SNMMI, Alzheimer’s Association Update Appropriate Use Criteria for Amyloid and Tau PET Imaging
Images
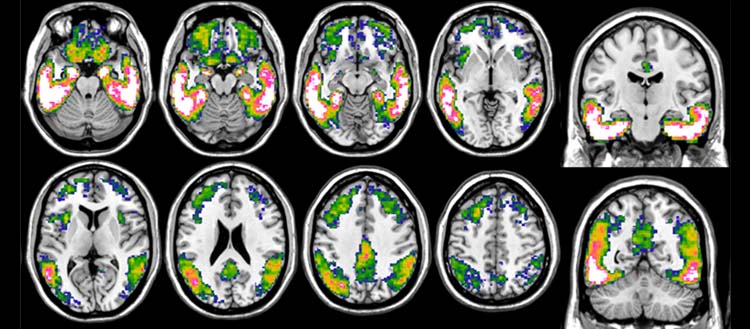
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the Alzheimer’s Association released updated appropriate use criteria (AUC) for amyloid and tau PET imaging in patients with Alzheimer disease, mild cognitive impairment and other dementias. The new criteria expand PET imaging guidance to include tau PET, incorporate updated information, and provide specific guidance to enhance diagnostic precision, treatment decisions and patient care.
This 2024 update is the first revision since the initial AUC for amyloid PET was introduced in 2013. Since then, the US Centers for Medicare and Medicaid Services (CMS) has announced key changes to reimbursement that make advanced imaging more accessible, lifting its one-scan-per-patient restriction in 2023 and unbundling payment for high-cost diagnostic radiopharmaceuticals in 2024. Notably, the updated AUC introduces guidelines for tau PET imaging, paving the way for its broader clinical use following the FDA’s approval of the tau radiotracer 18F-flortaucipir in 2020.
The updated criteria emphasize the critical role of PET imaging in identifying lesions associated with the diagnosis of Alzheimer disease and other tauopathies. The guidelines will help dementia experts determine whether imaging is appropriate, particularly when amyloid or tau imaging could significantly influence patient care and management.
“These new criteria focus on optimizing patient care,” said Kevin Donohoe, MD, chair of SNMMI’s Committee on Guidance Document Oversight. “They will help providers determine the most effective use of these important PET tracers as well as describe clinical scenarios that are not likely to benefit from PET imaging. The AUC also discuss the use of PET imaging for determining eligibility for newly introduced dementia treatments and for following treated patients for response to therapy. It is also expected these AUC will reduce the need for less specific diagnostic testing and provide guidance for safety considerations.”
In updating the AUC, a multidisciplinary task force reviewed an independent search of the clinical literature to address key questions about amyloid and tau PET imaging. They defined 17 clinical scenarios for which imaging would be either “appropriate”, “uncertain” or “rarely appropriate.” Factors including age, prognosis, how symptoms manifest, cerebrospinal fluid biomarker results, and whether a patient is considered at-risk were considered in the ratings. For amyloid PET, seven scenarios were deemed appropriate, two were deemed uncertain, and eight were determined to be rarely appropriate. For tau PET, the group rated five scenarios as appropriate, six as uncertain, and six as rarely appropriate.
While the AUC does not recommend that amyloid and tau imaging routinely be used together, it does highlight their distinct applications. Amyloid PET is more sensitive for identifying early Alzheimer pathology, especially in patients with mild cognitive decline or early-stages symptoms while brain accumulation of tau protein more closely follows the clinical progression of dementia.
“The field of dementia diagnosis and treatment is evolving rapidly, and this report incorporates the latest data and technological advances in recommending the best use of amyloid and tau PET. These imaging tests can also be compared to other emerging technologies, such as blood tests,” said Maria C. Carrillo, PhD, Alzheimer’s Association chief science officer and medical affairs lead and a co-author of the paper. “Neurologists and other clinicians rely on amyloid and tau PET, and it’s important they have the most up-to-date information on when they should be used.”