Parietal Lobe Infarction Secondary to Cortical Venous Thrombosis
Images
Case Summary
A term neonate presented 5 hours postnatally with 6 episodes of focal seizures characterized by right extremity jerking and staring lasting 2-5 minutes. The birth was complicated by gestational hypertension — prompting labor induction — a tight nuchal cord, and placental calcifications. Apgar scores at 5 minutes of life were normal, but some ventilatory support was provided for transient respiratory distress. Physical examination found bulging fontanelles, but laboratory analysis was normal. Toxicology and infectious workups were negative. No family history of hematologic or neurological disorders was noted.
Imaging Findings
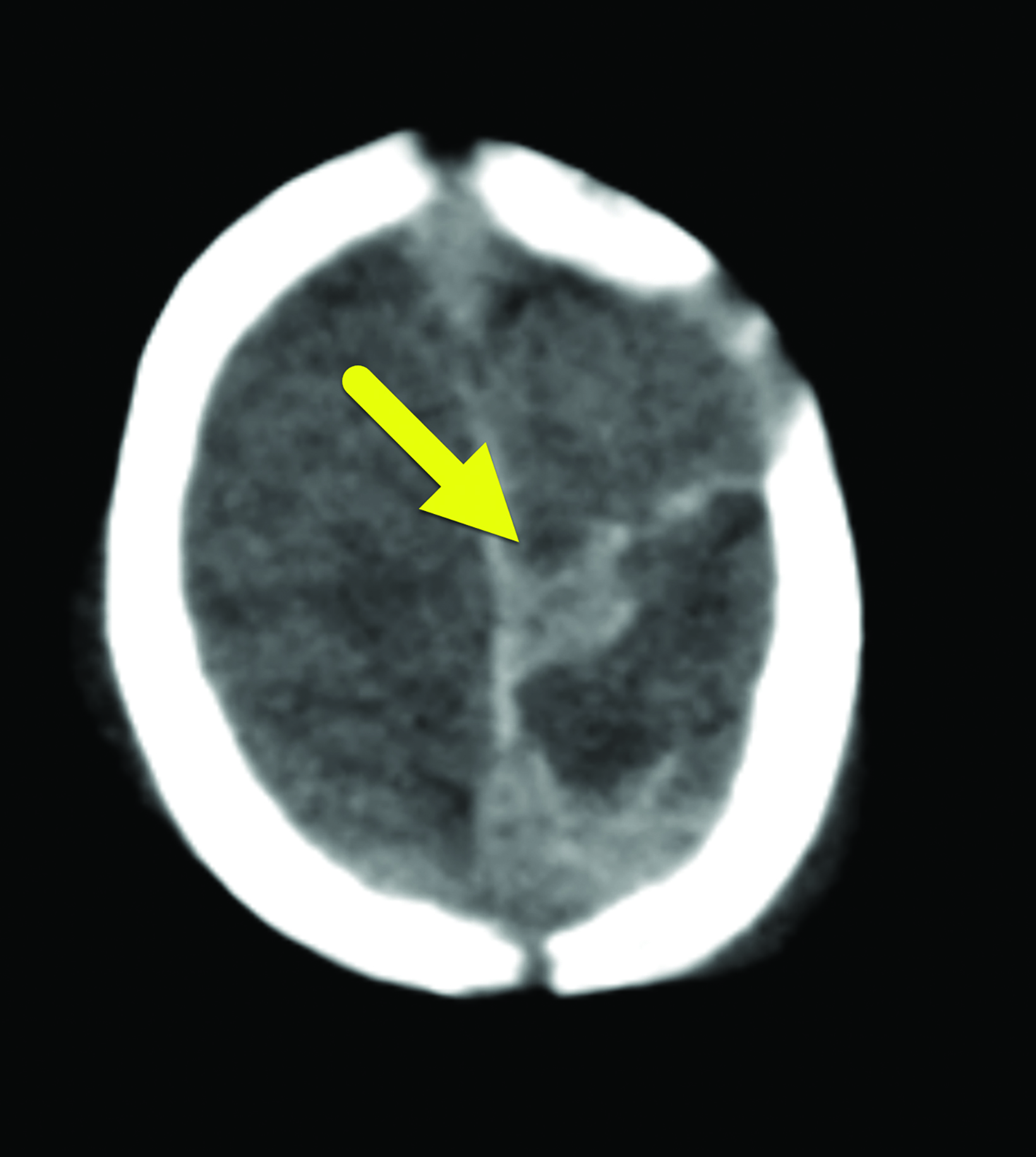
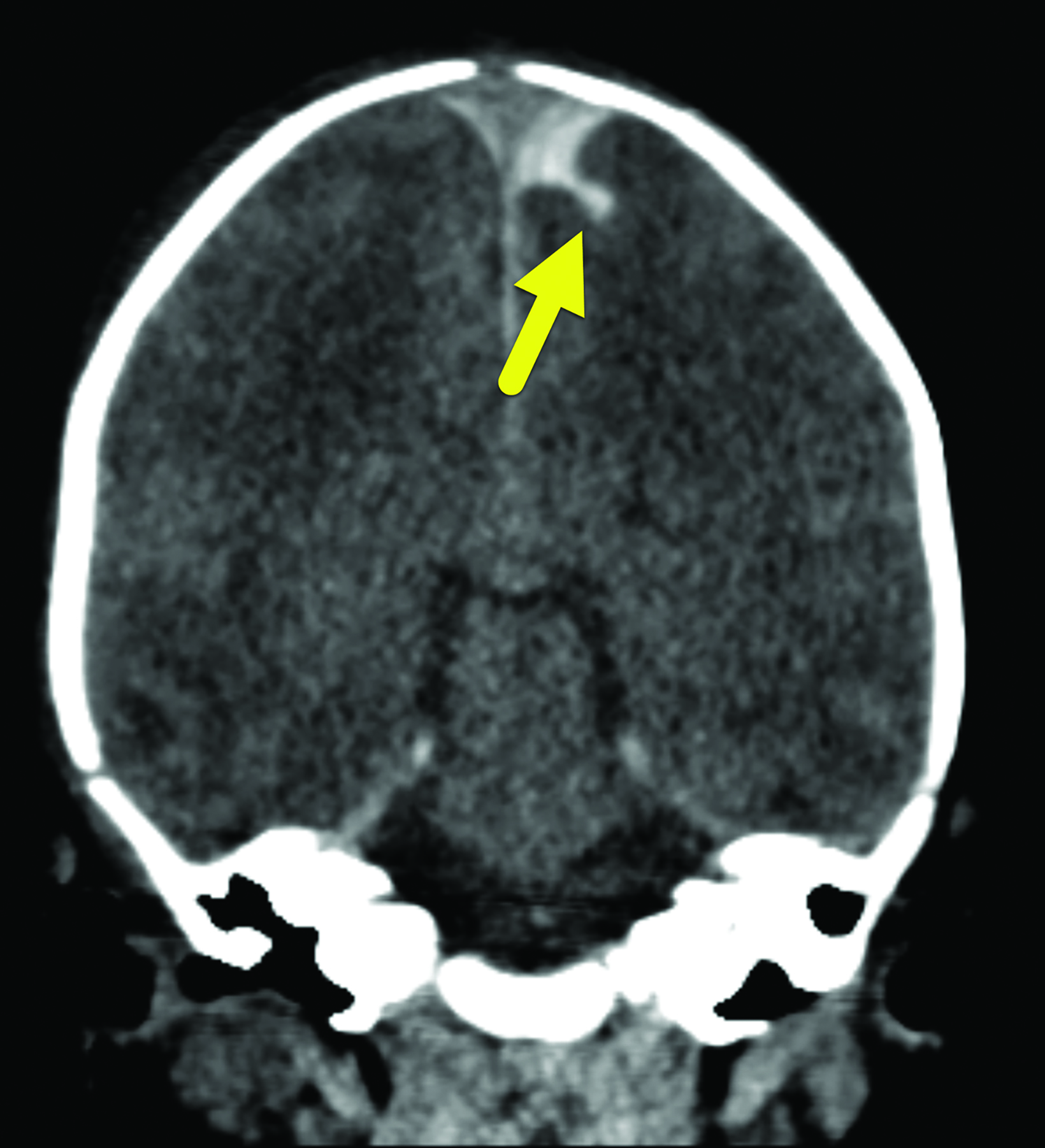
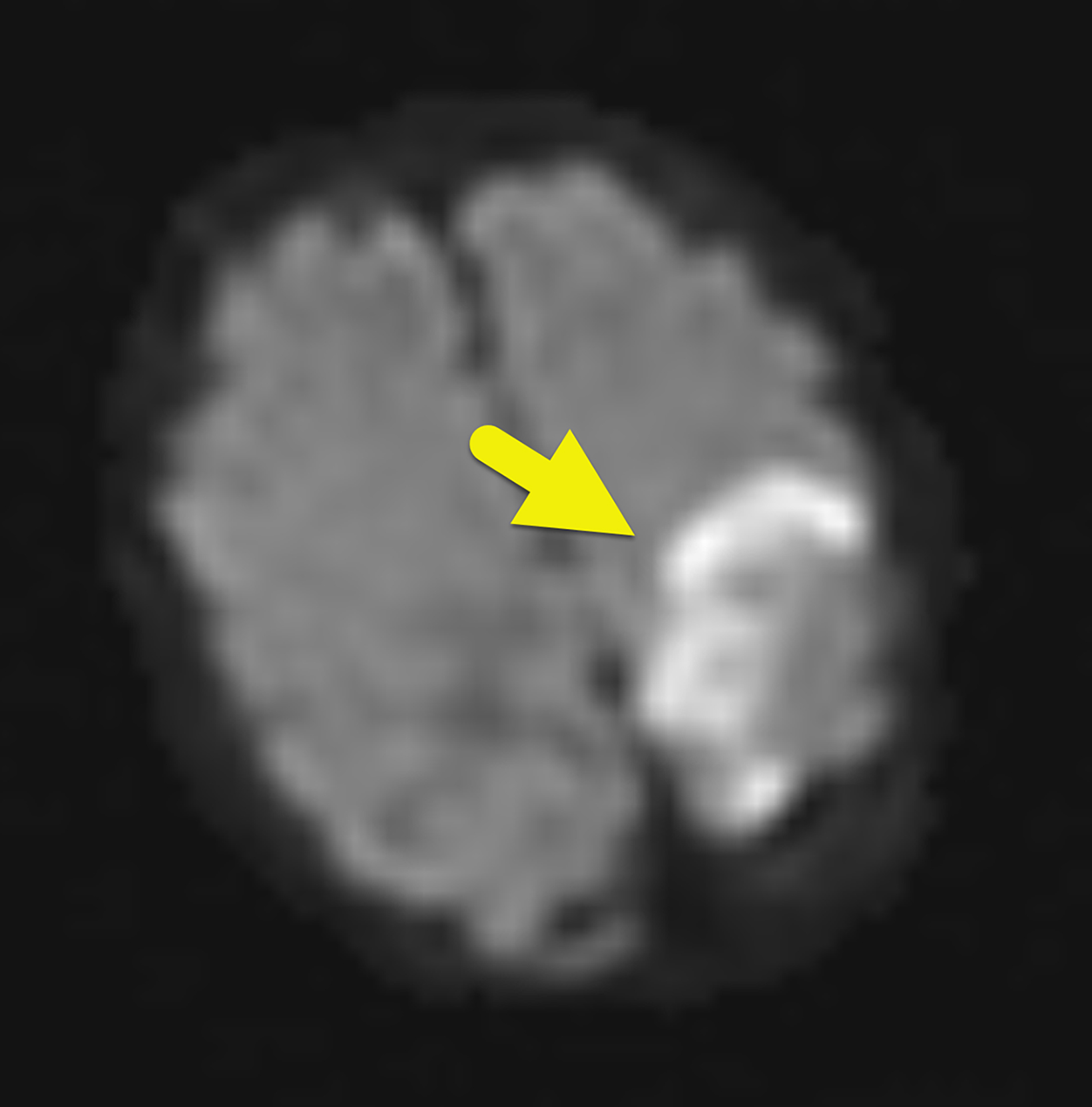
Noncontrast head computed tomography (CT) scan (Figure 1) on the first day of life revealed bilateral extra-axial hemorrhages overlying the parasagittal cerebral hemispheres near the posterior cranial vertex and along the falx cerebrii, layering onto the tentorium. Diffuse scalp edema was noted, but the brain parenchyma, cerebrospinal fluid spaces, and bony structures appeared normal. A CT venogram and head color Doppler ultrasound the same day were normal.
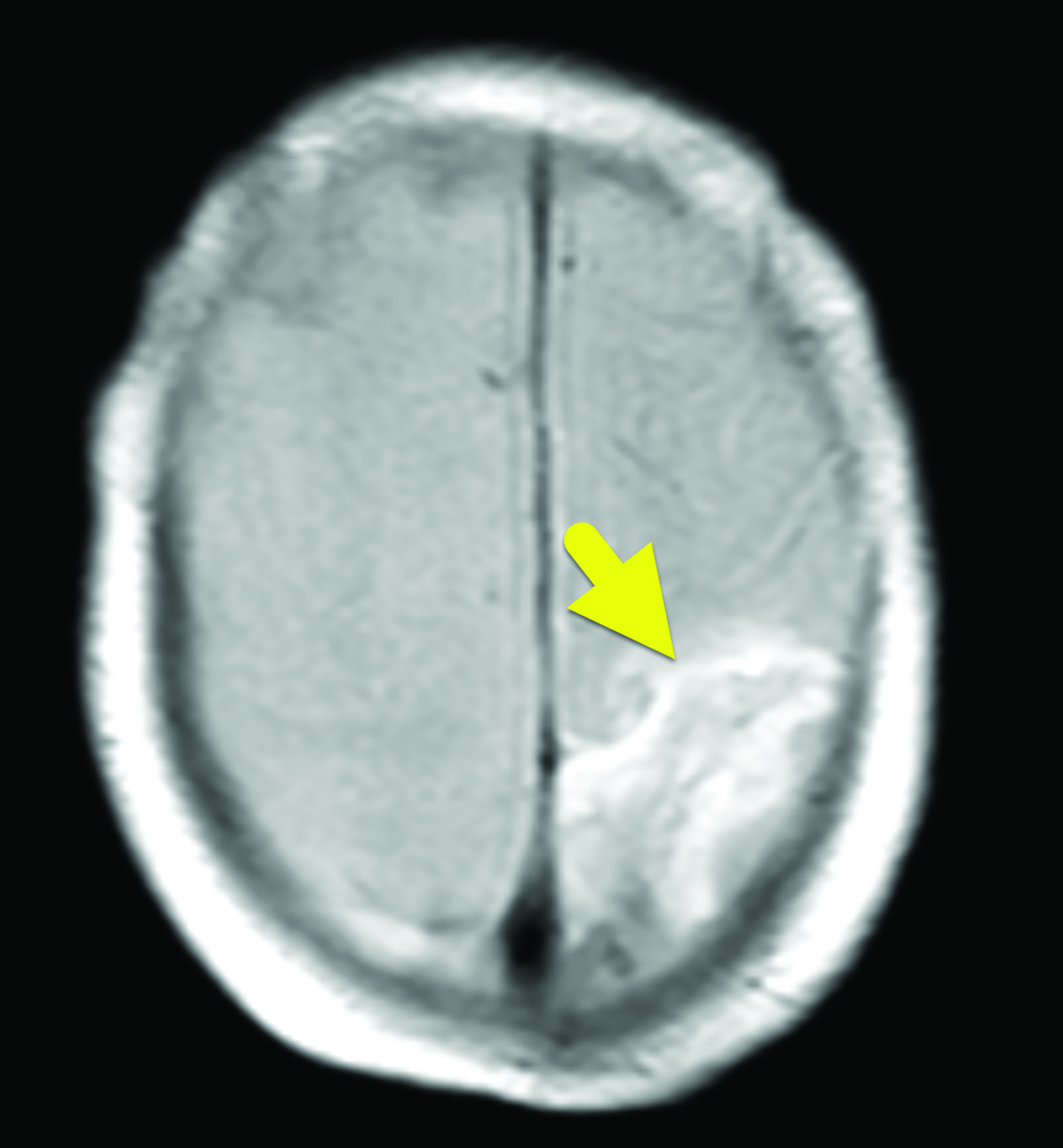
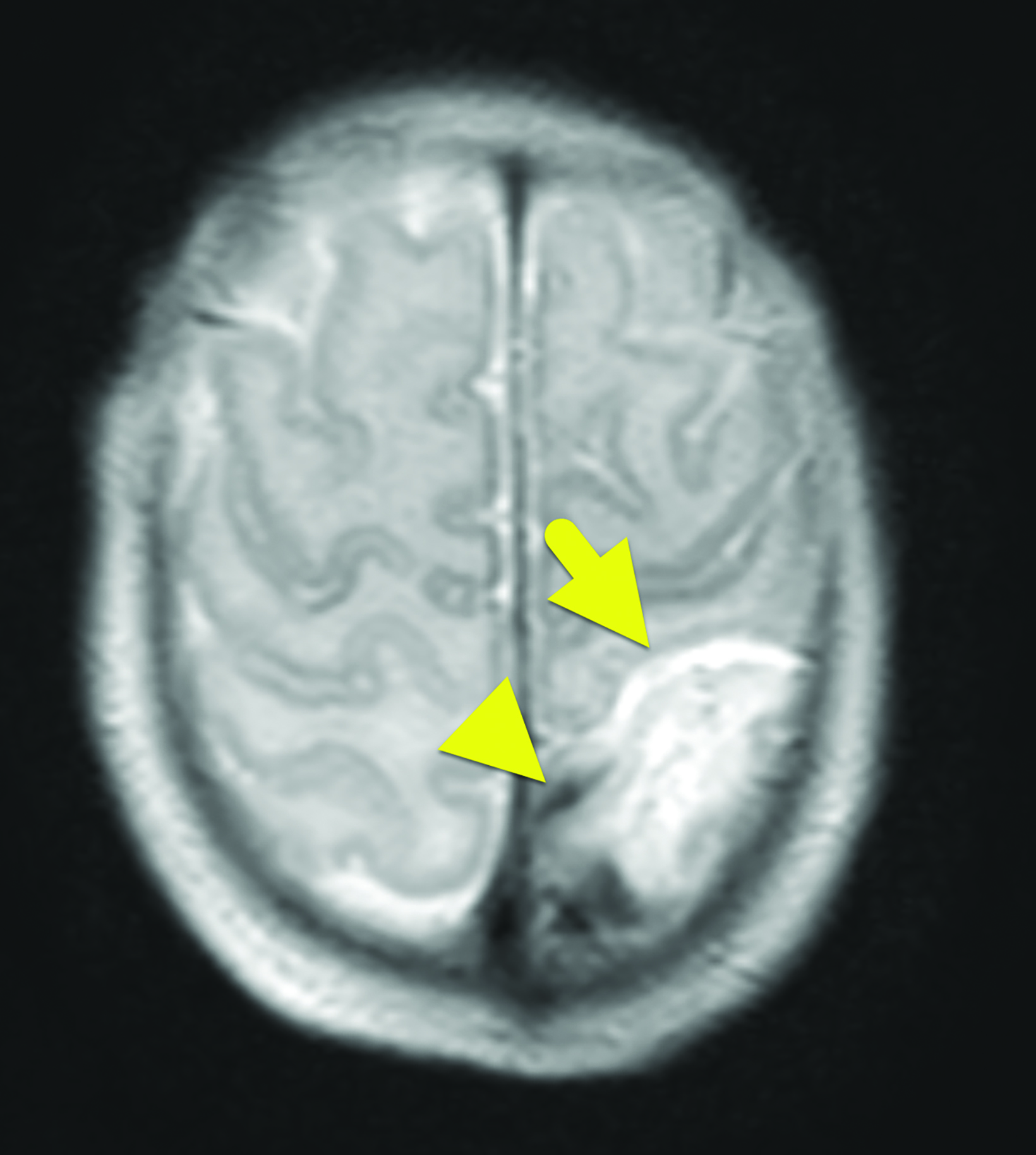
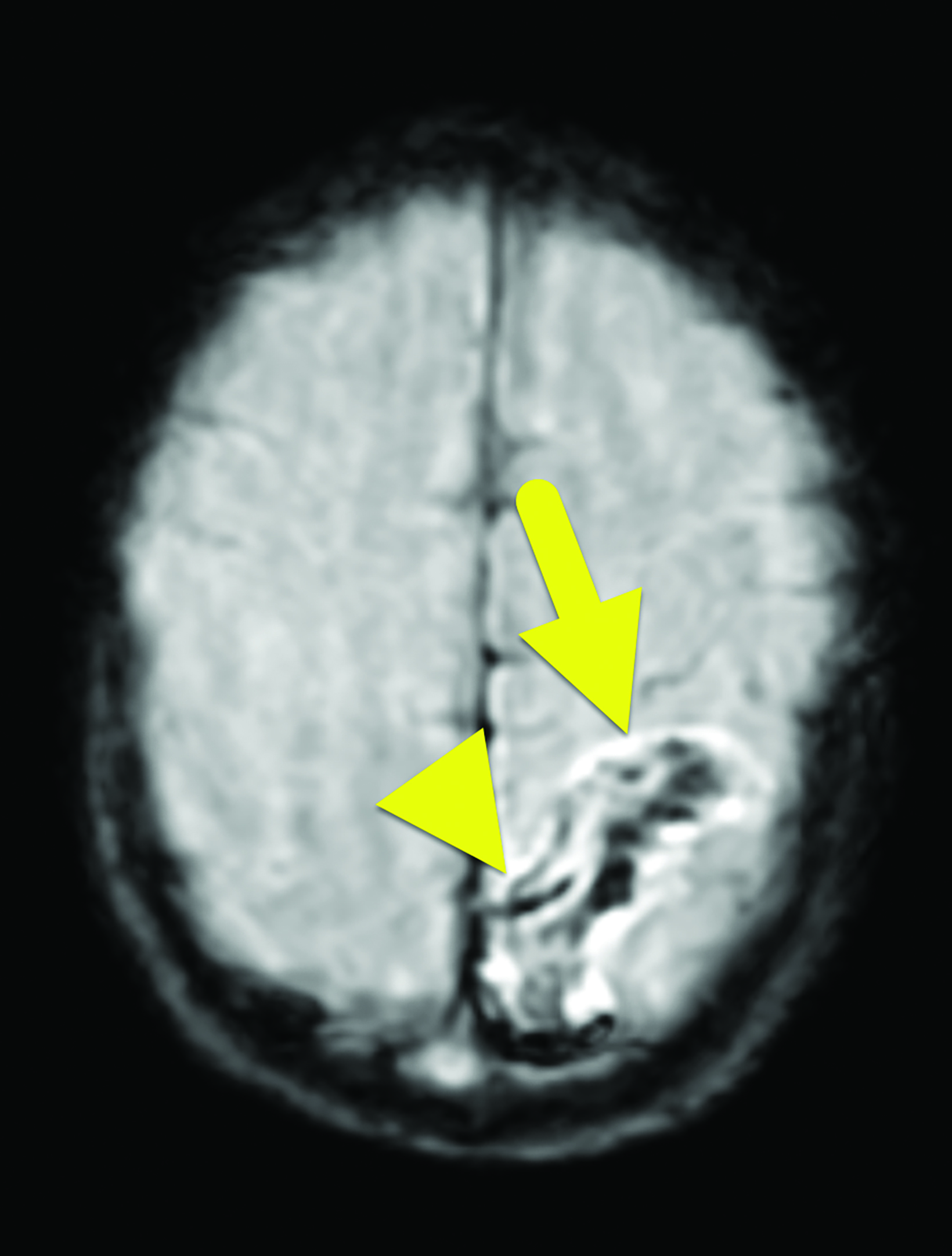
Magnetic resonance imaging (MRI) of the brain (Figure 2) 3 days later showed an area of infarction in the left posterior parietal lobe and extending inferiorly into the left periventricular white matter, with adjacent foci of susceptibility effect suspected to be thrombosed cortical veins. Follow-up gadolinium enhanced imaging revealed an additional nonocclusive thrombus in the right transverse sinus, an improvement in the hemorrhage, and no evidence of further infarction.
Diagnosis
Left parietal lobe infarction secondary to cortical vein thrombosis (CVT) with hemorrhagic transformation. The differential diagnosis includes arterial ischemic stroke and primary hemorrhagic stroke.
Discussion
Brain infarction, or stroke, is uncommon in infants, with an incidence of 0.6 per 100,000 each year. Only 0.5-1% of these cases are caused by CVT.1,2 When a cerebral vein is occluded, retrograde pressure prevents the drainage of local brain capillaries, inhibiting perfusion and causing infarction. The small vessels themselves are also damaged, and intracerebral hemorrhagic transformation follows 50% of CVT strokes.3 The postcapillary perfusion impairment seen in CVT is the opposite of that in arterial ischemic stroke, in which a blood clot blocks precapillary perfusion. As a result, arterial infarcts are confined to a specific area of arterial supply.
This differs from venous infarcts, which can affect any tissue drained by the occluded vein.
Risk factors for ischemic strokes relate to the classic Virchow triad of blood stasis, hypercoagulability, and endothelial injury.1 In neonates, the most common risk factor is an acute systemic illness, such as sepsis, pneumonia, or respiratory distress. Exposure to perinatal stressors like hypoxia and ischemia increase risk. Infants with congenital heart disease are also at increased risk for brain infarction caused by arterial emboli. Placental pathology, often reflected by calcifications, may also lead to inflammatory and prothrombotic states that promote CVT formation in newborns.4
The most common presenting signs of neonatal ischemic stroke are focal motor seizures. Bulging fontanelle, 6th cranial nerve palsy, and focal cortical deficit may also suggest hemorrhage. Up to 25% of CVT strokes are asymptomatic, with the infarct being found incidentally.5 In older children, seizures are much less common and they will instead exhibit a triad of progressive, unremitting headache, altered mental status, and vomiting, especially in patients with venous sinus thrombosis.2
Noncontrast CT of the head is the most frequently performed first-line imaging study in the setting of suspected stroke.6 In the nonemergent setting, CT and CT venography have been proven equivalent to MRI and MR venography for detecting CVT. MRI and MR venography are superior at assessing parenchymal injury and clot burden, respectively .6 Neonatal CVT strokes are increasingly being managed with early anticoagulation therapy, which is associated with better cognitive outcomes and reduced long-term morbidity and mortality.8
CVT stroke treated with anticoagulation undergoes clot propagation only 4% of the time, compared to 28% of the time in untreated cases.7 While concerning, hemorrhage is not an absolute contraindication to anticoagulation, and the risks and benefits should be weighed on an individualized basis.3
Thrombolysis and thrombectomy are controversial in children, but they may be considered in critically ill patients who do not improve with anticoagulation alone.2
The prognosis of neonatal arterial strokes varies and depends on the size of the infarct. One large study found that 68% of patients developed cerebral palsy, 59% had residual cognitive or speech impairments, and 47% had epilepsy.7 Less data exists for CVT stroke prognosis, but one multicenter study found that 50% of treated patients were asymptomatic at follow-up, while 25% had residual neurological deficits.8
Conclusion
Cortical vein thrombosis is a rare cause of stroke in children. Favorable prognosis relies on early detection, imaging, and treatment.
References
- Avni FE, Garel C, Cassart M, et al. Imaging and classification of congenital cystic renal diseases. Am J Roentgenol. 2012;198: 1004-1013. doi: 10.2214/AJR.11.8083.
- Moyle PL, Kataoka MY, Nakai A, Takahata A, Reinhold C, Sala E. Nonovarian cystic lesions of the pelvis. Radiographics. 2010;30(4):921-938. doi:10.1148/rg.304095706.
- Aslam M and Watson AR. Unilateral multicystic dysplastic kidney: long term outcomes. Arch Dis Child. 2006: 91(10):820-823. doi: 10.1136/adc.2006.095786.
- Coley BD, editor-in-chief. Section 7: Genitourinary system. In: Caffey’s Pediatric Diagnostic Imaging, 13th edition. Philadelphia, PA: Elsevier. 2019: 1065-1218.
- Blumer SL, Biko DM, Halabi SS. Pediatric Genitourinary Tract. In: Pediatric Imaging: A Core Review. Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo. Wolters Kluwer; 2019. 45-82.
- Towbin R, Martin L. Multilocular cystic dysplasia of half of a horseshoe kidney. J Pediatr Surg. 1974;9(3):421. doi:10.1016/s0022-3468(74)80308-8.
- Alam K, Varshney M, Aziz M, et al. Multicystic Renal Dysplasia. Brit Med J Case Rep. 2011. doi: 10.1136/bcr.03.2011.3989.fic Statement From the American Heart As- sociation/American Stroke Association. Stroke. 2019;50(3). doi:10.1161/STR.0000000000000183
- Sebire G. Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain. 2005;128(3):477-489. doi:10.1093/brain/awh412
Citation
JT H, RB T, CM S, AJ T.Parietal Lobe Infarction Secondary to Cortical Venous Thrombosis. Supplement to Applied Radiology. 2022; (6):9-11.
November 2, 2022