Pancreatitis associated with splenic artery pseudoaneurysms
Images




Summary
A 46-year-old man presented with a 5-month history of abdominal pain that had become aggravated in the previous half month. The patient’s temperature was 37.2°C, his pulse was 80/min, respiration 21/min, and blood pressure 13/8KPa. The patient was well developed and moderately nourished, with no evidence of heart or chest abnormalities. There was a scar located in the upper center of the patient’s abdomen. The patient was positive for left abdomen tenderness, negative for rebound tenderness. The patient was negative for liver and renal region knock pain and shifting dullness.
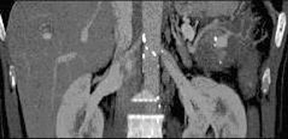
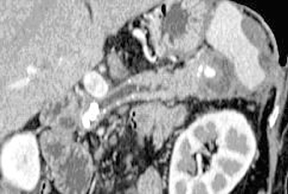
Scanning was performed with a 64-detector row computed tomography (CT) scanner and postprocessing workstation using a dual-phase protocol. The scanning parameters were as follows: 0.75-mm collimation, 1 pitch, 0.5-mm reconstruction interval, 120 Kv, 120 mAs. The dual-phase spiral CT protocol, arterial and venous phases,was performed. 100 ml of Iohexol(30g I/100ml) was intravenously injected with a flow rate of 3 ml/s before examination. Using the workstation, volume rendering (VR), maximum intensity projection (MIP), cure plane reconstruction (CPR), and inspace images were acquired.
Diagnosis
Pancreatitis associated with pseudocyst and splenic artery pseudoaneurysms
Findings
Pancreas volume was slightly reduced; there were a few stones in the main duct, which was obviously dilated. The largest stone, measuring 1.0 cm × 1.0 cm, was found in the head of the pancreas. A round heterogeneous lesion measuring 3.2 cm × 3.5 cm was located behind of the tail of the pancreas. On arterial and venous phase images, the center of the lesion showed distinct enhancement that was isoattenuating to the splenic artery. Punctal calcification was found at the lateral wall of the lesion. The periphery of the lesion did not enhance. VR and inspace images clearly displayed the relationship of the lesion to vascular and peripheral tissues.
Discussion
Pseudoaneurysm is a rare complication of pancreatitis; it has been reported to occur in 3.5% to 10% of pancreatitis cases. Although ruptures of pseudoaneurysms are relatively rare, the mortality rate from pseudoaneurysms has been reported to be as high as 50%.1,2 Therefore, accurate and timely diagnosis of pseudoaneurysm is very important.
Pseudoaneurysm is associated with pancreatic enzymes eroding peripancreatic vessels to cross tissue planes and boundaries. The arteries involved include, in order of frequency: the splenic, gastroduodenal, pancreaticoduodenal, gastric, and hepatic arteries.3 The splenic artery was involved in this case. Though ruptures of pseudoaneurysms are relatively rare, sufficient knowledge of this catastrophic complication is necessary to make a timely diagnosis and begin treatment to reduce the mortality. It has been reported that large peripancreatic pseudoaneurysms can be displayed by dynamic CT scan or color Doppler sonography, but small pseudoaneurysms can be displayed only by angiography.4 Plain CT cannot distinguish pseudoaneurysm from pseudocyst, while enhanced multisliced CT (MSCT) can show the shape and location of pseudoaneurysms straightforwardly, wholly and satisfactorily.
In our case, MSCT showed the location and extension of the lesion and its relationship to associated blood vessels. Postsurgical pathology revealed fiber tissue and hemorrhage in the cyst.
Pseudoaneurysm should be distinguished from pseudocyst and pancreatic masses. With regard to pseudocysts, plain CT scans frequently fail to diagnose pseudoaneurysm, but enhanced CT shows that no blood vessel supplies the pseudocyst. In our case, the pseudoaneurysm was located in pseudocyst.
With regard to pancreatic masses, on arterial phase images, a pseudoaneurysm is similar to insulin that is significantly enhanced and can be confused with a pancreatic mass.
Conclusion
If proper scan protocol and MSCT 3-dimensional angiography are applied, MSCT will be a suitable technique that combines diagnostic accuracy and minimum invasiveness in demonstrating the presence of pseudoaneurysm.
References
- MacMahon MJ. Acute pancreatitis. In: Misiewicz JJ, Pounder RE, Venables CW, eds. Diseases of the gut and pancreas. London: Blackwell Scientific Publications, 1994:3427-3440.
- Lendrum R. Chronic pancreatitis. In: Misiewicz JJ, Pounder RE, Venables CW, eds. Diseases of the gut and pancreas. London: Blackwell Scientific Publications, 1994:441-454.
- Ishida H, Konno K, Komatsuda T, et al. Gastrointestinal bleeding due to ruptured pseudoaneurysm in patients with pancreatitis. Abdom Imaging (United States). 1999;24:418-421.
- Wang ZK, Li P, Gou WM, et al. Superior mesenteric artery pseudoaneurysm complications of pancreatitis (case report) (Chin). J Clin Radiol. 2003;22:859.
Citation
Pancreatitis associated with splenic artery pseudoaneurysms. Appl Radiol.
February 1, 2013