Nuclear Medicine Takes on the Challenge to Manage Dose and Image Quality
Images

The campaign to lower radiation dose across imaging procedures is not limited to radiology, but is gaining momentum in the field of nuclear medicine.
Over the last decade, the medical imaging community has been driving home the message to lower radiation dose levels as low as reasonably achievable (ALARA), but much of the focus has primarily been on patient radiation dose reduction in x-ray procedures, predominantly in computed tomography (CT). This is despite the fact that a number of nuclear medicine examinations deliver patient effective dose in the range of 5 to 20 mSv per study, which is similar to that in CT.1 Additionally, the adoption of hybrid imaging modalities, in particular positron emission tomography with CT (PET/CT) and single photon emission computed tomography with CT (SPECT/CT), has proliferated, further increasing the levels of dose exposure to patients.
The focus on radiation dose management in nuclear imaging came to a head in the last two years when the Society of Nuclear Medicine (SNM) and the Society for Pediatric Radiology’s Board of Directors were compelled to establish new North American Guidelines for Radiopharmaceutical Doses for Children. These societies expanded their pediatric radiation protection initiative by standardizing doses (based on body weight) for [more than 11] nuclear medicine procedures commonly performed in children.2
“It is important that we standardize dose to help ensure that all pediatric nuclear medicine professionals consistently optimize medical images while only using the minimum amount of radiation necessary to obtain these images,”2 said S. Ted Treves, MD, Strategy Leader of the Image Gently™ Nuclear Medicine Initiative, Chief of Nuclear Medicine and Molecular Imaging at Children’s Hospital Boston and Professor of Radiology at Harvard Medical School, Boston, MA.
While the catalyst for change emerged out of a need to limit radiation exposure to children, it applies to patients across the board, and nuclear medicine has become equally committed as radiology to the cause of lowering radiation dose in imaging procedures.
More CT Enhances NM Exams
Similar to CT, lowering dose in nuclear medicine may compromise image quality, which can adversely affect diagnostic accuracy. However, with developments in dose reducing solutions, doctors may no longer have to trade-off image quality for lower patient dose.
A significant advancement in nuclear medicine has come with the development of hybrid systems. When performing a SPECT/CT exam, coregistration is much more straightforward when SPECT and CT are combined in a single scanner because the patient remains in the same position during the acquisition of both sets of images.3 This is especially valuable during oncology studies and in bone imaging.
However, conducting lesion localization with the low-diagnostic quality attenuation correction CT images from most hybrids is very challenging. As Johnsey Leef, MD, Chief of Radiology, CT and Nuclear Medicine, Charleston Area Medical Center (CMAC), Charleston, WV, indicated, “CT was originally just for mapping, and it was a really low-dose CT with poor quality CT. This is something we would like to improve.”
While the nuclear medicine community calls for improved quality in CT imaging, it wants to avoid raising radiation levels.
“One of the advantages with PET/CT is that it begins to carve into the volume of CT that has to be done in oncology. So, for example, the initial staging in lymphoma certainly needs diagnostic CT, and we almost always do a PET/CT. Many of these patients can be followed and scored on criteria with the combination of PET and the low-dose CT to look at changes in response to therapy. Therefore, some of the radiation dose to an individual patient can be decreased. That’s a benefit,” said James K. O’Donnell, MD, Associate Professor of Radiology, Case Western Reserve University (CWRU), Director, Division of Nuclear Medicine and PET. The challenge, however, has been acquiring quality images with low-dose CT.
This dilemma has prompted the development of solutions like the Ingenuity TF PET/CT system by Philips Healthcare. Like CT, the Ingenuity TF PET/CT system is equipped with the Ingenuity CT platform and iDose4. In addition, PET sensitivity and accuracy is enabled with Astonish TF time-of-flight technology providing greater accuracy of SUV values via list-mode reconstruction without compromising performance.
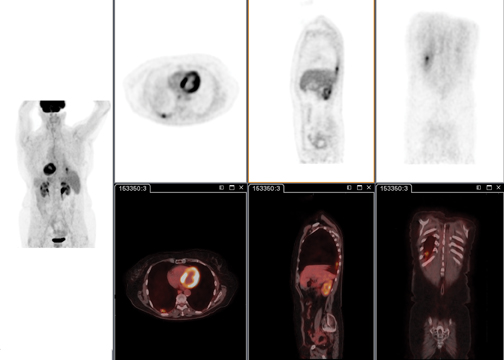
Enhanced image quality is possible thanks to Astonish TF, the latest generation in Time-of-Flight (TOF) technology, which leads to enhanced contrast by up to 30% compared to non-TOF images. With up to 5 times higher sensitivity than non-TOF scanners, you may be able to reduce radiopharmaceutical dosing in some or all of your studies (Figure 1). Also, Astonish TF technology allows Philips to select the best-in-class list-mode reconstruction algorithm without compromising reconstruction speed.
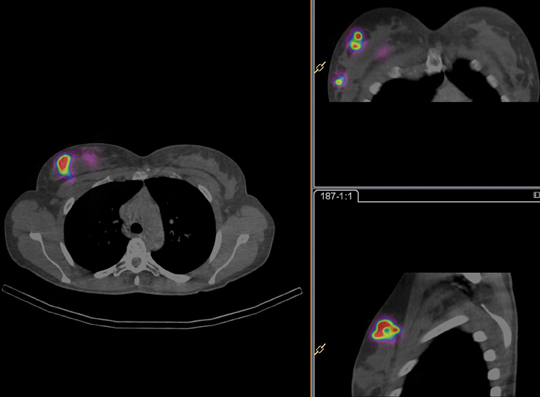
Similar to PET, the focus for SPECT is heavily weighted on correlating and fusing images from CT with the SPECT images. This can be achieved with the co-planar design of the BrightView XCT that allows the CT and SPECT images to be acquired with little or no table motion between the two studies. The flat-panel cone-beam CT (CBCT) component uses low dose scans for localization purposes. And since both the SPECT and CT acquisitions are planned from the nuclear medicine p-scope, there is no additional dose for scout or topogram imaging that conventional CT scanners use.
The BrightView XCT has full iterative technology (FIT), which uniquely supports iterative reconstruction on both the SPECT and CT (Figure 2). On the SPECT side, the Astonish technology, which incorporates resolution recovery into the iterative reconstruction process, provides improved spatial resolution. On the CT side, iterative reconstruction is used to improve image quality through increased uniformity and reduced noise.4
“We have the BrightView XCT SPECT/CT, which uses the flat panel. It has the full iterative reconstruction of CT data. That aids us a lot on just routine SPECT, bone, MIBG studies, parathyroid studies, and all the different kinds of studies you want to use the data for,” said George M. Ebert, MD, PhD, Associate Professor of Radiology, Chief, Informatics and Imaging Technology, Co-Director of Clinical MRI, University of Vermont College of Medicine, Burlington, VT, in affiliation with Fletcher Allen Healthcare.
Dose management: A balancing act
Effective management of oncological diseases requires repeated PET/CT or SPECT/CT imaging for diagnosis, staging, and monitoring. This adds up to multiple exposures to radiation throughout the therapy, and a need for dose management solutions.
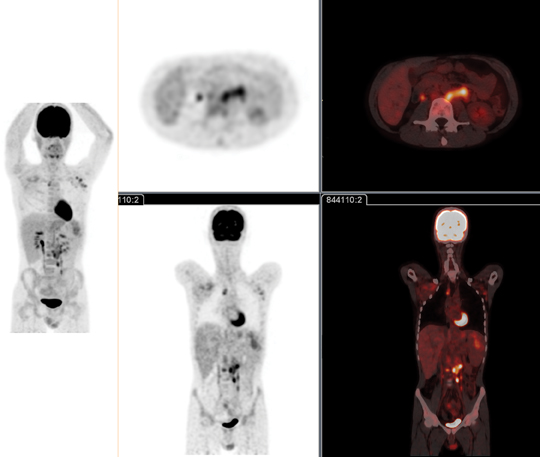
On the PET side, the advancements in the Ingenuity TF PET/CT System are driven by Astonish TF, which enhances lesion detectability with acquisition time that can be as fast as 30 sec/bed. Dr. Ebert noted how much faster the upgraded Astonish TF completes image reconstruction than the previous version (Figure 3).
“I can, in many cases, see lesions in the lung that are 4 mm and 3 mm—something that we never expected to see in PET,” said Dr. Ebert. “We used to have a threshold of approximately 8 mm in PET in the old days. So we’re seeing smaller lesions.”
A recent NIH study5 found that TOF improves lung and liver lesion detection in patients. This is especially true in heavy patients.
“One of our problems is that patients are getting heavier. Traditionally the only way to compensate for that has been [to] increase radiation dose to maintain image quality,” said Dr. Ebert. “Using Astonish TF, we can take a large patient and get spectacular image quality. The time penalty that we used to incur to do the Time of Flight is completely gone. So now we can use Time of Flight on every single case, for all applications, whether they’re cardiac or oncology. That alone has improved our stance a lot.”
“Setting appropriate levels to either reconstruction so that you’re able to achieve diagnostic quality images has also been a factor in SPECT/ CT,” noted Dr. O’Donnell, who works with the BrightView XCT. This system is uniquely outfitted with both iterative SPECT and CT reconstruction capabilities. “We have the flat-panel detectors with the attenuation correction and the iterative reconstruction that’s gone into SPECT,” said Dr. O’Donnell.
This is important because as Dr. O’Donnell pointed out, “Dose does add up after a while, when you’re doing repetitive studies, for example, with a regular follow-up with Indium octreotide scans and SPECT or a regular follow-up with FDG scans in oncology.”
List mode supports advanced imaging
Advanced techniques in PET imaging, such as improvements in standard uptake value (SUV) accuracy, are leveraging the TOF for fast scan times.
“When you do time-of-flight, you basically are counting every single photon, its direction, and how long it took to get from one side to hit the ring,” explained Dr. Ebert.
The list mode feature helps Dr. O’Donnell and his clinical team to perform advanced imaging studies and the latest techniques in oncology.
“We’re doing quantitative blood flow, and you need list mode for that because you have to capture that initial arterial input into the blood. Because it happens so fast, you can try framing rates, but it’s much better to have the list mode, where the computer’s concentrating on just gathering all,” said Dr. O’Donnell.
“For cardiac and oncology imaging, if you want to post-process this into some sort of data study program—either respiratory data or cardiac data—it is one of the big advantages of list mode,” noted Dr. Ebert.
Stress-only imaging to reduce dose
Another technique for reducing dose that can benefit patients and clinicians is stress-only imaging. A method used for myocardial perfusion that can be applied in SPECT/CT imaging studies, stress-only imaging demonstrates that perfusion and gated imaging can be performed on half-count data with high diagnostic accuracy and acceptable image quality.
In a recent multi-center trial designed to test performance of the Astonish algorithm for myocardial perfusion SPECT imaging, researchers compared the clinical performance of Astonish on both full-count and half-count stress-rest data, both with and without attenuation and scatter corrections.6
The study showed that absorbed radiation doses can be reduced by injecting less activity while imaging for conventional imaging times.7 Results from stress-only imaging, which requires the use of attenuation correction, demonstrate that perfusion and gated imaging can be performed on half-count data with diagnostic accuracy, acceptable image quality, diagnostic confidence, similar defect extent and severity to full-time acquisitions, and a low perceived need for rest imaging. Performing studies using stress-only may increase patient acceptance, further reduces radiation doses (compared to stress/rest half dose imaging).6
According to Dr. Ebert, “The positive rate in stress-only imaging is 10% or 11%. So that means 90% of the time that we get these scans, the stress-only portion is normal, and you can argue that the rest of the portion was unnecessary. I think there’s a future in stress-only imaging.”
The advantage of stress imaging, as Dr. O’Donnell points out, is “you can save the radiation dose.” “When [patients] have the test, if it looks normal in the stress images, you can save the radiation dose and the time,” he explained.
According to Dr. Ebert’s assessment, “The new iterative reconstruction techniques, such as FIT, have made improvements; together they have all really helped us maintain the lowest dose that we can possibly get and still maintain image quality.”
References
- Radiation dose optimization in nuclear medicine. Radiation Protection of Patients. https://rpop.iaea.org/RPOP/RPoP/Content/News/radiation-dose-optimization-nuclear-medicine. htm. Accessed October 14, 2011.
- Image gently, SNM launch initiative to standardize radiation dose in pediatric nuclear medicine. American College of Radiology. http://www.acr.org/SecondaryMainMenuCategories/NewsPublications/FeaturedCategories/CurrentHealthCareNews/IG-SNM-Standardize-NM-Dose.aspx. Accessed October 14, 2011.
- Miller JC. Hybrid SPECT/CT: Enhancing Nuclear Medicine. Radiology Rounds. http://www.mghradrounds.org/index.php?src=gendocs&ref=2010_july. Accessed November 7, 2011.
- Hansis E, Da Silva A, Hines H. BrightView XCT – flat-panel cone-beam CT with iterative reconstruction for localization and attenuation correction. Whitepaper. Koninklijke Philips Electronics N.V. 2011.
- Johnston J, Killion J, Veale B, Comello R. U.S. Technologists’ Radiation Exposure Perceptions and Practices. Radiol Technol. 2011;82:311-320.
- Heller GV, Bateman TM, Cullom SJ, Hines HH. Improved clinical performance of myocardial perfusion SPECT imaging using Astonish iterative reconstruction. Netforum community. Astonish reconstruction. Philips. http://clinical.netforum.healthcare.philips.com/us_en/Explore/White-Papers/SpectCT/Improved-clinical-performance-of-myocardial-perfusion-SPECT-imaging-using-Astonish-iterative-reconstruction. Accessed October 7, 2011.
- Borras C. Radiation Protection in Diagnostic Radiology. Radiological Physics and Health Services Consultant. Washington, DC.