Pulmonary Veno-Occlusive Disease and the Role of the Radiologist
Images




Pulmonary veno-occlusive disease (PVOD) is an uncommon form of pulmonary hypertension (PH) with preferential involvement of the pulmonary venous system rather than the pulmonary arteries seen in other causes of pulmonary hypertension.1 The condition was initially described by German physician J Hora in 1934; however, not until 1966 was the term PVOD established as a separate entity by Heath, et al.2 In 2015, the Joint Task Force of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) identified PVOD as a distinct disease, categorizing it as subgroup 1 of pulmonary arterial hypertension (PAH) in the clinical classification of pulmonary hypertension (Table 1). 3
Despite the compartmental histological difference, patients with PVOD share clinical characteristics similar to those of patients with PAH due to other causes. However, the distinction of PVOD from other entities of PH is paramount, as patients with PVOD have a worse prognosis.
The gold standard for diagnosis of PVOD is lung biopsy, but this procedure carries a high risk of morbidity/mortality for patients with reduced respiratory reserve.4–6 A consensus for a minimally invasive diagnostic approach has been established which includes diagnostic radiology, pulmonary catherization, echocardiogram, bronchoalveolar lavage, medical therapy, and genetic testing.
This review addresses the various aspects of PVOD, including its clinical presentation, etiology, risk factors, and treatment, and discusses the important role of the radiologist in recognizing key imaging features that can aid in diagnosing the condition.
Clinical Presentation
The clinical presentation of patients with PVOD is nonspecific and difficult to distinguish from PAH and sequelae of cardiovascular disease. Typical symptoms include progressive dyspnea, reduced exercise tolerance, syncope, and hemoptysis.1,4,6– 8 Cardiac auscultation may show a prominent P2 component of the second heart sound and systolic murmur of tricuspid regurgitation.4 An additional clinical sign is digital clubbing, which is more frequently seen in PVOD than in idiopathic pulmonary arterial hypertension (IPAH).9 Nonspecific clinical signs include elevation of the jugular venous pressure, peripheral edema, ascites, and hepatomegaly.
Epidemiology, Etiology, and Risk Factors
The incidence of PVOD ranges from 0.1 to 0.5 cases per million.3,10 This estimate is likely low, as 5-10% of cases are either misclassified as IPAH1,5 or unrecognized, as PVOD can occur in association with other diseases, including HIV,12–14 bone marrow transplant, malignancies, and connective tissue diseases.15–21,22,25 Males are usually affected more than females.1,4 The distribution of age at diagnosis is bimodal, with the youngest ranging from 20 to 30 years, reflecting genetic causes, while the second peak is observed at 70 to 80 years, which can be attributed to secondary causes.1
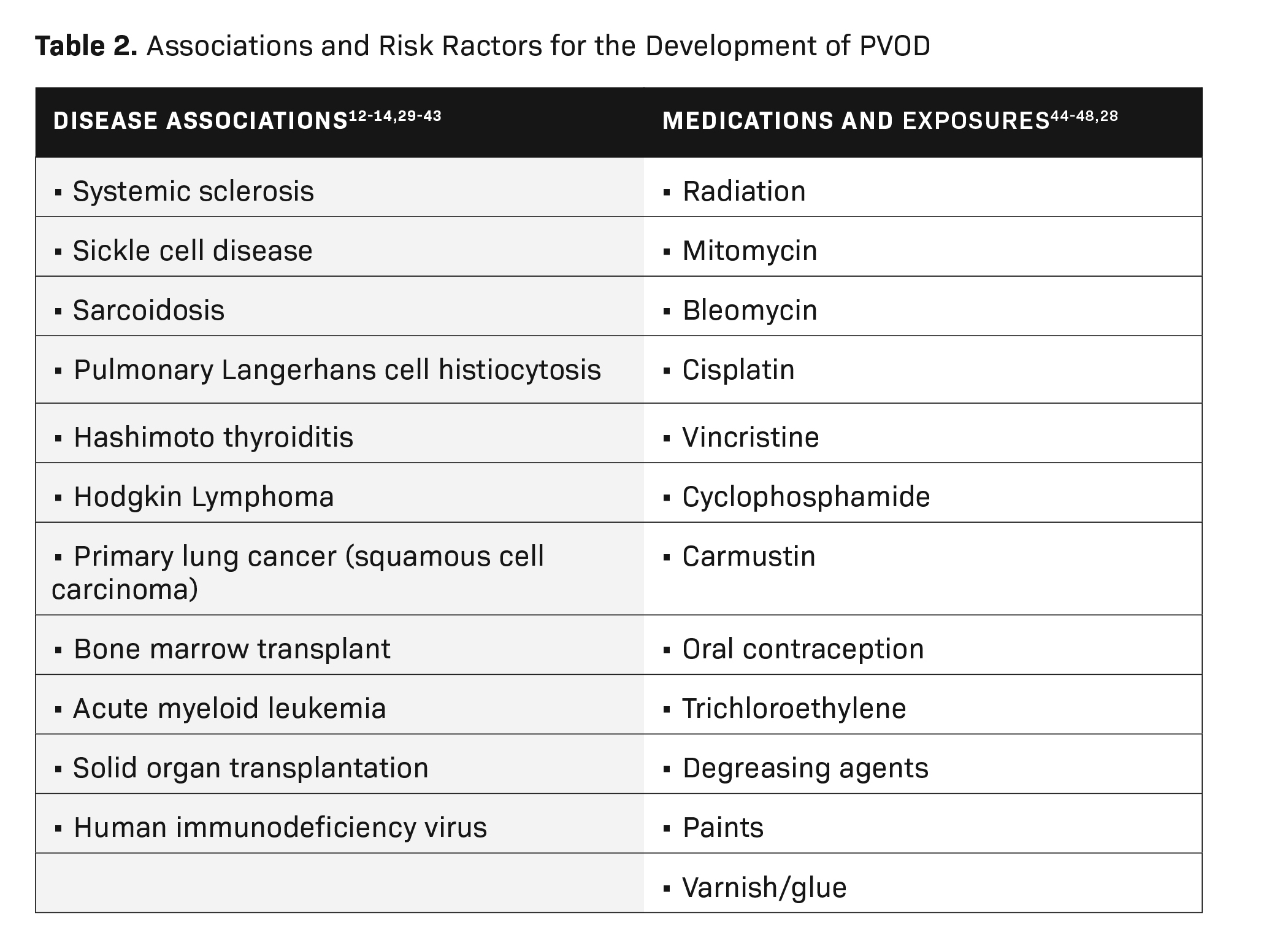
Apart from the mutation in eukaryotic translation initiation factor 2 alpha kinase 4 (EIF2AK4), which has been confirmed as a cause PVOD,26,27 several disease processes and exposures are related to PVOD development. These include inflammatory/immunological, connective tissue diseases, malignancy, medication-related effects, and occupational exposures (Table 2).
A case control study revealed exposure to trichloroethylene was significantly more frequent in PVOD compared to idiopathic PAH (42% vs 3%, respectively).28 The use of trichloroethylene was reported mostly by metal workers, mechanics, building painters, and cleaners. Other chemical exposures included degreasing agents, paint, and varnish/glue.
The prognosis is bleak for patients with PVOD, with an estimated mortality of 72% at one year from time of diagnosis and close to 100% within two years without definitive treatment as reported in two case series.1,4,49
Histopathology and Pathogenesis
All three vascular compartments of the pulmonary vasculature (pulmonary veins, capillaries and arteries) are affected in PVOD, with a predilection for the pulmonary veins.50, 51 Inflammation and immune-mediated injury of pulmonary venules are implicated in PVOD pathogenesis, with the disproportionate upregulation of circulating cytotoxic T-cell, natural killer cell, and natural killer T-cell populations.52
The autosomal recessive bi-allelic mutations of EIF2AK4 have been confirmed in all patients with the heritable form of PVOD and in approximately 9% of sporadic cases.53,54 EIF2AK4 belongs to a family of four kinases that are involved in controlling general translation in response to various cellular stresses. EIF2AK4 function loss leads to increased inflammation and oxidative stress.55
Histologically, diffuse remodeling of post-capillary venules and septal veins results in smooth muscle hyperplasia and intimal fibrosis leading to luminal narrowing. In turn, the affected vessels are obliterated as a result of thrombosis.32,50-52,56 In addition, focal proliferation of capillaries within the alveolar septa is associated with mild interstitial inflammatory infiltrates known as capillary hemangiomatosis-like foci,57 interstitial edema, and/or mild fibrosis of the interlobular septa.2 Pulmonary venous obstruction and pulmonary haemorrhage results in hemosiderin deposition from macrophages. PVOD arterial lesions are similar to PAH; they include intimal fibrosis, medial hypertrophy, and thrombotic occlusion. Plexiform lesions typical of PAH, however, are not present.32,49 Lymphadenopathy secondary to lymphatic vessel congestion occurs frequently in PVOD, leading to nodal congestion with dilatation of the sinuses.58
Imaging Diagnosis
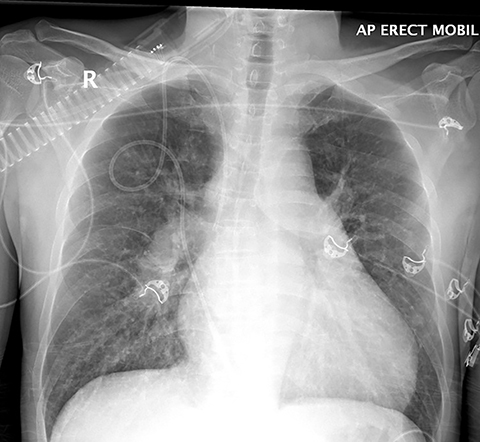
Chest radiography is included in the diagnostic work-up, but the modality has limited sensitivity for PVOD.9, 59 In severe pulmonary hypertension, chest radiographs show enlarged main pulmonary arteries and right-ventricular hypertrophy, the detection of which can be aided by a lateral radiograph demonstrating right-ventricular enlargement with encroachment of the right ventricular silhouette into the retrosternal space (Figure 1). Other features include prominent upper-lobe pulmonary vasculature and attenuation of pulmonary vascular markings. Nonspecific findings include Kerley B lines, pulmonary edema, and pleural effusions.6
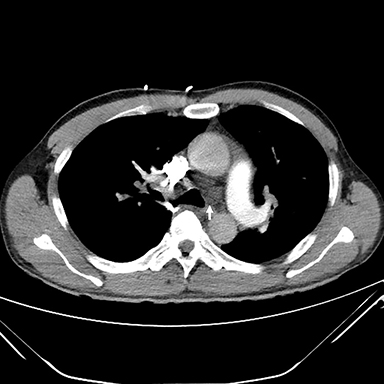
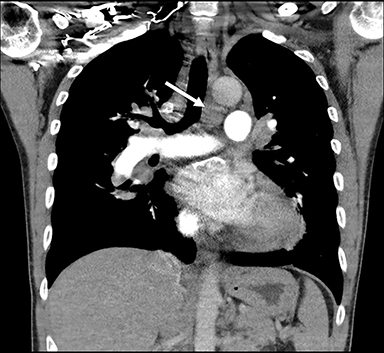
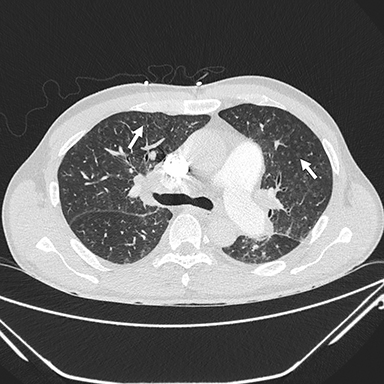
Thin-section CT, a relatively specific test, plays an important role in the minimally invasive approach to PVOD diagnosis. Interlobular septal thickening and centrilobular ground glass opacities have been shown in several studies to be statistically significant features. The presence of thickened interlobular septa has a sensitivity and specificity of 83% and 87%, respectively, in patients with suspected PVOD.1, 62, 63, 66 Lymphadenopathy is also a common feature (Figures 2, 3).61-64 In the setting of precapillary PAH of unknown etiology, the presence of at least two of three CT signs—septal thickening, centrilobular ground glass opacity, and lymphadenopathy—has a sensitivity of 95.5 % and a specificity of 89 %, with a positive predictive value of 72.5%. A high negative predictive value of 98.5% confers exclusion of PVOD.61
In a small number of biopsies, Resten, et al, found that a centrilobular pattern of distribution of ground glass opacities was significantly more frequent than a panlobular pattern in PVOD, with a sensitivity and specificity of 87% and 67%, respectively.62 The pathogenesis of centrilobular ground glass opacities is not well known; however, their presence may be caused by formation of cholesterol granulomas resulting from occult pulmonary hemorrhage.67 Pleural and pericardial effusion are frequent in PVOD, but they are not specific for pre-capillary PAH.62
Thin-section CT can reveal a mosaic pattern with oligemic areas of hypoattenuation, suggesting vascular rather than small airway disease.65
Diagnostic Criteria
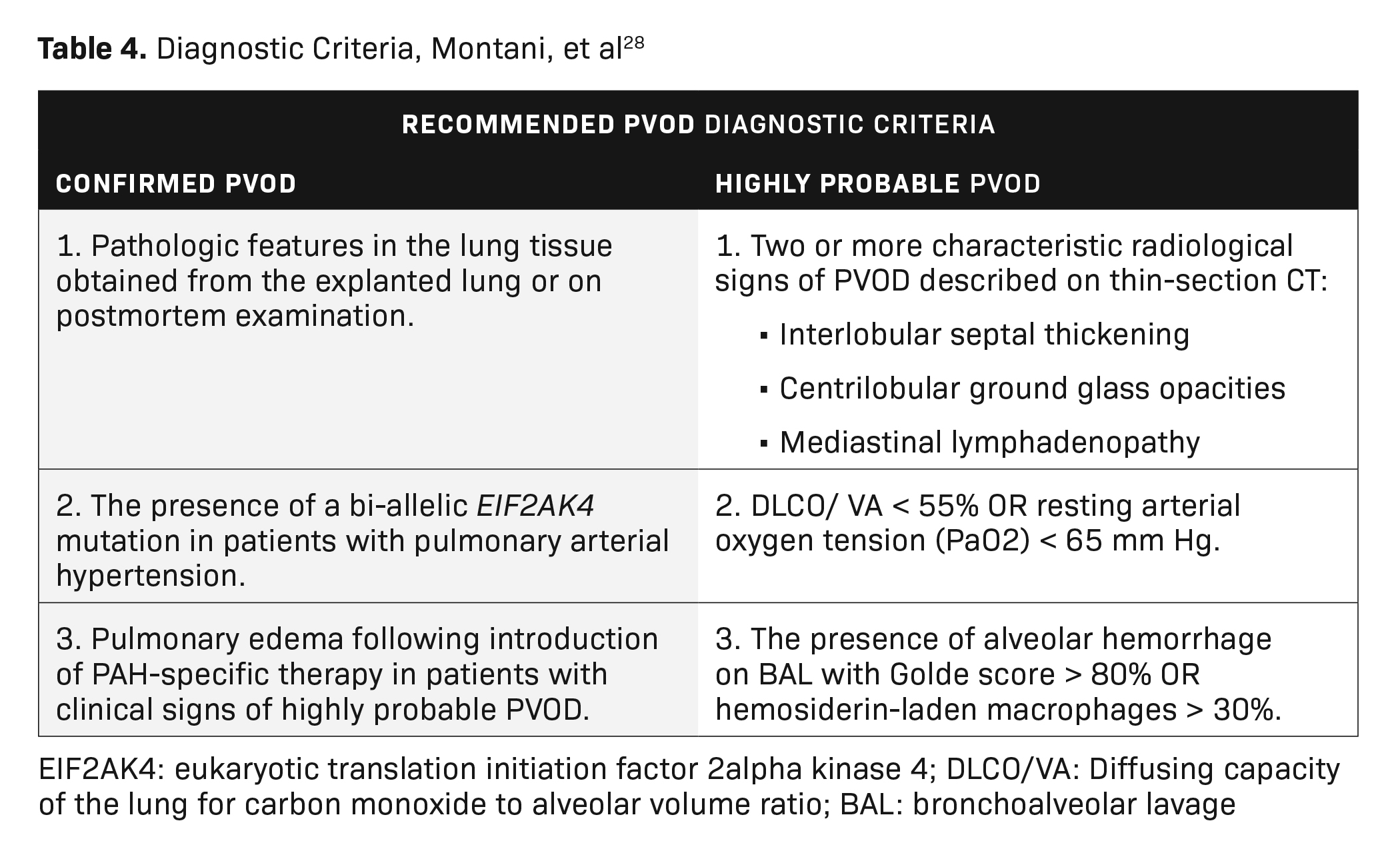
Definitively diagnosing PVOD requires histopathological confirmation via tissue biopsy. This is an invasive procedure, however, that greatly affects patient morbidity and can lead to premature death. A combination of minimally invasive tests has been explored to diagnose PVOD clinically (Table 3). Moreover, Montani, et al, have proposed a PVOD diagnostic algorithm termed “recommended” and “highly probable” PVOD diagnostic criteria (Table 4).28
Differential Diagnosis
Pulmonary Capillary Hemangiomatosis (PCH)
The European Respiratory Society/European Society of Cardiology (ERS/ESC) Classification of Pulmonary Hypertension has grouped PVOD and PCH in a special subgroup of Group 1 of PAH.3 In the past, PVOD and PCH were regarded as separate conditions. However, current evidence based on histology regards PVOD and PCH as varied expressions of the same disorder,49 while some regard PCH as a secondary process of PVOD occurring in smaller veins.
In addition, there is histological overlap between PVOD and cases of PCH in which they are characterized by aggressive, patch-like capillary angioproliferation. 49This is consistent with similar clinical and radiological presentation.
- Idiopathic pulmonary arterial hypertension
- Absence of interlobular septal thickening
- Peripheral lung oligemia
- Chronic pulmonary thromboembolism
- Absence of interlobular septal thickening
- Presence of vascular pruning
PVOD Treatment
The definitive treatment for PVOD is bilateral lung transplantation. This is supported by the 2015 ESC/ERS Guidelines for Pulmonary Hypertension, which recommend listing PVOD patients for transplantation at diagnosis.3, 69 Pulmonary veno-occlusive disease was significantly associated with a higher risk of dying while awaiting transplantation compared with PAH.70
A combination of targeted PAH therapy and immunomodulatory and supportive treatments is used to manage PVOD while patients await lung transplantation. Cautious use of PAH drugs such as prostacyclin, endothelin-1, and NO pathway therapies is recommended, as PVOD patients may develop hemodynamic compromise and life-threatening pulmonary edema.71 Approximately 20-50% of PVOD/PCH patients with PAH-specific therapy32,72,73, and 75% of PVOD patients receiving calcium channel blockers experience these complications.32
Treatment with the immunomodulatory drug imatanib as an adjunct to PAH therapy has yielded positive results. Ogawa, et al, reported significant improvement of the World Health Organization functional class and serum brain natriuretic peptide concentration, as well as reduction of mean pulmonary artery pressure and prolonged survival.74
General supportive measures include counseling patients to avoid concomitant medication such as beta-adrenergic receptor blockers, which can precipitate pulmonary hypertension or interfere with the metabolism of vitamin K antagonist anticoagulation therapy, as well as to limit physical activity to tolerance.
Oxygen therapy can be prescribed for individuals with resting or exercise-induced hypoxemia to maintain arterial oxygen saturation greater than 90%.75 Warfarin is routinely used in patients with idiopathic PAH; however, it should be prescribed cautiously in PVOD patients, owing to its association with alveolar hemorrhage. 8 Symptomatic right ventricular volume overload may be treated with diuretics under close supervision to avoid hemodynamic compromise.
Conclusion
Pulmonary veno-occlusive disease is a rare entity that causes severe pulmonary hypertension and carries a poor prognosis. Often these patients are misdiagnosed, as PVOD clinical symptoms and signs are similar to those seen in other forms of PAH/PH. Radiologists play an important role in diagnosing PVOD; CT criteria are paramount in the minimally invasive approach to PVOD recognition. Awareness and recognition of centrilobular ground glass opacities, interlobular septal thickening, and mediastinal lymphadenopathy on CT in patients with relevant demographics and risk factors allows for a high index of suspicion for PVOD. This, in turn, can contribute to timely diagnosis and early referral for lung transplantation.
References
- Montani D, Achouh L, Dorfmuller P, et al. Pulmonary venoocclusive disease: clinical, functional, radiologic, and hemodynamic characteristics and outcome of 24 cases confirmed by histology. Medicine. (Baltimore) 2008; 87(4):220e33.
- Heath D, Segel N, Bishop J. Pulmonary veno-occlusive disease. Circulation. 1966; 34: 242–248.
- Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2015; 46: 903–975.
- Holcomb BW Jr, Loyd JE, Ely EW, Johnson J, et al. Pulmonary veno-occlusive disease: a case series and new observations. Chest. 2000; 118: 1671–1679.
- Mandel J, Mark EJ, Hales CA. Pulmonary veno-occlusive disease. Am J Respir Crit Care Med. 2000; 162: 1964–1973.
- Rambihar V, Fallen E, Cairns J. Pulmonary veno-occlusive disease: antemortem diagnosis from roentgenographic and hemodynamic findings. CMA Journal. 1979; 120:1519-1522.
- Woerner C, Cutz E, Yoo S, et al. Pulmonary veno-occlusive disease in childhood. Chest. 2014; 146(1):167-174.
- Rabiller A, Jais X, Hamid A, et al. Occult alveolar haemorrhage in pulmonary veno-occlusive disease. Eur Respir J. 2006; 27: 108–113.
- McGoon M, Gutterman D, Steen V et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension. Chest. 2004; 126(1):14S-34S.
- Balko R, Edriss H, Nugent K, et al. Pulmonary veno-occlusive disease: An important consideration in patients with pulmonary hypertension. Respir Med. 2017 Nov; 132:203-209.
- Szturmowicz M, Kacprzak A, Szołkowska M, et al. Pulmonary veno-occlusive disease: pathogenesis, risk factors, clinical features and diagnostic algorithm — state of the art. Adv Respir Med. 2018; 86(3).
- Escamilla R, Hermant C, Berjaud J, et al. Pulmonary veno-occlusive disease in a HIV-infected intravenous drug abuser. Eur Respir J. 1995; 8: 1982–1984.
- Ruchelli ED, Nojadera G, Rutstein RM, et al. Pulmonary veno-occlusive disease. Another vascular disorder associated with human immunodeficiency virus infection? Arch Pathol Lab Med. 1994; 118: 664–666
- Hourseau M, Capron F, Nunes H, et al. Veino-occlusive pulmonaire et infection par le VIH. [Pulmonary veno-occlusive disease in a patient with HIV infection. A case report with autopsy findings]. Ann Pathol. 2002; 22: 472–475.
- Williams LM, Fussell S, Veith RW, et al. Pulmonary veno-occlusive disease in an adult following bone marrow transplantation. Case report and review of the literature. Chest. 1996; 109: 1388–1391.
- Kuga T, Kohda K, Hirayama Y, et al. Pulmonary venoocclusive disease accompanied by microangiopathic haemolytic anaemia 1 year after a second bone marrow transplantation for acute lymphoblastic leukemia. Int J Hematol. 1996; 64: 143–150.
- Troussard X, Bernaudin JF, Cordonnier C, et al. Pulmonary veno-occlusive disease after bone marrow transplantation. Thorax. 1984; 39: 956–957.
- Salzman D, Adkins DR, Craig F, Freytes C, LeMaistre CF. Malignancy-associated pulmonary veno-occlusive disease: report of a case following autologous bone marrow transplantation and review. Bone Marrow Transplant. 1996; 18: 755–760.
- Seguchi M, Hirabayashi N, Fujii Y, et al. Pulmonary hypertension associated with pulmonary occlusive vasculopathy after allogeneic bone marrow transplantation. Transplantation. 2000; 69: 177–179.
- Hackman RC, Madtes DK, Petersen FB, Clark JG. Pulmonary veno-occlusive disease following bone marrow transplantation. Transplantation. 1989; 47: 989–992.
- Bunte MC, Patnaik MM, Pritzker MR, et al. Pulmonary veno-occlusive disease following hematopoietic stem cell transplantation: a rare model of endothelial dysfunction. Bone Marrow Transplant. 2008; 41: 677–686.
- Dorfmuller P, Humbert M, Perros F, et al. Fibrous remodelling of the pulmonary venous system in pulmonary arterial hypertension associated with connective tissue diseases. Hum Pathol. 2007; 38: 893–902.
- Johnson SR, Patsios D, Hwang DM, et al. Pulmonary veno-occlusive disease and scleroderma associated pulmonary hypertension. J Rheumatol. 2006; 33: 2347–2350.
- Zhang L, Visscher D, Rihal C, et al. Pulmonary veno-occlusive disease as a primary cause of pulmonary hypertension in a patient with mixed connective tissue disease. Rheumatol Int. 2007; 27: 1163–1165.
- Rounds S, Cutaia M. Pulmonary hypertension: pathophysiology and clinical disorders. In: Baum G, Crapo J, Celli B, Karlinsky J, editors. Textbook of Pulmonary Diseases. Philadelphia: Lippincott-Raven, 1998: 1273-1295.
- Eyries M, MontaniD, GirerdB,etal. EIF2AK4 mutations cause pulmonary veno-occlusivedisease,arecessiveformofpulmonary hypertension. Nat Genet. 2014; 46:65-9.
- Nossent EJ, Antigny F, Montani D, et al.Pulmonary vascular remodelling patterns and expression of general control nonderepressible 2 (GCN2)in pulmonary veno-occlusive disease. J Heart Lung Transplan. 2018 May;37(5):647-655
- Montani D, Lau EM, Descatha A, et al. Occupational exposure to organic solvents: a risk factor for pulmonary veno-occlusive disease. Eur Respir J. 2015; 46(6): 1721–1731.
- Johnson SR, Patsios D, Hwang DM, et al. Pulmonary veno-occlusive disease and scleroderma associated pulmonary hypertension. J Rheumatol. 2006;33(11):2347e50.
- Morassut PA, Walley VM, Smith CD. Pulmonary veno-occlusive disease and the CREST variant of scleroderma. Can J Cardiol. 1992;8(10):1055e8.
- Dorfmuller P, Montani D, Humbert M. A walk on the far side of the lung e pulmonary venous involvement in patients suffering from systemic sclerosis-associated pulmonary arterial hypertension. Eur Respir J. 2010;35(1):6e8.
- Montani D, Lau EM, Dorfmüller P, Girerd B et al. Pulmonary veno-occlusive disease. Eur Respir J. 2016 May; 47(5):1518-34.
- Hoffstein V, Ranganathan N, Mullen JB. Sarcoidosis simulating pulmonary veno-occlusive disease. Am Rev Respir Dis. 1986; 134 (4):809e11.
- Zhang L, Visscher D, Rihal C, et al. Pulmonary veno-occlusive disease as a primary cause of pulmonary hypertension in a patient with mixed connective tissue disease. Rheumatol Int. 2007 Oct; 27(12):1163-5. Epub 2007 May 23.
- Hamada K, Teramoto S, Narita N, et al. Pulmonary veno-occlusive disease in pulmonary Langerhans’ cell granulomatosis. Eur Respir J. 2000 Feb; 15(2):421-3.
- Kokturk N, Demir N, Demircan S, et al. Pulmonary venoocclusive disease in a patient with a history of Hashimoto’s thyroiditis. Indian J Chest. Dis Allied Sci 2005; 47(4):289e92.
- Swift G, Gibbs A, Campbell I, Wagenvoort C, et al. Pulmonary venoocclusive disease and Hodgkin’s lymphoma. Eur Resp J 1993; 6: 596–598
- Ibrahim N, Burnley H, Gaber K, et al. Segmental pulmonary veno-occlusive disease secondary to lung cancer. J Clin Pathol. 2005; 58(4):434-436.
- Seguchi M, Hirabayashi N, Fujii Y, et al. Pulmonary hypertension associated with pulmonary occlusive vasculopathy after allogeneic bone marrow transplantation. Transplantation. 2000; 69(1):177e9.
- Salzman D, Adkins DR, Craig F, et al. Malignancy-associated pulmonary veno-occlusive disease: report of a case following autologous bone marrow transplantation and review. Bone Marrow Transplant. 1996; 18(4): 755e60.
- Mukai M, Kondo M, Bohgaki T, et al. Pulmonary veno-occlusive disease following allogeneic peripheral blood stem cell transplantation for chronic myeloid leukaemia. Br J Haematol. 2003; 123(1):1.
- Canny G, Arbus G, Wilson G, et al. Fatal pulmonary hypertension following renal transplantation. Brit J Dis Chest. 1985; 79(2):191-195.
- Izbicki G, Shitrit D, Schechtman I, et al. Recurrence of pulmonary veno-occlusive disease after heart lung transplantation. J Heart Lung Transplant. 2005; 24(5):635e7.
- Ranchoux B, Günther S, Quarck R, et al. Chemotherapy-induced pulmonary hypertension: role of alkylating agents. Am J Pathol. 2015; 185(2): 356–371.
- Perros F, Günther S, Ranchoux B, et al. Mitomycin-Induced Pulmonary Veno-Occlusive Disease: Evidence from human disease and animal models. Circulation. 2015; 132(9): 834– 847.
- Gagnadoux F, Capron F, Lebeau B. Pulmonary veno-occlusive disease after neoadjuvant mitomycin chemotherapy and surgery for lung carcinoma. Lung Cancer. 2002; 36(2):213e5.
- Shahab N, Haider S, Doll DC. Vascular toxicity of antineoplastic agents. Semin Oncol. 2006; 33(1):121e38.
- Townend JN, Roberts DH, Jones EL, et al. Fatal pulmonary venoocclusive disease after use of oral contraceptives. Am Heart J. 1992; 124:1643–1644.
- Lantuéjoul S, Sheppard M, Corrin B, et al. Pulmonary venoocclusive disease and pulmonary capillary hemangiomatosis: a clinicopathologic study of 35 cases. Am J Surg Pathol. 2006; 30(7):850-857.
- Wagenvoort CA, Wagenvoort N. The pathology of pulmonary veno-occlusive disease. Virchows Arch A Pathol Anat Histol. 1974; 364: 69–79.
- Pietra GG, Capron F, Stewart S, et al. Pathologic assessment of vasculopathies in pulmonary hypertension. J Am Coll Cardiol. 2004; 43: Suppl., 25S–32S.
- Perros F, Cohen-Kaminsky S, Gambaryan N, et al. Cytotoxic cells and granulysin in pulmonary arterial hypertension and pulmonary veno-occlusive disease. Am J Respir Crit Care Med. 2013; 187: 189–196.
- Hadinnapola C, Bleda M, Haimel M, et al. NIHR BioResource–Rare Diseases Consortium; UK National Cohort Study of Idiopathic and Heritable PAH. Phenotypic Characterization of Mutation Carriers in a Large Cohort of Patients Diagnosed Clinically With Pulmonary Arterial Hypertension. Circulation. 2017; 136(21): 2022–2033.
- Best DH, Sumner KL, Smith BP, et al. EIF2AK4 Mutations in Patients Diagnosed With Pulmonary Arterial Hypertension. Chest. 2014; 145: 231–236.
- Wilson GJ, Bunpo P, Cundiff JK, et al. The eukaryotic initiation factor 2 kinase GCN2 protects against hepatotoxicity during asparaginase treatment. Am J Physiol Endocrinol Metab. 2013; 305: E1124–E1133.
- Dorfmuller P, Perros F, Balabanian K, Humbert M. Inflammation in pulmonary arterial hypertension. Eur Resp J. 2003; 22(2):358-363.
- Günther S, Perros F, Rautou PE, et al. Understanding the Similarities and Differences between Hepatic and Pulmonary Veno-Occlusive Disease. Am J Pathol. 2019 Jun; 189(6):1159-1175.
- Thomas de Montpréville V, Dulmet E, et al. Lymph node pathology in pulmonary veno-occlusive disease and pulmonary capillary haemangiomatosis. Virchows Arch. 2008; 453(2): 171–176.
- François C, Schiebler M. Imaging of pulmonary hypertension. Radiologic Clinics of North America. 2016; 54(6):1133-1149.
- Grunig E, Barner A, Bell M, et al. Non-invasive diagnosis of pulmonary hypertension: ESC/ERS Guidelines with updated commentary of the Cologne consensus conference 2011. Int J Cardiol. 154S:S3–S12
- Mineo G, Attinà D, Mughetti M, et al. Pulmonary veno-occlusive disease: the role of CT. Radiol Med. 2014 Sep; 119(9):667-73.
- Resten A, Maitre S, Humbert M et al. Pulmonary hypertension: CT of the chest in pulmonary venoocclusive disease. AJR Am J Roentgenol. 2004 183:65–70.
- Szturmowicz M, Kacprzak A, Burakowska B, et al. Centrilobular nodules in high resolution computed tomography of the lung in IPAH patients — preliminary data concerning clinico-radiological correlates. Pneumonol Alergol Pol. 2016; 84(5):265-270.
- Dufour B, Maître S, Humbert M, et al. Highresolution CT of the chest in four patients with pulmonary capillary hemangiomatosis or pulmonary veno-occlusive disease. Am J Roentgenol. 1998; 171(5):1321-1324.
- Swensen S, Tashjian J, Myers J et al. Pulmonary veno-occlusive disease: CT findings in eight patients. Am J Roentgenol. 1996; 167(4):937-940.
- Frazier A, Franks T, Mohammed T, et al. Pulmonary venoocclusive disease and pulmonary capillary hemangiomatosis. RadioGraphics. 2007; 27(3):867-882
- Nolan RL, McAdams HP, Sporn TA, et al. Pulmonary cholesterol granulomas in patients with pulmonary artery hypertension: chest radiographic and CT findings. Am J Roentgenol. 1999; 172(5): 1317–1319.
- rip P, Girerd B, Bogaard HJ, et al. Diffusion capacity and BMPR2 mutations in pulmonary arterial hypertension. Eur Respir J. 2014; 43: 1195–1198.
- Montani D, Jais X, Price L et al. Cautious epoprostenol therapy is a safe bridge to lung transplantation in pulmonary veno-occlusive disease. Eur Resp J. 2009; 34(6):1348-1356.
- Wille KM, Sharma NS, Kulkarni T, et al. Characteristics of patients with pulmonary venoocclusive disease awaiting transplantation. Ann Am Thorac Soc. 2014; 11: 1411–1418.
- Humbert M, Lau EM, Montani D, et al. Advances in therapeutic interventions for patients with pulmonary arterial hypertension. Circulation. 2014; 130: 2189–2208.
- Montani D, Girerd B, Jaïs X, et al. Clinical phenotypes and outcomes of heritable and sporadic pulmonary veno-occlusive disease: a population-based study. Lancet Respir Med. 2017; 5(2): 125–134.
- Hadinnapola C, Morrell NW. Pulmonary veno-occlusive disease: characterising a rare but important disease. Lancet Respir Med. 2017; 5(2): 89–90.
- Ogawa A, Miyaji K, Matsubara H. Efficacy and safety of long-term imatinib therapy for patients with pulmonary veno- occlusive disease and pulmonary capillary hemangiomatosis. Respir Med. 2017; 131: 215–219.
- Montani D, O’Callaghan DS, Savale L,et al.Pulmonary veno-occlusive disease: recent progress and current challenges. Respir Med. 2010 Jul; 104 Suppl 1:S23-32.
References
Citation
SVK L.Pulmonary Veno-Occlusive Disease and the Role of the Radiologist. Appl Radiol. 2021; (4):19-26.
July 15, 2021