PET-CT in the evaluation of colorectal carcinoma
Images









Dr. Moadel is an Assistant Professor, Dr. Feng is an Assistant Professor, and Dr. Freeman is a Professor and the Vice Chair, Department of Nuclear Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY.
The imaging combination of 2-deoxy-2-[18F] fluoro-D-glucose (FDG) and positron emission tomography (PET) with computed tomography (CT) has revolutionized the evaluation of colorectal cancer in terms of staging, restaging, accurately assessing response to therapy, and surveillance of the “cured” patient. However, pitfalls exist; these include bowel uptake due to physiologic, iatrogenic, and infectious and inflammatory processes. The key to being able to differentiate malignant disease from artifactual uptake within the bowel often lies in pattern recognition and the ability to triangulate FDG uptake to normal- or abnormal-appearing bowel on CT. Using this pattern recognition, PET can be useful in identifying incidental premalignant or malignant lesions, and infectious and inflammatory bowel disease. An understanding of the physiologic processes that account for nonmalignant uptake allows one to better interpret PET/CT oncology studies.
Physiologic bowel uptake
FDG uptake in the gastrointestinal (GI) tract has been attributed to a physiologic process of the smooth muscle or, alternatively, intraluminal activity. Just as activity in voluntary muscles under active contraction is commonly seen during the FDG uptake phase (within 30 minutes of administration),1 it had been proposed that peristaltic smooth muscle action was responsible for bowel uptake. However, it is likely that FDG is excreted into the bowel lumen and is used by normal bacterial flora. Kim and coworkers2 noted that antiperistaltic constipation, and not diarrhea, is associated with focal and intense bowel uptake, and significant activity in fecal matter suggests an intraluminal and/or bacterial component to the activity. In a study by Jadvar et al,3 FDG PET scans were performed on normal subjects without intervention, with atropine to reduce peristalsis, and with sincalide (a cholecystokinetic) to promote peristalsis. The authors noted that there was no difference in uptake between the groups.3 Miraldi et al4 reported that bowel preparation with an iso-osmotic bowel solution eliminated bowel activity, which supports intraluminal, rather than peristaltic, smooth muscle activity. It is presumed that FDG enters the GI lumen via tight junctions that are present in between intestinal epithelial cells and are variably permeable, allowing for absorption from and excretion into the GI tract.2 FDG uptake has been noted specifically in the cecal/right colonic region and has been thought to be related to increased metabolic activity of Peyer’s patches (intra- and submucosal lymphoid tissue) that are more heavily concentrated in this region (Figure 1).5,6
Iatrogenic bowel uptake
FDG bowel uptake can be a result not only of intrinsic physiologic mechanisms, but also of extrinsic or iatrogenic causes, including the use of oral contrast for diagnostic CT studies and the effects of prescribed medications, such as metformin. High-density oral contrast can result in greater attenuation by low-dose CT energy X-rays (120 KeV) as compared with the higher positron gamma rays (511 KeV). Using oral contrast, the attenuation correction reconstruction process based on the CT data can lead to overestimation of FDG uptake in bowel by 20%. However, when attenuation-corrected and noncorrected images were evaluated, there were common visual discrepancies as a result of the presence of oral contrast media, but none were clinically significant.7 There were no alterations in the final diagnosis. While the oral contrast artifacts are not clinically significant in patient management, these artifacts could be completely eliminated by the use of a negative contrast agent, such as locust-bean gum.7,8
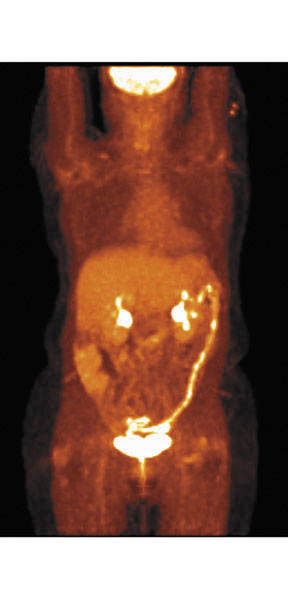
Systemic medications, such as metformin, can increase bowel uptake, which generally results in an increase in large and small bowel FDG uptake in a diffuse pattern (Figure 2). This pattern does not appear to occur with other diabetic medications. Metformin acts to enhance transfer of glucose from the vasculature to the intestinal epithelial cells and thereby increases glucose utilization within the GI tract by up to 60% in animal models, mediated by glucose transporters (GLUT 1,2,4) and by activation of protein kinases within the glycolytic pathway.9 These iatrogenic causes and patterns of artifactual uptake are important entities in the evaluation of bowel uptake and the differentiation of benign versus malignant etiologies.
Incidental neoplastic colorectal lesions
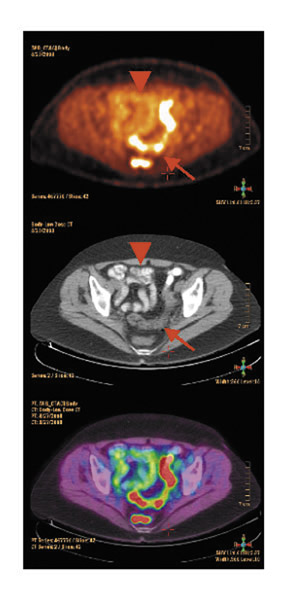
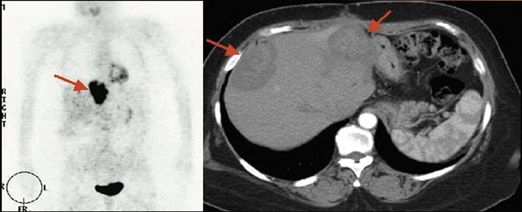
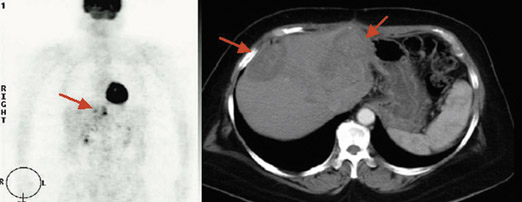
Despite possible intrinsic and iatrogenic causes for bowel uptake, the authors routinely recommend evaluation with colonoscopy when there is focal bowel uptake. This may be seen in patients being studied for an unrelated reason, such as a lung or breast neoplasm. Since there are a significant number of incidental true-positive premalignant or malignant lesions, it is preferable for such patients to undergo further investigation rather than missing a lesion. The pattern of diffusely increased uptake within the bowel is not associated with findings of cancer on colonoscopy and is thought to be related to normal intrinsic or iatrogenic causes, while a segmental pattern is associated with infectious or inflammatory causes such as colitis. A nodular focal or multifocal pattern is associated with a high risk of premalignancy or malignancy ranging from 59% to 100%,10-12 and colonoscopic evaluation is recommended. Examination of the simultaneously performed CT images often confirms the presence of a mass (Figure 3). It should be noted that lesions <1.7 cm are not detected on PET imaging. There is a correlation of standard uptake value (SUV) with severity of malignancy,13 likely due to upregulation of the glucose transporter (GLUT 1) caused by oncogene expression14,15 ; however, a cutoff value cannot be established due to significant overlap in SUV between low and high severity of malignancy.
Inflammatory lesions of the colon
While inflammatory lesions of the bowel are cause for false-positive findings in the oncology setting, PET/CT can be useful in the primary detection of infectious or inflammatory bowel disease, which is indicated by an intense segmental pattern.10 PET can be useful in determining the causes of fever of unknown origin, often pointing to bowel pathologies such as infectious or inflammatory colitis.16 It is also specifically useful in the detection of inflammatory bowel diseases (IBD) such as Crohn’s, with high sensitivity (73% to 85%) in comparison to endoscopic biopsy in the adult population. As with malignancies, the SUV correlates with disease severity in IBD.16,17 In children suspected of having Crohn’s disease, PET has a sensitivity of 98% and is recommended prior to endoscopic evaluation.18 In a small number of patients who have persistent watery diarrhea, abdominal pain, and weight loss but who also have negative colonoscopic and radiologic studies, PET reveals segmental regions of uptake. Kresnik et al19 reported that subsequent PET-directed colonoscopic biopsy revealed microscopic collagenous or eosinophilic colitis in patients who were not found to have mucosal abnormalities at colonoscopy.19 PET can also be instrumental in detecting disease activity in ulcerative colitis, with a sensitivity of 96% when compared with colonoscopic findings (Figure 4).20
Staging/restaging
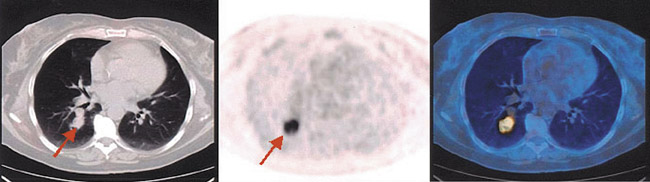
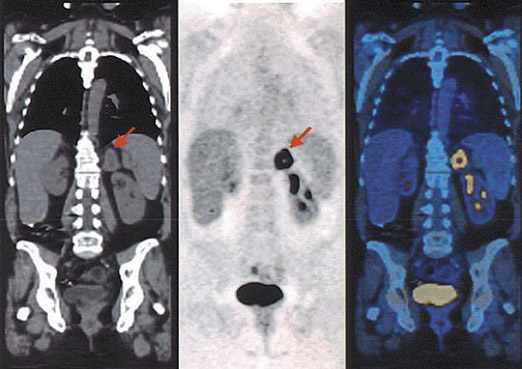
The aforementioned patterns should help to distinguish benign from premalignant or malignant pathology within the bowel. However, once the diagnosis of colorectal carcinoma has been made, usually by colonoscopy, the true value of FDG PET/CT is in the initial staging and detection of unknown disease that is not otherwise seen by other imaging modalities, and the resultant change that it directs in ultimate therapeutic management. After the initial diagnosis, a change of therapeutic management was instituted in 16% of patients with colorectal carcinoma due to PET findings of disease in unsuspected locations.21 CT can provide additional information concerning these lesions. It should be noted, however, that local lymph node metastases are not reliably seen by any imaging modality.21 Nahas et al22 reported that 13% of patients with locally advanced rectal cancer had metastatic disease on subsequent clinical follow-up, and PET was able to detect this disease a priori in almost all of these patients. PET/CT is able to outperform other imaging modalities in the detection of disease, and, when compared directly with whole-body 3T magnetic resonance imaging (MRI), PET/CT detected more pulmonary and lymph node metastases.23 However, PET is limited in detection of hepatic lesions <1 cm because of inherent resolution limitations. Contrast-enhanced PET/CT or manganese dipyridoxyl diphosphate (Mn-DPDP) contrast-enhanced hepatic MRI can be instrumental in revealing such metastases.24 Interestingly, when patients are preselected for curative hepatic resection based on PET results, 5-year survival increases from a historically established 30% to 58% because of more accurate staging.25 In addition, a change in clinical management is seen in 25% to 32% of patients.26 PET/CT is also a valuable tool in the detection of synchronous primary cancers, thereby changing management to address additional malignancies such as lung, breast, uterus, and thyroid.27 Primary lung lesions must be differentiated from colorectal metastases and treated accordingly (Figure 5). It should be noted, however, that PET is not sensitive in detecting mucinous colon cancers and can be a cause of false-negative results (Figure 6).28 Given the value of detecting unknown disease and the effect on patient management, PET/CT is an important tool for the initial staging of patients with colorectal cancer.
Response to therapy
FDG PET is invaluable in assessing response to therapy, especially therapies that cause anatomic abnormalities. These metabolic responses are often associated with only subtle changes on CT or MRI, and response can be appreciated only with the addition of PET imaging. Currently, there are several therapeutic modalities available for colorectal hepatic metastases, including hepatic resection, hepatic arterial chemotherapy (HAC) delivery, radiofrequency (RF) ablation, and intrahepatic yttrium-90 (90 Y) microspheres. Since many of these therapies cause significant anatomic alterations, PET/CT is often better able to detect response than CT alone (Figure 7). There is controversy as to whether HAC alone improves survival in patients with unresectable hepatic metastases,29 but the data suggests that it enhances response as an adjunct to the other mentioned therapies.30-32 PET/CT imaging can definitively show response of hepatic metastases in these clinical scenarios. This is particularly evident in the settings of RF ablation and hepatic resection, since the therapies themselves cause significant anatomic change.33 Additionally, PET can provide prognostic information in patients who undergo hepatic resection, in that lower preoperative SUVs are associated with longer survival.34 As with HAC, there is currently debate among surgeons whether RF ablation is as effective as hepatic resection. Preliminary evidence suggests that they are equivalent for tumors <3 cm, but RF ablation is associated with local recurrence in larger tumors, although long-term follow-up and a randomized controlled study are deemed necessary to confirm this.35 In the therapy of colorectal hepatic metastases with90 Y microspheres, PET is able to detect metabolic response while there is often no change on CT imaging.36
Patients with isolated pulmonary metastases often have longer survival following surgical resection, and PET/CT is an integral part of the staging process to identify those eligible for resection.37 Additionally, PET is utilized to evaluate the success of recently introduced therapeutic techniques such as RF ablation of pulmonary metastases.38 Hence the metabolic response to these local therapies (in addition to anatomic response and localization) is integral to determine the next steps in patient therapeutic management.
In addition to monitoring local therapies, FDG uptake reflecting metabolic response to systemic therapies often predicts survival in a multitude of malignancies, including colorectal cancer. In patients with locally advanced rectal cancer treated with neoadjuvant chemoradiation therapy, those who showed complete FDG PET response are more likely to have longer disease-free and overall survival.39,40 In patients with advanced colorectal cancer, >20% decrease in tumor SUV after 2 months of chemotherapy is associated with both longer progression-free and overall survival.41 The evaluation of metabolic response early in the course of disease can predict survival and offers the opportunity to modify the chemotherapeutic regimen when tumors are unresponsive, thereby sparing patient exposure to noneffective therapies.
Surveillance: Monitoring of recurrence
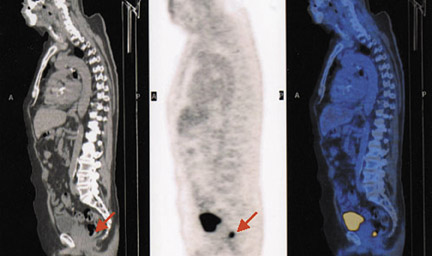
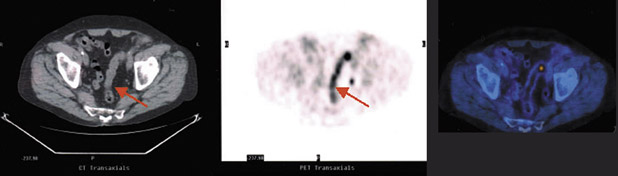
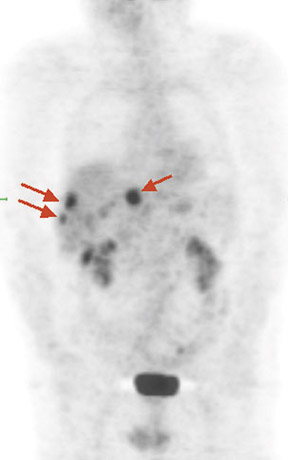
At Montefiore Medical Center, the great majority of oncologists are monitoring “cured” colorectal cancer patients with PET/CT as opposed to PET or CT alone. When recurrence or metastases are seen early with PET/CT and not necessarily seen on anatomic imaging alone, these patients are often at a treatable state of disease (ie, local recurrence, or surgically resectable hepatic or pulmonary metastases).42-44 In evaluation of recurrence, PET/CT is able to detect more lesions than anatomic imaging alone, with high sensitivity (95%) and high positive predictive value (96%)45 (Figure 8). The addition of contrast enhancement to the CT portion of the PET/CT helps to definitively localize hepatic lesions to the correct segment, which is essential for surgical planning.46 Often, patients are monitored with abdominal CT alone, with indeterminate results, in that postsurgical fibrosis cannot be distinguished from local recurrence. PET is especially useful in this situation, since fibrosis is not FDG-avid and recurrence will show uptake (Figure 9). Finding the cause for elevated carcinoembryonic antigen in post-curative monitoring is often elusive on anatomic imaging but can be clearly elucidated on PET imaging with sensitivity of >95% (Figure 10).47 In monitoring for recurrence, PET effects a change in therapeutic management in a substantial proportion (38% to 66%) of patients.48,50 PET is able to provide prognostic information,50 and PET/CT significantly improves restaging.51 Thus, PET/ CT is the diagnostic modality of choice in monitoring patients for colorectal cancer recurrence, providing accurate restaging and guiding patient management.
Conclusion
PET/CT is currently the preferred method for staging and restaging of patients with colorectal carcinoma. It also provides the most reliable means of monitoring patients for possible recurrence after a variety of therapeutic interventions, both for the primary lesion and sites of metastases.
Related Articles
Citation
. PET-CT in the evaluation of colorectal carcinoma. Appl Radiol.
November 5, 2008