Neuropathic Shoulder Joint with Syringomyelia
Case Summary
A previously healthy adult presented with a 6- to 12-month history of progressively worsening pain and loss of range of motion in the right shoulder. The patient reported radiation of pain into the right hand and noticed bruising of the right upper arm. There was no reported trauma, prior surgical intervention, recent illness, fever, night sweats, or worsening pain at night. Laboratory values were within normal limits without leukocytosis or other inflammatory markers.
Imaging Findings
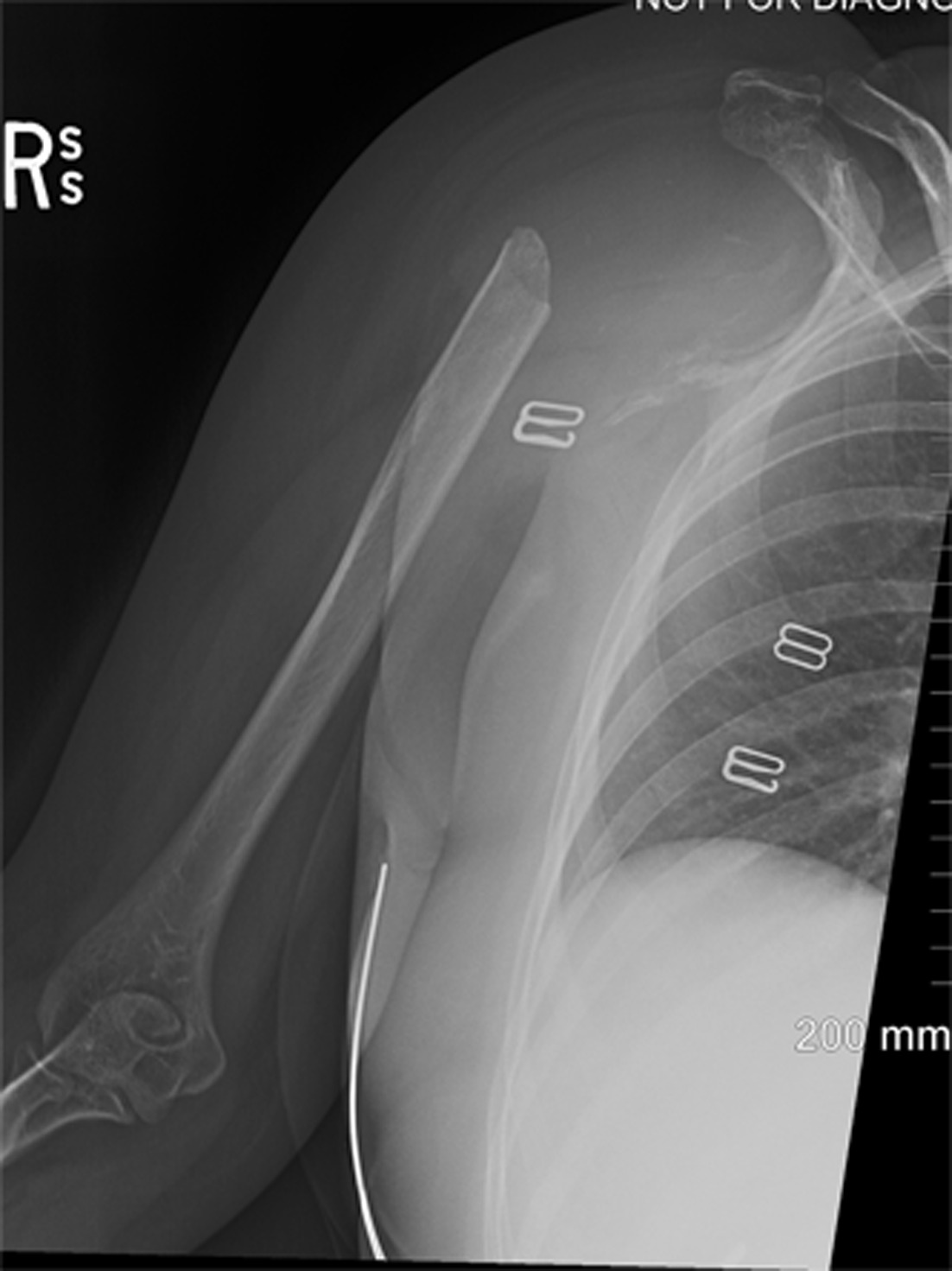
Right shoulder radiographs showed massive osteolysis of the humeral head and glenoid, without significant new bone production ( Figure 1 ). A US of the right upper extremity was also performed to evaluate for deep venous thrombosis. Vascular structures were normal, but the US demonstrated a large, complex joint effusion and synovitis in the shoulder.
The initial anteroposterior radiograph of the right humerus in internal rotation demonstrates severe osteolysis of the proximal right humeral head, neck, and glenoid. A few calcified foci are noted in the expected region of the right humeral head.
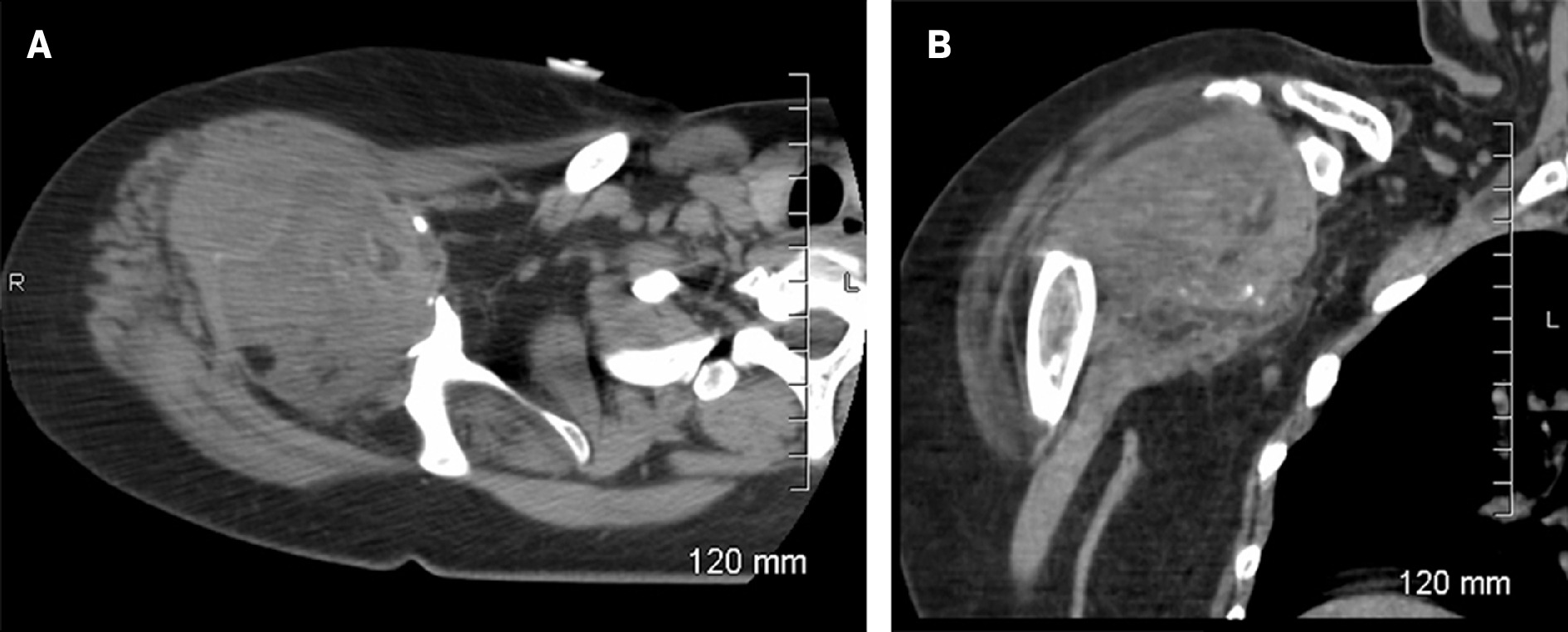
An MRI of the right shoulder confirmed the extensive osteolysis of the proximal humerus and the glenoid, a large glenohumeral joint effusion, and significant synovial proliferation ( Figure 2 ). Additional MRI of the cervical and thoracic spine was recommended to evaluate for syringomyelia; this revealed syringomyelia extending from the C2 through T8 levels. Low-lying cerebellar tonsils were also noted, consistent with a Chiari I deformity ( Figure 3 ). A follow-up CT of the right shoulder was performed, which again demonstrated massive osteolysis of the right proximal humerus and glenoid with large joint effusion ( Figure 4 ). A skeletal survey showed no other osteolytic lesions.
Axial proton density fat-suppressed sequence demonstrates extensive osteolysis of the proximal humerus. Additionally, there is a large shoulder joint effusion with associated severe synovial proliferation.

MRI of sagittal T2-weighted imaging of the cervical and upper thoracic spine demonstrates Chiari I deformity with caudal descent of the cerebellar tonsils to the level of the posterior arch of C1. There is an associated syrinx (inferior extent not included).

Axial (A) and coronal reformation (B) nonenhanced CT imaging demonstrates massive osteolysis of the right proximal humerus and glenoid with scattered intra-articular bony fragments. There is also a large glenohumeral joint effusion with severe mass-like synovial thickening.
Diagnosis
Neuropathic joint (Charcot joint) with associated syringomyelia.
The differential diagnosis of massive osteolysis of the shoulder joint includes Gorham-Stout disease, Milwaukee shoulder, and infectious processes, including septic joint/osteomyelitis. Neuropathic joints can result from various etiologies, including diabetes mellitus, syringomyelia, neurosyphilis/tabes dorsalis, traumatic spinal cord injury, alcoholism, or tumors compressing/involving the spinal cord or peripheral nerves.
Discussion
Shoulder pain and limited range of motion are common general complaints, often related to trauma, arthritis, and subacromial impingement. Patients presenting with similar symptoms secondary to massive osteolysis are much rarer; to our knowledge, only a few have been reported in the literature. The clinical presentation of this case, along with normal inflammatory laboratory values and lack of leukocytosis, was not consistent with an infectious process or other inflammatory causes. The patient did not have diabetes mellitus.
Gorham-Stout disease, commonly known as “vanishing bone disease,” is a rare vascular disorder characterized by progressive osteolysis. It is a multisystem, developmental disorder of lymphangiogenesis that also affects bone, with slow endothelial cell turnover and associated cutaneous lymphatic malformations. Gorham-Stout, which predominately affects males, is typically diagnosed based on imaging findings and biopsy. The mean age of presentation is 12.8 years. It is polyostotic, typically involving the ribs, cranium, clavicles, and cervical vertebrae.1 A treatment approach involving oral medications to suppress the immune system, and medications such as interferon alpha-2b, and rapamycin to target lymphatic vessel formation, has been found to inhibit disease progression, symptoms, and complications. Surgical intervention may be necessary to stabilize or remove affected bones as well as treat symptoms of the disease.1
In this case, the subsequent diagnosis of a Chiari I deformity and large syrinx clinched the diagnosis of neuropathic joint with massive osteolysis. The presentation of a neuropathic joint may include severe and rapid joint destruction, effusion, limited range of motion, and instability. Typically, the joints are painless and lack significant neurological deficits.
Physical examination may demonstrate abnormalities in proprioception and decreased or blunted deep-pain sensation.2 - 4 Imaging findings include generally normal bone density, large joint effusion, and severe, massive, bony destruction without new bone formation. Cross-sectional imaging supports the diagnosis and assessment of the extent as well as underlying causes. Common etiologies for neuropathic joints include diabetes mellitus, syrinogomyelia, tabes dorsalis, alcoholism, and spinal cord injury.2
According to the literature, when the shoulder is involved, it is typically secondary to syringomyelia and Chiari I deformity.3, 5 The exact etiology of osteolysis is unclear but may be related to alteration in blood flow, leading to osseous hyperemia and increased bone resorption.3 MRI of the entire spinal cord is the preferred modality to assess the size and extent of the syrinx. The craniocervical junction should be evaluated for caudal descent of the cerebellar tonsils greater than 5 mm below the foramen magnum and narrowing of the cerebrospinal fluid spaces to indicate Chiari I deformity. In our case, the diagnosis was supported by the MRI findings ( Figure 3 ).6
Treatment of the affected joint can vary from conservative management to steroid injections, proper joint splinting, and physical therapy. Other treatment options include arthrodesis and joint reconstruction.7 Treatment of the underlying etiology is important.
Conclusion
Massive joint osteolysis is rare. Laboratory studies and imaging can assess for underlying etiologies and define the extent of the abnormalities. Imaging modalities that should be considered include MRI of the brain and cervical spine since spinal cord syringomyelia can present with a neuropathic joint in the upper extremity.
References
Citation
Vetter K, Raynor T, Shinde T.Neuropathic Shoulder Joint with Syringomyelia. Appl Radiol. 2025; (1):1 - 4.
doi:10.37549/AR-D-24-0055
February 1, 2025