Radiomic Biomarkers from Pre-Treatment CT Scans May Improve Prognosis, Treatment for Head and Neck Cancers
Images
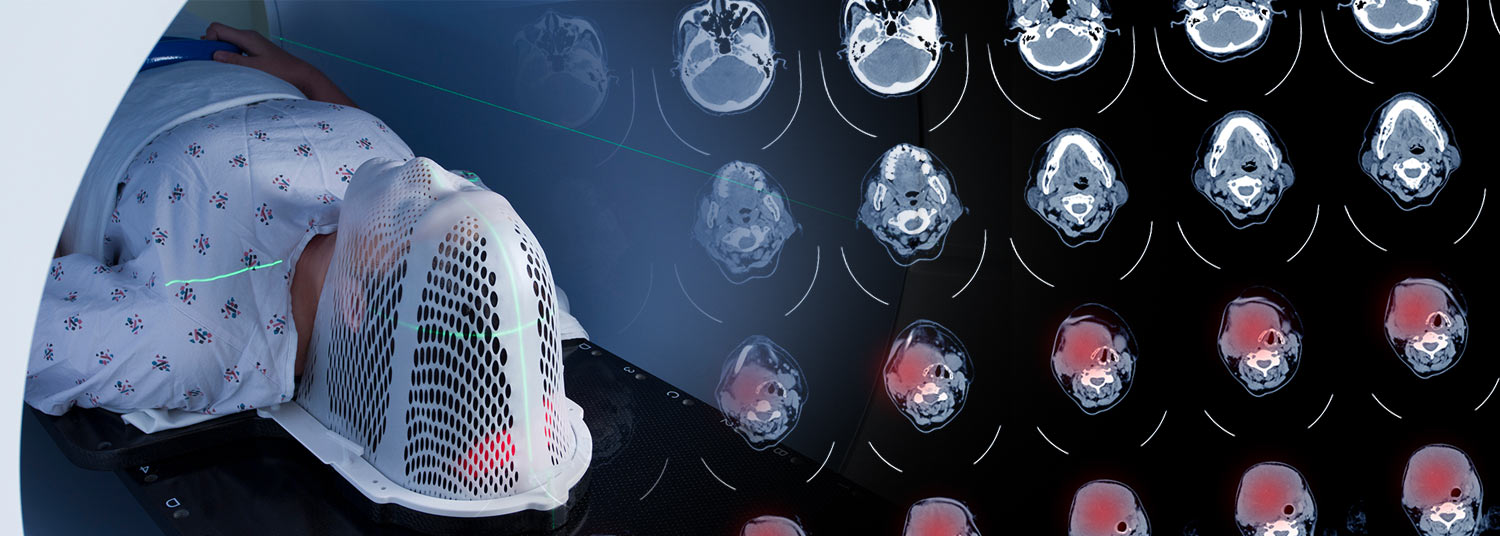
A new study provides insights that may eventually help oncologists better predict how cancers occurring in the mouth, nose, and throat will respond to certain therapies, leading to improved survival outcomes for patients. The findings, published in the journal Scientific Reports, analyzed the pre-treatment CT scans of patients with head and neck squamous cell carcinoma (HNSCC) to locate radiomic biomarkers that can be used to predict the aggressiveness of the disease and its response to treatment. The study was conducted by a team of researchers from the University of Maryland School of Medicine (UMSOM) Department of Radiation Oncology and the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC).
In this study, researchers took a closer look at the data collected by pre-treatment CT scans in 203 patients from UMGCCC and 77 patients from the MD Anderson Cancer Center dating back to 2003. Using radiomics, advanced mathematical and statistical algorithms, they identified tumor features that are not otherwise visible to the human eye. These biomarkers were then used to develop predictive models for treatment, focusing on the likelihood of progression-free survival after treatment. Researchers concluded that the identification of these radiomic biomarkers offer valuable insights into who will be most likely to benefit from certain treatments.
“Integrating prognostic and predictive biomarkers into clinical care could help to provide more targeted therapies, leading to improved survival outcomes for patients,” said the study’s senior author, Lei Ren, PhD, Professor of Radiation Oncology and Associate Chief of Physics Research in the Department of Radiation Oncology at UMSOM. “The findings from this study pave the way for future investigations through larger clinical trials to further evaluate the clinical efficacy of radiomics biomarkers for progression-free survival prediction in HNSCC patients.”
Despite advancements in surgical techniques and other therapies, the 5-year survival rate for HNSCC remains around 50 percent. Tobacco smoking and alcohol consumption significantly increase the risk of HNSCC, as well as certain strains of Human Papillomavirus (HPV).
Typical treatment for these cancers may include surgically removing the tumor, administering radiation to the affected area, or giving the patient a regimen of chemotherapy, immunotherapy, or a combination of therapies. These treatments can cause potentially permanent side effects impacting a patient’s ability to see, swallow, or speak. Researchers found that the use of radiomic biomarkers in treatment planning may also allow oncologists to recommend less invasive treatment protocols, therefore reducing the risk of lasting side effects.
“This research is reflective of our goal at UMGCCC to improve outcomes and reduce side effects for patients with HNSCC and other forms of cancer,” said William F Regine, MD, the Isadore and Fannie Schneider Foxman Professor and Chair of the University of Maryland Department of Radiation Oncology. “Exacting imaging biomarkers from standard-of-care CT scans offers a noninvasive approach without additional costs to patients.”
“Our Institute for Genome Sciences team played a crucial role in this study by helping to acquire the clinical data necessary for analysis, as well as evaluating and validating the obtained results,” said Daria Gaykalova, PhD, Associate Professor of Otorhinolaryngology at UMSOM and researcher at IGS. “We are proud to contribute to research in head and neck and other forms of cancer to learn more about causes and treatments.”
In future studies, researchers hope to gain a better understanding of these imaging biomarkers and their underlying meaning and validate their findings in data from other institutions. This research will need to be completed before a prospective clinical trial could be offered to patients for treatment intervention based on the imaging biomarkers and prognosis prediction. For example, patients with imaging biomarkers associated with less aggressive disease might be offered a decreased radiation protocol.
“While preliminary, this study offers a promising path forward to learn about novel predictors of response and to develop a non-invasive tool to personalize different treatment options for head and neck cancers,” said Taofeek K Owonikoko, MD, PhD, Executive Director of UMGCCC and the Marlene and Stewart Greenebaum Distinguished Professor of Oncology at UMSOM.