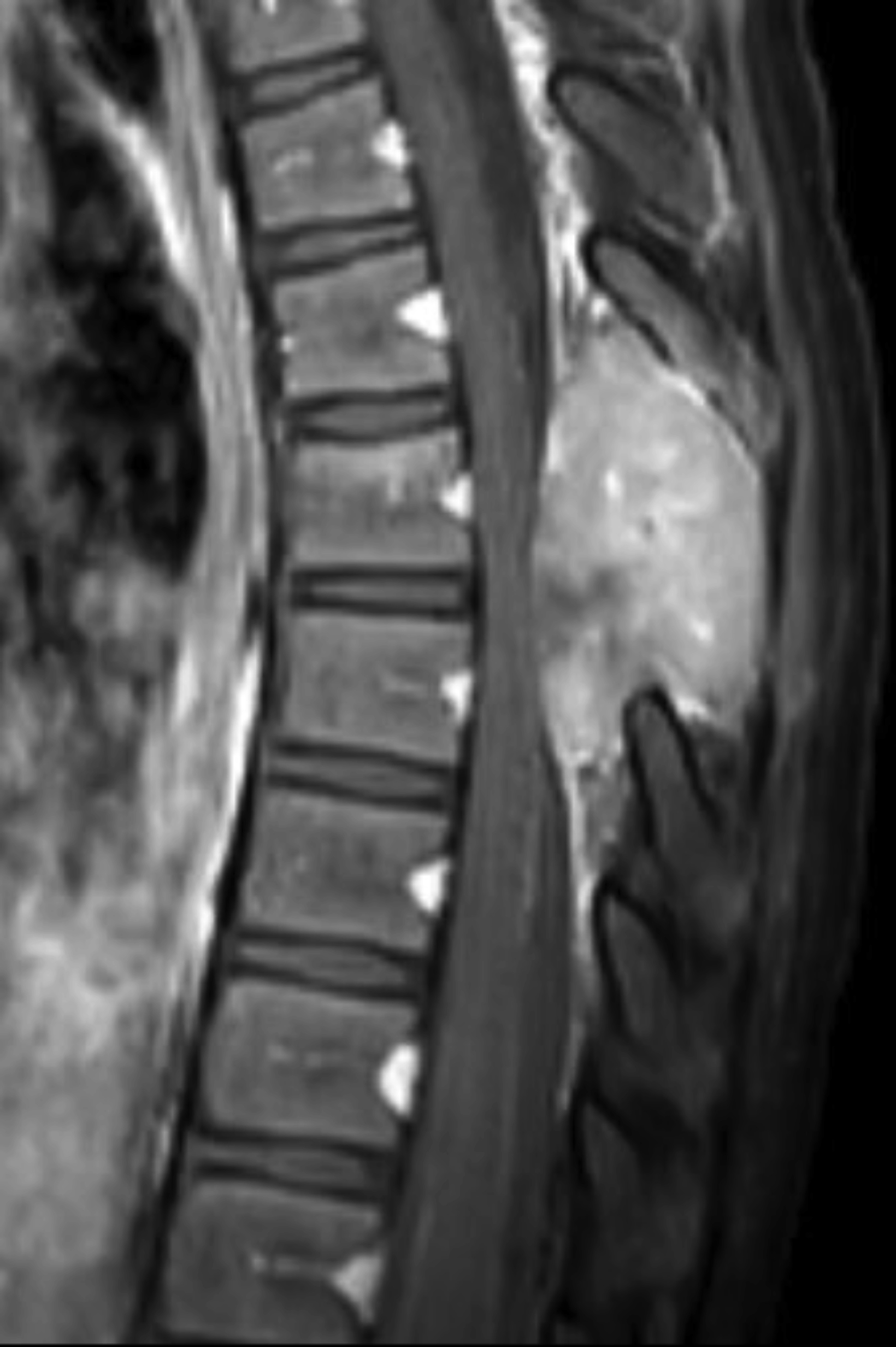
Sagittal and axial noncontrast computed tomography (CT) images of the thoracic spine showed a lytic and expansile lesion in the posterior elements of the T7 vertebral body. The lesion thinned the cortex with a cortical disruption noted (Figures 1,2). Sagittal mDixon T2 and sagittal T1 fat-saturated postcontrast images showed that the lesion was composed of soft tissue. The lesion caused posterior mass effect on the spinal cord with minimal signal change in the spinal cord. The lesion was predominantly T2 hyperintense (Figure 3) and T1 hypointense/isointense. There was heterogeneous contrast enhancement of the lesion following gadolinum-based contrast agent administration (Figure 4).
Diagnosis
Spinal giant cell tumor. Differential diagnosis includes metastasis and chordoma.
Discussion
Giant cell Tumor (GCT) is a well-studied primary tumor accounting for 5% of all primary bone tumors and 20% of benign skeletal tumors. Eighty percent of all GCTs occur in patients 20-50 years of age. 5.7% of GCT occur in patients that are under 19 years of age with 1.7% of GCT occurring in patients less than 15 years old.3 Most studies demonstrate an increased prevalence among females. GCT develops in various bones of the body. In the general population only 1.4% to 9.4% of GCT occur in the mobile spine (above the sacrum).1,2
In the setting of pain CT or MRI may be initially employed. However, there is value in ordering both studies as each can provide pertinent information. On CT, GCTs present as expansile, lytic lesions which demonstrate cortical thinning.6 CT helps to elucidate the cortical expansion and destructive changes. On MR imaging, GCTs demonstrate hypointense T1 signal with heterogeneous T2 hyperintense signal. Contrast enhancement patterns tend to be heterogeneous.5,7 In up to 14% of cases GCTs may also contain fluid-fluid levels due to secondary aneurysmal bone cyst (ABC) formation.7 This can lead to confusion and missed diagnosis of GCT, only reporting the ABC. Imaging characteristics on MRI are not pathognomonic but help to show the extent of the tumor and define the relationship of the tumor to relevant structures. Diagnosis should be made with tissue sampling, which would demonstrate multi-nucleated giant cells in a mononuclear stroma, consistent with GCT.4,5
Imaging follow up is also crucial. The overall local recurrence rate in the spine is 28% after surgical treatment.1 Recurrence can be difficult to detect. Immediate post-operative imaging can serve as a valuable baseline for comparison.
Conclusion
Spinal GTCs are uncommon tumors of the spine and even more uncommon in skeletally immature patients. Regardless, when a characteristic lytic and expansile lesion is identified in an immature spine, the diagnosis of GTC should be considered. Although diagnosis is made with tissue sampling, imaging is helpful in suggesting GCT and in directing treatment.
References
- Stefano B, et al. Giant Cell Tumor of the Mobile Spine: A Review of 49 Cases. Spine. 2012; 37(1):E37-E45. doi: 10.1097/BRS.0b013e3182233ccd.
- Chakarun CJ, Forrester DM, Gottsegen CJ, Patel DB, White EA, Matcuk GR. Giant Cell Tumor of Bone: Review, Mimics, and New Developments in Treatment. Radiographics. 2013; 33:1. https://doi.org/10.1148/rg.331125089
- Schütte, HE, Taconis, WK. Giant Cell Tumor in Children and Adolescents. Skeletal Radiol. 1993; 22: 173. https://doi.org/10.1007/BF00206148.
- Alfawareh MD, Shah ID, Orief TI, Halawani MM, Attia WI, Almusrea KN. Pediatric Upper Cervical Spine Giant Cell Tumor: Case Report. Global Spine Journal. 2015; 5(4):e28-e33. doi: 10.1055/s-0034-1396433.
- Jong Won Kwon, Hye Won Chung, Eun Yoon Cho, Sung Hwan Hong, Sang-Hee Choi, Young Cheol Yoon, and Sang Kyu Yi. MRI Findings of Giant Cell Tumors of the Spine. American Journal of Roentgenology. 2007; 189:1, 246-250. doi: 10.2214/AJR.06.1472.
- Gerber S, Ollivier L, Leclère, J, et al. Imaging of Sacral Tumors. Skeletal Radiol. 2008; 37: 277. https://doi.org/10.1007/s00256-007-0413-4.
- Anchan C. Giant cell tumor of bone with secondary aneurysmal bone cyst. Int J Shoulder Surg. 2008; 2(3):68. doi: 10.4103/0973-6042.42582.
References
Citation
RB KMMCJSTAT.Spinal Giant Cell Tumor. Supplement to Applied Radiology. 2022; (5):8-10.
September 2, 2022