Patient-Specific Imaging: Initial Impressions of Native TEQ
Images









Video Clip 1 , Video Clip 2 , Video Clip 3 , Video Clip 4 , Video Clip 5 , Video Clip 6
Dr. Richard G. Barr is a Professor of Radiology at Northeastern Ohio Universities College of Medicine (NEOUCOM) and is Director of Ultrasound, Forum Health, Western Reserve Care System
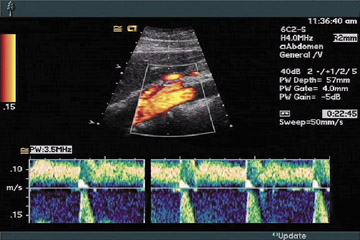
Ultrasound imaging has the advantages of being a real-time, multiplanar, nonionizing radiation imaging technique. However, the technique is limited by operator dependence [1, 2]. While other imaging modalities such as computed tomography, magnetic resonance imaging, and nuclear medicine adjust parameters to improve image quality and diagnostic information, these are usually standardized and programmed before the start of the examination. These parameters are used without change throughout the data acquisition. However, in ultrasound, the interaction of the sound beam with the patient varies significantly throughout the course of a standard examination. The sonographer therefore must adjust parameters continuously throughout the examination to optimize the image [3, 4]. There are multiple operator-dependent controls used to optimize the image in ultrasound [5]. Some of these are difficult and time-consuming to optimize. To overcome this limitation, ultrasound manufacturers have developed an automated optimization technique whereby with the push of one button, the image is optimized by the computer operating system. This technique is available from several manufacturers [6]. This technique decreases the number of buttons that must be adjusted to optimize an image. The technique corrects all of the most common technical errors in ultrasound, including unbalanced gain, undergained or overgained images, and refractive shadowing. This technique also has the capability of optimizing some parameters that are not available for the operator to adjust, such as lateral gain. However, these techniques optimize only a single image, and the scan is no longer optimized as soon as the probe is moved. This technique of image optimization has also been developed to manually optimize and present Doppler information (Figure 1; Online video clip 1) .
Native TEQ Technology
As opposed to TEQ ultrasound technology, which optimizes a single image, Native TEQ™ ultrasound technology (NTEQ) has been developed as a real-time technique to adjust the gain as well as other parameters while scanning. The computer is programmed to perform advanced real-time motion analysis in addition to accurately detecting and differentiating noise and artifacts from soft tissue. The image gain is automatically optimized in the axial and lateral dimensions in real-time, once the transducer touches the patient or anytime it is moved to a new acoustic window. This leads to several advantages. Image quality is optimized on the fly with real time analysis every few seconds. The optimization technique optimizes some parameters which the operator does not have the ability to adjust and, as a result, the images are of improved quality over that of manually adjusted images. Additionally, there is a significant decrease in the number of buttons adjustments a sonographer needs to adjust during the examination, which improves overall ergonomics. There are no gain or depth-gain-compensation (DGC) control adjustments needed while scanning, and the technique removes operator dependence on the adjustment of the scan, therefore providing a "standardized" image that is independent of the operator and specific to each patient. The technique can be used with other imaging techniques, such as harmonic imaging and compounding.
The robustness of the technique can be demonstrated by manually adjusting the initial image so the image is uninterpretable, and then turning on the technique, and within a few frames, the image is optimized (Figure 2; Online video clip 2) . Figure 3 demonstrates the technique during a routine scan of the retroperitoneum. The image on the left (A) is a frame just before an optimization, while the image on the right (B) is the frame immediately after the optimization (Online video clip 3) . Note the improved image quality obtained without any manual adjustments and the fact that there is a significant decrease in the reverberation artifact in the cyst. Figure 4 demonstrates the ability of the computer optimization to improve image quality over manual optimization. The image in Figure 4A is a testicle manually optimized. Note the refractive shadowing from the superior and inferior poles of the testicle. Figure 4B shows the image that has been optimized with NTEQ ultrasound technology. Note that the computer has the ability to eliminate the artifact because of its ability to control lateral gain. With the real-time optimization, spontaneous flow is often noted in larger blood vessels. Figure 5 (Online video clip 4) illustrates the blood flow visualized in the inferior vena cava (Figure 5B), which is not seen in the manually adjusted image (Figure 5A). This is appreciated best in real-time imaging.
The operator can adjust overall image intensity, making it brighter or darker for personal preferences. The rate at which optimization occurs can also be adjusted for each user preference. The technique is turned on with a single button and can be turned off by manually adjusting the gains or turning the technique off. In our experience, there are very few circumstances where using the technique is not preferred. The technique can be used on all types of examinations, and is available for all transducer types.
Where Is NTEQ Technology Useful?
We have found that the use of NTEQ ultrasound technology is extremely helpful in the intensive care unit or neonatal care unit settings. The sonographer no longer needs to be positioned with one hand on the machine for manual image optimization and the other hand with the probe on the patient. With the use of a foot pedal, the sonographer can now move around the patient and obtain optimized images with minimal need to adjust the system. Because the system automatically adjusts gains, the images obtained are uniform and appropriately adjusted for gain, independent of the ambient light in the room. One can adjust the gain settings on the monitor for visualization while performing the exam on the monitor, and the system gains are appropriate for optimized images and final review. In the operating room, one can scan with minimal need to touch the system improving sterility during the exam. During scanning in the operating arena, there is often limited space, so the system can be hooked to an external monitor and placed distant from the operating table with the use of a foot pedal for data storage.
When performing real-time ultrasound-guided image biopsies, the technique allows for rapid continued image optimization during the procedure. As a result, there is no need for an additional sonographer to be adjusting the system while the radiologist, with a needle in one hand and the probe in the other, is performing the biopsy. It is our preference to scan continuously through the area of the biopsy as well as in the transverse plane to the needle entering to confirm adequate placement of the needle in three dimensions. This can be done with NTEQ ultrasound technology with optimization of the images throughout the procedure. Another area where NTEQ ultrasound technology is extremely helpful is what I refer to as "dynamic anatomy." In those situations where anatomy is moving, it is very difficult to manually adjust parameters to optimize an image. The rapid optimization offered by the system allows for significantly improved optimized images during the examination and decreases the amount of lost information because of the inability to optimize an image when the anatomy is in the best window. This is most apparent when doing an OB ultrasound examination (Online video clip 5) . The rapid image optimization allows for captured fetal anatomy when the fetus is in an optimal window without the need for manual adjustments during which time the window could have been lost.
In organs that vary in sonographic properties, the effect is more apparent. In tissue, such as breast, where the sonographic properties can vary greatly from fatty tissue to dense breast tissue over a small area we find the technique allows for decreased scanning time by eliminating the need for continuous gain adjustments (Online video clip 6) .
Does This Mean Everyone Will Be Able To Perform Ultrasound Now?
A major concern of sonographers is that the use of this technique will allow less-trained personnel to perform ultrasound examinations. In fact, I believe these techniques will empower the sonographer to improve the quality of examinations and require their anatomy and pathology training to be more critical. A sonographer can now concentrate on the patient and his/her anatomy and pathology, as opposed to button pushing. A sonographer can now spend his/her time obtaining an optimal acoustical window, positioning patients for the best image, and obtaining more information from ultrasound imaging. Excellent images, while missing pathology, are of no clinical use.
Ergonomics
In addition to providing improved image quality dynamically throughout the examination, this technique should also decrease the repetitive injury associated with ultrasound scanning. The technique significantly decreases the number of key strokes required to perform an examination. Personally, I believe that the technique decreases the amount of back strain when trying to maintain one hand on the console and one hand on the patient. One can maintain a more comfortable position while performing the examination. Our initial impression is that this also decreases the time needed to perform an examination.
New Applications
Because the computer is performing the image optimization, the images are more "standardized" than those created with manual optimization. One would expect a significant decrease in the amount of intra- and interscanner variation in images. To test this hypothesis, we evaluated the intensities of objects in a phantom scanned multiple times using NTEQ technology and the manual technique. The results are tabulated in Table 1. The standard deviations using NTEQ technology are all significantly smaller than when performing manual adjustments. When one compares the uniform areas of the phantom at different depths, the intensities of the near and far field are all more uniform utilizing NTEQ technology.
If we can confirm that the images are more standardized using the NTEQ technology technique in a clinical setting, new opportunities for evaluation or detection of pathology can be envisioned. One can monitor the intensity of a liver over time and pick up more subtle changes, which may occur in such disease states as cirrhosis, hepatitis, and fatty liver infiltration. This may lead to improved confidence of changes occurring or not occurring in lesions during treatment. There is decreased confidence of small changes with the manual technique, as these changes can be contributed to operator dependence. One may also be able to pick up more subtle changes in renal transplants to detect rejection or acute tubular necrosis at an earlier time point. The technique can also be used with ultrasound contrast material for improved quantitation over time to assess treatment response, particularly the evaluation of neovascularity in a tumor.
One can also envision that more subtle lesions may be identified. In manual imaging, one optimizes an image to be recorded while the majority of the scanning is performed without optimization. With more continuous image optimization, less conspicuous lesions may be identified during the scanning portions of the exam.
Conclusions
NTEQ ultrasound technology is a real-time technique that optimizes ultrasound images throughout the course of an examination, and, as a result, improves image quality while significantly reducing the number of buttons that need to be adjusted during an exam. There are certain situations such as in an intensive care unit, operating room, or neonatal intensive care unit, where NTEQ ultrasound technology is extremely helpful in allowing the operator to be positioned away from the machine and allowing for optimized images for storage regardless of the ambient light in the room. If early indications that standardization of images can be obtained are confirmed, the technique may open up new uses for ultrasound in the detection and follow-up of pathology. Further controlled studies are needed to confirm the amount of time savings, image improvement, ergonomics, and improved consistency of images using this technique. This technique moves ultrasound one step closer to being an operator-independent modality.
This publication is sponsored by:
Siemens Medical Solutions USA, Inc.
Ultrasound Division
1230 Shorebird Way
P.O. Box 7393 Mountain View, CA 94039-7393 USA
Siemens Medical Solutions USA
51 Valley Stream Parkway
Malvern, PA 19355-1406
USA Telephone: +1-888-826-9702
www.usa.siemens.com/medical