PET/CT neuroimaging applications in dementia
Images







Dr. Mountz is a Professor of Radiology, Director of NeuroNuclear Medicine, and Chief of The Division of Nuclear Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA.
The diversity of neuroimaging examinations on positron emission tomography (PET)/computed tomography (CT) scanners is more limited than those possible on dedicated neuro-PET or neuro-CT equipment, since the design of most PET/CT scanners is optimized for the performance of body oncology imaging protocols. However, most PET/CT scanners can provide excellent PET and CT brain scans if the acquisition and reconstruction parameters are appropriately selected. This review will highlight the role of neuro-PET/CT in the evaluation of dementia.
Central nervous system PET radiopharmaceuticals
There are 3 main classes of radiopharmaceuticals now available for PET brain imaging: 1) regional cerebral blood flow tracers; 2) general metabolic tracers; and 3) specific receptor or molecular binding agents.
The major PET radiopharmaceutical used to measure cerebral perfusion is O-15 H 2 O. 1 While brain perfusion is critical for delivery of all tracers to the brain, the practical application for region cerebral perfusion PET alone is currently mainly limited to the assessment of cerebrovascular disease.
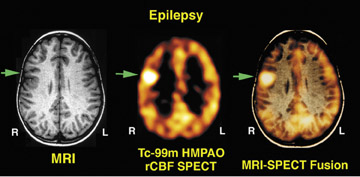
The second major class of radiopharmaceuticals is made up of those that specifically measure brain metabolism of oxygen or glucose. These radiopharmaceuticals are transported to the brain tissues by regional cerebral blood flow, but subsequent tissue distribution reflects regional cerebral energy utilization. The PET radiopharmaceutical predominantly used is fluorine-18 (F-18) 2-fluoro-2-deoxy-D-glucose (FDG), 2 which has an important role in the diagnosis and assessment of dementia, epileptogenic focus localization, and diagnosis of viable high-grade tumor from areas of radiation or chemotherapy-induced cerebral necrosis.
The third class of radiotracers that are important in brain imaging includes central nervous system receptor-binding or transporter-dependent agents that measure neuronal receptor density, membrane transport, or a more general cerebral metabolic pathway.
Numerous reviews have been published describing the hundreds of PET tracers that have been developed for application in brain PET imaging, primarily for brain receptor studies or metabolic incorporation into essential biochemical pathways. 3,4 After intravenous (IV) injection, these tracers initially follow first-order kinetics compartmental distribution, since their delivery depends on cerebral blood flow. Over time, there is clearance of nonspecific uptake, and the delayed scan reflects the more specific process under investigation.
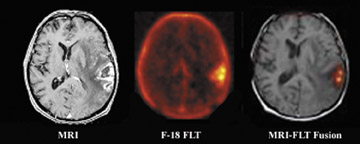
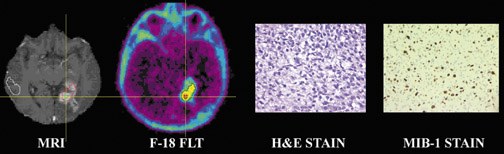
Positron emission tomography and PET/CT are beginning to play a dominant role in brain tumor assessment using [ 18 F]-fluoro-3-deoxy-3-L-fluorothymidine ([ 18 F]FLT), l-[methyl- 11 C] methio-nine (C-11 MET) and 3,4-dihydroxy-6- 18 F-fluoro-L-phenylalanine (18 F-FDOPA) in addition to F-18 FDG. In addition, N-methyl-[ 11 C]2-(4':-methylaminophenyl)-6-hydroxybenzothiazole (C-11 Pittsburgh compound B [PIB]) is emerging as a specific radiotracer for assessing brain amyloid accumulation in the diagnosis of Alzheimer's disease (AD).
Dementia
Approximately 3% to 4% of the adult U.S. population exhibits significant cognitive impairment. In general, the causes of dementia include primary neurodegenerative disorders, with the most prevalent being AD, followed by frontotemporal dementia, Lewy body dementia, Parkinsonian dementia, progressive supranuclear palsy, Pick's disease, cortical basilar degeneration, Huntington's disease, and Wilson's disease. 5 Vascular dementias are categorized as multi-infarct, Binswanger's, cerebral autosomal dominant arteriopathy with subcortical infarctions, and leukoencephalopathy. Inflammatory etiologies include multiple sclerosis and vasculitis. Infectious etiologies include syphilis, human immunodeficiency virus, Lyme disease, and other viral and fungal diseases. Cancers are a rare cause of dementia, although dementia can be attributed to a primary result of the disease, metastatic disease to the brain, and paraneoplastic syndromes. Other causes and physical abnormalities include trauma and hydrocephalus.
The prevalence of dementia in the population increases significantly with age, with approximately 13% of the population having dementia in the 77- to 84-year-old range, and almost 50% in the population ≥95 years. With the increasing age of the U.S. population, dementia is expected to be an increasingly significant healthcare problem. It has been documented that approximately 77% of all dementias are attributable to AD or Lewy body dementia. 6
Alzheimer's disease
Alzheimer's disease was first described by Alois Alzheimer in 1906 as an unusual disease of the cerebral cortex with primary clinical symptomatology as a presenile dementia that affected a woman in her 50s. It caused memory loss, disorientation, hallucinations, and, ultimately, death by the age of 55. The classic neuropathological changes were identified as senile plaques and neurofibrillary tangles. He also described a granulovascular degeneration and amyloid angiopathy. The diagnosis of AD has traditionally been through the criteria developed by the National Institute of Neurological and Communicative Diseases and Stroke/ Alzheimer's Disease and Related Disorders Association (NINCDS/ADRDA). 7 The NINCDS/ADRDA criteria for dementia are established by clinical examination and documented by the Mini Mental Test or Blessed Dementia Scale and are confirmed by a neuropsychological examination. A diagnosis of Alzheimer's dementia requires cognitive deficits in ≥2 areas, with progressive worsening of memory and other cognitive function. There should be no disturbances in consciousness. The age of onset is typically between 40 and 90 years, most often after 65 years. In addition, the absence of systemic disorders or other brain diseases is required, as these can confound the diagnosis of AD.
The 2 basic types of AD are familial and sporadic . Familial AD (FAD) is a rare form of AD, affecting <10% of AD patients. All FAD is early-onset, meaning the disease develops before age 65. Apolipoprotein E (APOE) epsilon4 gene dose (ie, the number of epsilon4 alleles in a person's APOE genotype) is associated with a higher risk of AD and a younger age at dementia onset 8 and correlates with reduced regional hypometabolism in the brains of patients with AD. In addition, advanced age, prior head trauma, low educational levels, and gender (with female greater than male predominance) have been associated with an increased risk for AD.
The rationale for imaging as a diagnostic tool for AD is based on the disease-associated reduction in metabolic brain activity, which can be visualized on F-18 FDG brain PET. There is a reduction of brain glucose metabolism identified on PET caused by reduced neuronal metabolism and synaptic activity in areas of neuronal degeneration from excessive amyloid deposition. The characteristic findings in AD are as follows: 1) there is often bilateral involvement with asymmetry of F-18 FDG reduction in the posterior temporoparietal cortical areas; 2) reduction of metabolism and blood flow to the posterior cingulate gyrus; 3) relatively early onset (<65 years) have more marked reduction of F-18 FDG uptake; 4) less commonly, primary visual cortex involvement (which is more common in Lewy body dementia); 6) relative sparing of the corpus striatum, thalamus, and primary sensorimotor cortex; 7) late involvement of the frontal lobes; and 8) coexisting micro- or macrovascular disease involvement that results in neuronal injury and death.
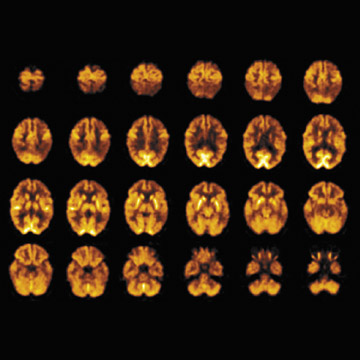
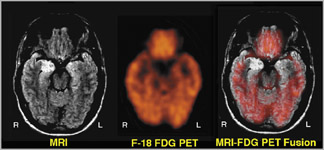
Imaging of AD with F-18 FDG- PET-- Accurate and early diagnosis of AD is vital to ensure that patients receive proper treatment, that research is targeted correctly, and that prevention and cures are found. However, it can be difficult to distinguish between AD and other forms of dementia, or even to distinguish it from other reversible disorders. The standard tools for assessing AD include neuropsychological or cognitive evaluation, physical examination, neurological examination, laboratory testing, neuroimaging, behavioral assessment, and patient history. The diagnosis of AD by F-18 FDG-PET imaging has been reported to have a sensitivity of 93% and a specificity of 63%. 9 Figure 1 shows an F-18 FDG-PET scan in a 54-year-old woman with early onset of dementia who meets the clinical diagnosis of frontotemporal dementia and AD. Symptom onset was 4 years before the PET scan, and the current Folstein Mini Mental Status Examination (Folstein MMSE) was 17 of 30. The CT scan showed mild nonspecific, nonlobar atrophy.
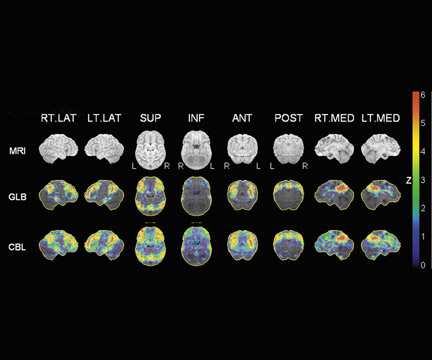
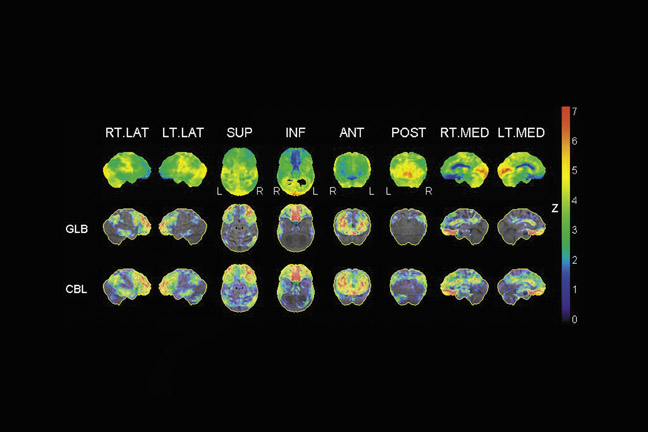
As an aid in evaluating the F-18 FDG- PET scans of patients suspected of having AD, several automated statistical analysis methods have been developed. The 3-dimensional stereotactic surface projection (3D SSP) analysis method 10 is used to analyze patients, such as the patient described in Figure 1. The method generates comprehensive image presentations and objective diagnostic indices for individual patients compared with age-range-matched normal controls by calculating a Z-score on a pixel-by-pixel basis displayed in 3D SSP views for visual inspections (Figure 2).
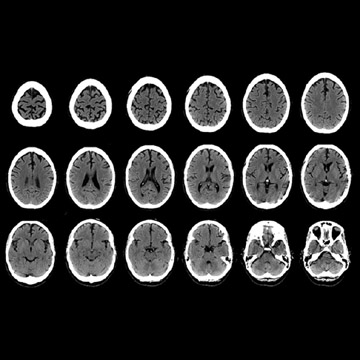
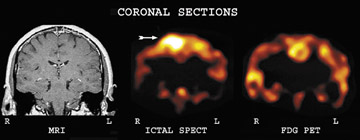
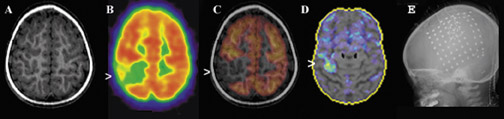
The added value of CT on PET/CT scans is illustrated by the case of a 48-year-old woman who was evaluated for characterization of dementia that was suspected to be Creutzfeldt-Jakob disease based on neurologic examination (Figures 3 through 5). The FDG-PET scan showed markedly reduced F-18 FDG uptake in the posterior temporoparietal regions; sparing of the sensorimotor cortex, corpus striatum, thalamus, and cerebellum that was characteristic of moderately severe AD. Since this scan was acquired on a standard PET/CT scanner for which the CT scan is used for attenuation correction, by changing the mAs and kVp to brain technique, a diagnostic brain CT scan can be obtained without added cost or time. The CT scan showed that the dementia was not attributable solely to specific atrophy in these brain regions (Figures 4 and 5).
Figure 6 shows another example of an F-18 FDG-PET scan; this one is from a 72-year-old woman who was being evaluated because of concerns regarding a 6-month cognitive decline. On questioning, however, it was determined that her memory loss had begun approximately 4 years prior to admission. Her Folstein MMSE score was 9 of 30, and she satisfied the NINCDS/ADRDA criteria for probable AD. The 3D SSP statistical map showed decrease metabolism in the posterior temporoparietal lobes, with the right worse than the left.
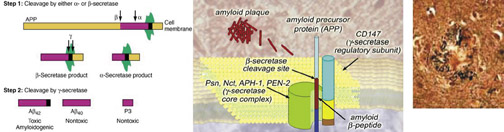
Amyloid b-precursor protein and PET imaging of C-11 PIB-- Alzheimer's disease is a widespread, neurodegenerative, dementia-inducing disorder of the elderly that has been estimated to affect >4 million people in the United States alone. 11 The disease is characterized by synaptic loss and neuronal death in the cerebral cortex and the hippocampus, with the presence of extensive extracellular amyloid plaques and intracellular neurofibrillary tangles (Figure 7). 12 The accumulation of amyloid protein (Aβ) in the brain is an important step in the pathogenesis of AD. Amyloid β-precursor protein (AβPP) was identified in 1987, on the basis of the sequence of the first 28 amino acids of the A β peptide that had been purified from AD meningeal blood vessels. 13 The cloning studies of 4 laboratories led to the identification of a single gene locus named amyloid b(A4) precursor protein, on chromosome 21q21.2. Other genes localized to chromosomes 19 and 11 (denoted APLP1 and APLP2 for Amyloid [Alzheimer] Precursor Protein 1 and 2) are considered to be members of the APP gene family, although they do not encode the Aβ sequence.
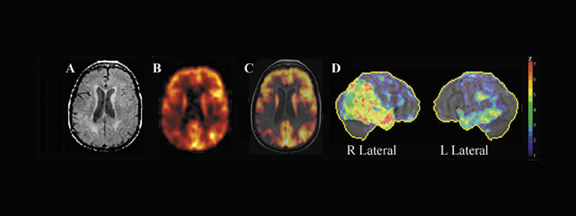
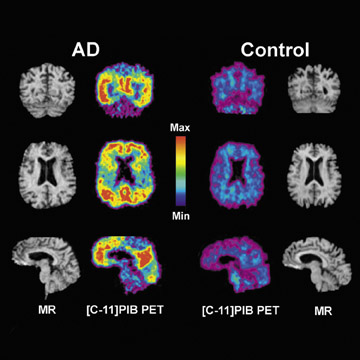
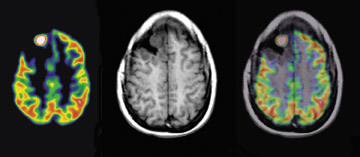
Pittsburgh Compound-B is an amyloid-imaging PET tracer. The main compound is derived from thioflavin T, similar to Congo Red, and is believed to bind to sites on the amyloid peptide fibrils. Klunk et al 14 studied the use of PIB to assess amyloid in 16 patients with diagnosed mild AD as compared with 9 controls. 14 Alzheimer's disease patients show marked retention of PIB in areas of association cortex that contain large deposits of amyloid. Compared with controls, AD patients typically showed marked retention of PIB in areas of association cortex known to contain large amounts of amyloid deposits in AD (Figure 8). In cortical areas, PIB retention correlated inversely with F-18 FDG uptake. This relationship was most robust in the parietal cortex. The results suggest that PET imaging with the novel tracer C-11 PIB can provide quantitative information on amyloid deposits in humans, and should be of value in the diagnosis of AD and the development of antiamyloid therapies.
Center for Medicare and Medicaid Services decision memorandum for PET imaging in suspected dementia-- The Center for Medicare and Medicaid Services (CMS) issued a decision memorandum for positron emission tomography and other neuro-imaging devices for suspected dementia on September 15, 2004. 15 The CMS decided that an F-18 FDG brain PET scan is reasonable and necessary in patients with a recently established diagnosis of dementia with documented cognitive decline for at least 6 months who have met the criteria for both AD and frontal temporal dementia, and who have been evaluated for specific alternate neurodegenerative diseases or causative factors for which the cause of clinical symptoms remains uncertain. The coverage criterion for AD requires the additional information to be met 15 :
- The onset, clinical presentation, or course of cognitive impairment is atypical for AD, and frontal temporal dementia is suspected as an alternative neuro- degenerative cause of cognitive decline. Specifically, symptoms such as social dysinhibition, awkwardness, difficulties with language, or loss of executive function are more prominent early in the course of frontal temporal dementia than the memory loss typical of AD.
- The patient must have had a comprehensive clinical evaluation encompassing a medical history including formal documentation of cognitive decline by 2 time points with intervals of at least 6 months apart. This should be aided by cognitive scales of neuropsychological testing, laboratory tests, and structural imaging, such as MRI or CT.
- The patient has to be evaluated by a physician experienced in the diagnosis and assessment of dementia, and in that evaluation a likely or specific neurodegenerative disease or cause of clinical symptoms was not identified and information available through F-18 FDG-PET is reasonably expected to clarify the differential diagnosis between frontal temporal dementia and AD.
- A brain single-photon emission CT (SPECT) or a prior F-18 FDG-PET scan should not have been performed for this same indication.
- The referring or billing provider will collect and maintain and furnish upon the request of CMS the following documentation to verify that conditions for coverage described have been met: Date of onset of symptoms, Mini mental status examination or similar test score, report from any neuropsychological testing performed, diagnosis of clinical syndrome (eg, mild cognitive impairment, dementia, etc.), presumptive cause (eg, possible, probable, or uncertain AD, results of structural imaging-eg, MRI and CT), relevant laboratory tests (B12 or thyroid hormone levels), and any prescribed medications (in- cluding the quantity and name).
Frontotemporal dementia
The term frontotemporal dementia refers to a group of diseases that are commonly misdiagnosed as AD. Frontotemporal dementia is 1 of 3 clinical syndromes associated with frontotemporal lobar degeneration. Frontotemporal dementia selectively affects the frontal lobe of the brain and may extend backward to the temporal lobe. Symptoms can be classified into 2 groups that underlie the functions of the frontal lobe: behavioral symptoms (and/or personality change) and symptoms related to problems with executive function. Behavioral symptoms include apathy and aspontaneity or, oppositely, disinhibition. Apathetic patients may become socially withdrawn and stay in bed all day or no longer take care of themselves. Disinhibited patients can make inappropriate (sometimes sexual) comments or perform inappropriate acts. Executive function is the cognitive skill of planning and organizing-patients often become unable to perform skills that require complex planning or sequencing.
Frontotemporal dementia has been shown to be associated with brain re-gions with reduction of glucose metabolism, significant hypometabolism in extensive prefrontal areas, in cingulate gyri, in anterior temporal regions, and in the left inferior parietal lobule. 16 Figure 9 shows an F-18 FDG-PET scan from a 54-year-old man with frontotemporal dementia with a recent MMSE score of 26 of 30. Figure 10 shows the 3D SSP map for this patient.
Conclusion
There is a growing demand for early and accurate diagnosis of Alzheimer's disease in the United States due to the increase in the expected human life-span and the desire to remain active and productive into the later years of life. This is more important considering the recent advancements in therapies for treatment of early disease. In addition, improvements in F-18 FDG-PET imaging capability and development of quantitative F-18 FDG-PET analysis methods have made this service more widely available. The recent coverage approval decision by the Center for Medical Services to allow PET to be used in the early diagnosis of Alzheimer's disease was an important step towards insurance coverage. Nuclear medicine physicians and radiologists now need to inform the referring physicians (mainly neurologists, family practice physicians, and geriatric psychiatrists) of the value of F-18 FDG-PET in the diagnosis of dementia.
Related Articles
Citation
PET/CT neuroimaging applications in dementia. Appl Radiol.
June 5, 2007