Radiology of body packers: The detection of internally concealed illegal materials
Images



Dr. Prabhu and Dr. Patel are Radiologists, Radiology Department, Newark Beth Israel Medical Center, Newark, NJ. Mr. Ne'eman is a student, University of Maryland, Baltimore, MD. Mr. Bier is a student, East Brunswick High School, East Brunswick, NJ.
The practice of body packing is defined as the trafficking of illicit drugs within the gastrointestinal tract or vagina.1 Body packers, also known as "swallowers," "internal carriers," "couriers," or "mules," were first reported in Toronto in 1973.2 Currently, customs officials seize >1 million pounds of drugs annually, with marijuana, cocaine, and heroin representing the majority of the illegal narcotics.3 As 80% of apprehended drug smugglers use the practice of body packing, it is imperative for radiologists to understand and familiarize themselves with the radiological signs of ingested drug packets.4 Radiologists must also be aware of their legal responsibilities when interpreting examinations of suspected smugglers.
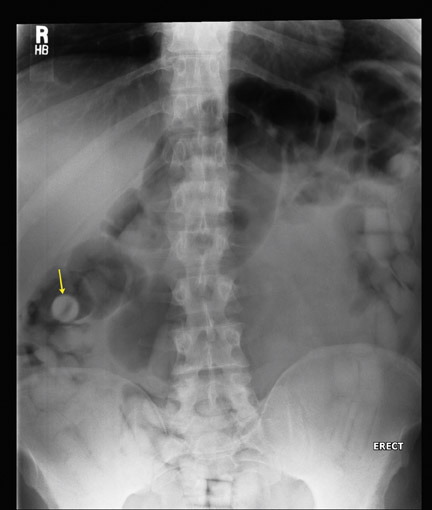
Body packers ingest drug packets, commonly consisting of a latex sheath, such as a condom or balloon, filled with tightly packed illicit drugs. Law enforcement officials often call upon radiologists to document drugs within the gastrointestinal tract of suspected drug traffickers. Radiological measures may also be required also when suspected smugglers present with foreign-body-induced in test inal obstruction or drug toxicity due to the rupture or leakage of drug packets. The most commonly used radiological method for investigating suspected body packers is the abdominal radiograph. This is a relatively quick study that is easily performed and has a high accuracy for the detection of drug-filled packets. Ingested drug packets appear unusually uniform in shape and are often spherical or cylindrical. However, as stool may also appear somewhat spherical as well, the radiological differences between ingested drug packets and surrounding stool may be subtle.5,6 The high density of material within the packets and the dense edge of the packet's synthetic material helps distinguish the ingested substance from normal bowel content. Often, the most useful finding is a thin, lucent rim of air in a spherical or cylindrical pattern. This finding is most often caused by air trapped between the wrapping and the illicit substance (Figure 1). This distinctive finding can also be created by a rim of air found between layers of latex when body packers use double-wrapped condoms, the so-called double condom sign.7,8
Plain abdominal radiography has been credited with a sensitivity of 85% to 90%. However, after reviewing the literature and interviewing law enforcement officials, we caution the reader that such a high sensitivity may be inappropriately optimistic since a "negative" radiograph often leads to a suspect's release. Body CT performed without oral contrast has been shown to achieve the high degree of sensitivity desired; however, due to current legal restraints, these studies are less likely to be performed than radiographs.5
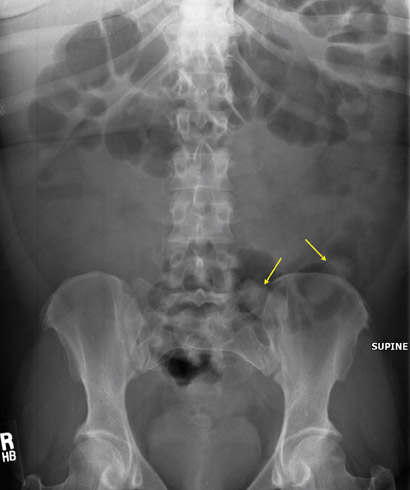
A falsely negative radiograph can lead to intestinal obstruction and/or drug toxicity in a subject and can allow the successful introduction of illicit drugs into a community.6 A review of the literature reveals that the major cause of documented false-negative results has changed during the past 3 decades. Rather than resulting from the inexperience of radiologists, as was the case in the 1970s and 1980s, today the primary source of false-negative results are sophisticated smuggling techniques that attempt to limit detection by decreasing the radiodensity difference between drug packets and stool. Clever packaging techniques-such as the incorporation of aluminum foil, plastic food wrap, and carbon paper-are now used to alter the radiodensity of ingested drug packets.9,10 Packaging a narcotic loosely within its wrapping material further decreases the likelihood of detection by lowering the radiodensity of the in gested contraband (Figure 2). Machine-made wax packets remove the rim of air that radiologists are accustomed to visualizing. Jamaican radiologists report the use of less radiodense packaging material such as pig in testines.11 Smugglers may also attempt to mask drug packets within surrounding stool by inducing constipation with diphenoxylate or loperamide.12,13 Radiologists should be cautious in cases of young, otherwise healthy suspected drug smugglers when abdominal radio graphs show only constipation.
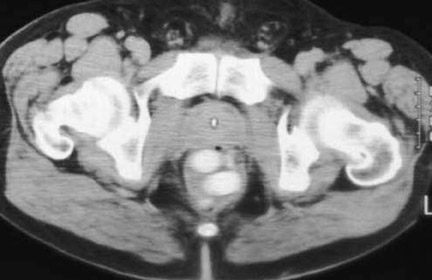
An understanding of the radiographic properties of common illicit drugs will help the radiologist overcome these surreptitious criminal techniques. A popular misconception of radiologists and emergency room physicians is that the high-density material seen on radio graphs is the illicit drug. This is true in the case of hashish or cocaine stones; however, several in vitro studies in Europe have shown that pure, unadulterated heroin and cocaine powder as well as Ecstasy (3,4-methylenedioxy meth am phetamine), and Thai pills (mixtures of methamphetamine and caffeine) display variable radiographic densities1 (Figure 3). CT attenuation values of commonly smuggled drugs can range from 700 HU to the density of fat or air (Figure 4). Research performed by Austrian radiologists in collaboration with the Austrian Customs Police reveal that the high radiographic density of drug packets is most dependent on the chemicals used as cutting agents and also on how tightly the drugs are packed.8,9 Therefore, with illicit drugs showing such variable radiodensities, the most reliable radiographic findings in the detection of body packers remains geometrically shaped densities surrounded by thin rims of air and arranged in a nonrandom pattern, particularly with a background of constipation.
Oval, elongated foreign bodies (such as carrots, asparagus, bladder stones, and intra-abdominal calcifications) have on occasion been misinterpreted as drug packets.5,14 The most common cause of falsely diagnosed ingested drug packets in suspected smugglers is hard stools, particularly when the patient showed radiographic signs of constipation (Figure 5).5,9 While false-positive diagnoses are not common, radiologists must be careful not to let the intimidating label of "drug smuggler" influence their interpretation. The difference between stool within a gas-filled gastro intestinal tract and ingested drug packets can be subtle. A helpful sign for radiologists is that drug couriers tend to ingest large numbers of packets. A 2005 study found the mean number of carried packets was 70.0 ± 20.4, with a range of 18 to 150. Single or small numbers of air-rimmed oblong shadows tend to be stool, not drug packets.15
Since radiologists have a significant role in whether a suspected body packer is charged with a crime and radiographic interpretations can influence the verdict of guilt or innocence, radiologists should familiarize themselves with their responsibilities toward both the state and the patient. When law enforcement agents bring a suspect to a hospital, treating physicians do not become an agent of the state. However, when radio graphic means are used to determine if a patient is charged with a crime, the interpreting radiologist becomes a participant in the process of law enforcement.9,16 Radiologists are unlikely to be held responsible for procedural violations committed by law enforcement agents; however, radiologists should be aware of the methods used to determine if a suspect warrants evaluation by hospital personnel and of the basic underlying legal principles and the ethical issues that arise from such detainments.
While radiologists need not be experts in the specifics for determining a suspect's detention, they should be aware that the main cause for detainment is the U.S. Customs/Department of Homeland Security's Courier Profile. Government agents use a profile, which is based upon multiple law enforcement criteria, to determine if a person's actions are suspicious enough to warrant detainment and arrest.17 Detention based on profiling may place the radiologist in the ethically confusing position of performing medical tests on asymptomatic patients who are deemed suspicious because of characteristics that may be displayed by innocent persons (eg, nervousness, arrival from a source city, little or no luggage, cash purchase of ticket). Ethical questions also arise as the decision to perform tests is made by nonmedical personnel who base their decisions on a profiling system that has never been empirically validated.17 Questions have also been raised concerning whether asking or demanding a suspect to undergo radiographic testing violates a patient's Fifth Amendment right against self-incrimination.
There are other medicolegal dilemmas. The radiological procedures, in particular CT with oral contrast, carry slight health risks. Contrarily, without proper detection and removal of internally concealed drugs, body packers may experience drug toxicity or intestinal obstruction from concealed packets. Ignorance or fear of radiological examinations may lead an innocent detainee to be falsely imprisoned. The situation is further muddled as the clinical outcome of body packers is considered to be unpredictable and some of the treatments (such as surgery, enemas, and food deprivation) carry potentially serious complications.18
A body packer who is not yet in legal custody poses even more of a medico legal dilemma. Should law-enforcement officials be contacted if a patient presents to the emergency room with symptoms of drug-packet ingestion? Most hospitals in America and Europe follow a policy of confiscating and destroying drugs without notification of law enforcement officials when the drug is discovered on a symptomatic patient who presents for treatment and is not under criminal investigation. This policy is based upon the belief that doctor-patient confidentiality should not be overridden solely because of illicit drugs.5,16,18 A review of both the international medical and American legal literature finds no absolute answer to these dilemmas. Notification of hospital-based legal counsel and of a hospital ethics committee is perhaps the most prudent course.5,19
REFERENCES
- Hergen K, Kofler K. Drug smuggling by body packing: What radiologists should know about it. Eur Radiol.2004;14:736-742.
- Deitel M, Syed AK. Intestinal obstruction by an unusual foreign body. Can Med Assoc J. 1973;109: 211-212.
- U.S. Customs and Border Patrol. CBP border patrol seizes over 1.1 million pounds of narcotics through the third quarter of fiscal year. Available at: http://www.cbp.gov/xp/cgov/newsroom/news_releases/archives/2006_news_releases/062006/06302006.xml. Accessed June 9, 2007.
- Lutz FU, Reuhl J. Body packing as a fatal risk: Result of a questionnaire survey in Western Europe. Beitr Gerichtl Med.1992;50:211-214.
- Traub SJ, Hoffman RS, Nelson LS. Body packing-the internal concealment of illicit drugs. N Engl J Med.2003;349:2519-2526.
- Ichikawa K, Tajima N, Tajima H, et al. Diagnostic imaging of "body packers" [in Japanese]. Nippon Iqaka Hoshasen Gakkai Zasshi.1997;57:89-93.
- Hierholzer J, Cordes M, Tantow H, et al. Drug smuggling by ingested cocaine-filled packages: Conventional x-ray and ultrasound. Abdom Imaging.1995;20:333-338.
- Pinsky MF, Ducas J, Ruggere MD. Narcotic smuggling: The double condom sign. J Can Assoc Radiol. 1978;29:79-81.
- Karhunen PJ, Suoranta H, Penttilä A, Pitkäranta P. Pitfalls in the diagnosis of drug smuggler's abdomen. J Forensic Sci. 1991;36:397-402. Comment in: J Forensic Sci. 1992;37:681-682.
- Aldrighetti L, Paganelli M, Giacomelli M, et al. Conservative management of cocaine-packet ingestion: Experience in Milan, the main Italian smuggling center of South American cocaine. Panminerva Med. 1996;38:111-116.
- McCartney T. 29th Annual Dr. Ena Thomas Memorial Symposium. Reported in: KPH burdened by drug mules. Jamaica Gleamer. November 20, 2002.
- McCarron MM, Wood JD. The cocaine "body-packer" syndrome. Diagnosis and treatment. JAMA.1983;250:1417-1420.
- Khan FY. The cocaine "body-packer" syndrome: Diagnosis and treatment. Indian J Med Sci.2005; 59:457-458.
- Raben AM, Phoa SS, Busch OR, Schultz MJ. Case report of a smuggler's dinner: Carrots and asparagus, or bolitas? Med Sci Monit.2005;11: CS79-CS81.
- de Prost N, Lefebvre A, Questel F, et al. Prognosis of cocaine body-packers. Intensive Care Med.2005;31:955-958.
- Wittau M, Weber D, Reher B, et al. Emergent surgery for body packing-what happens to the drugs? [in German]. Chiurug. 2004;75:436-441.
- Cloud M. Search and seizures by the numbers: The drug courier profile and judicial review of investigative formulas. Boston Univer Law Rev.1985;65: 853-921.
- Pidoto R, Agliata A, Bertolini R, et al. A new method of packaging cocaine for international traffic and implications for the management of cocaine body packers. J Emerg Med. 2002;23:149-153.
- Rella J. Drug smuggling raises medical and legal issues. Cleve Clin J Med.2002;69:465-466. Comment on: Cleve Clin J Med.2002;69:453-462.
Author's note
The authors of this article include Ari Ne'eman, a college sophomore with autism, and Kenneth Bier, a high school junior with an autoimmune neurological disorder. Project Head-On, a nonprofit organization dedicated to empowering the lives of people on the autism spectrum, selects students to be mentored by local radiologists. With their eagerness and imagination, the students, at times, mentored the radiologists. For more information, email: drsjb123@aol.com.
Ramdas Prabhu, MD