MRI-guided cryoablation for treatment of neuropathy-mediated sitting pain
Cryoablation of the posterior femoral cutaneous nerve (PFCN) may be a promising, minimally invasive treatment option for long-term relief of pain caused when a patient is sitting. Interventional radiologists from Johns Hopkins University School of Medicine in Baltimore describe a magnetic resonance imaging (MRI) -guided cryoablation technique they developed to relieve chronic neuropathy-mediated sitting pain in an article published in Skeletal Radiology.
Neuropathy of the thin cutaneous branch (CB) of the PFCN typically causes pain and paresthesia, or tingling of the skin, over the inferior buttocks, posterior thigh, and popliteal region. Treatments for temporary, short-term pain relief include perineural injections with steroids and local anesthetics. Currently surgical neurectomy is the only treatment that is used to provide sustained relief of pain.
Cryoablation involves disruption of both axons and myelin sheath with subsequent Wallerian degeneration (a process in which the part of the axon separated from the neuron’s cell body degenerates distal to the injury). It is less likely to cause the formation of neuromas and results in long-lasting interruption of the nerves’ ability to conduct pain.
Cryoablation is performed by temporarily freezing neural tissues through the creation of an ice ball at the tip of a probe. It requires accurate visualization and targeting of the often small nerve in addition to monitoring of the ice ball.
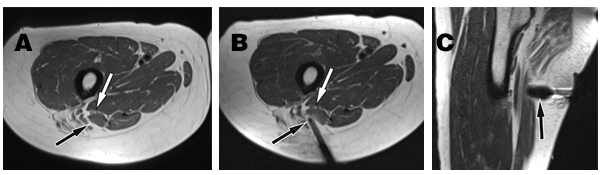
(A) Axial intermediate-weighted MR image of the proximal thigh shows the cutaneous branch of the posterior femoral cutaneous branch (black arrow) next to the hamstring muscles and the sciatic nerve (white arrow). (B) Axial intermediate-weighted MR image of the proximal thigh shows the cryoablation probe (black arrow) in contact with the cutaneous branch of the posterior femoral cutaneous nerve before creation of the ice ball. The white arrow shows the sciatic nerve. (C) Sagittal intermediate-weighted MR image of the proximal thigh shows the grown ice ball (black arrow) as an area of signal void. Courtesy of J. Fritz, Department of Radiology, Johns Hopkins University School of Medicine.
The authors believe that interventional MRI is well suited for the technique because the high spatial and soft-tissue resolution of MRI enables visualization of the less than 1-mm thin posterior femoral cutaneous nerve and the monitoring of the cryoablation ice ball. The distance from the outer margin of the cryoablation zone to the sciatic nerve also needs to be monitored. The MRI monitoring vizualizes the cryoablation zone as a signal void, allowing for verification that the ice ball reaches the cutaneous branch of the PFCN while maintaining a safe distance from the sciatic nerve.
Description of the procedure
An axial intermediate-weighted high spatial resolution MRI was performed to identify the cutaneous branch of the PFCN using a multi-channel body surface coil and table element coils in parallel. The body surface coil was exchanged with a 19-cm loop coil. After the administration of a sedative, a nerve block was performed, displayed on axial intermediate-weighted MR images. The injection needle was replaced with a cryoablation probe, using the same technique and pulse sequence as for the injection needle. After the contact of the cryoablation needle with the targeted nerve was visualized on MRI, cryoablation was performed and ice ball growth was monitored using continuous MRI acquisition at a frame rate of 21 seconds and axial intermediate-weighted MRI.
This procedure took one hour 20 minutes. The patient was an active 66-year-old woman. The authors reported that the patient remains in remission seven months following the treatment.
Potential for cryoablation as a treatment for pain
Principal investigatorJan Fritz, MD, director of the interventional MRI service and an assistant professor of radiology and radiological science in the Section of Musculoskeletal Radiology, told Applied Radiology that he and his colleagues were planning a clinical trial to compare the clinical outcomes of cryoablation and surgical neurectomy. The researchers have not performed this treatment on other patients who experience pain when sitting, but are considering it for several patients currently being treated if their perineural injections are not effective. However, they have been treating bone lesions, such as osteoid osteomas, aneurysmal bone cysts and metastases and other peripheral nerves of the human body with MR-guided cryoablation.
“We had an ideal candidate. However, this technique is applicable to a wide spectrum of patients. MRI-guided cryoablation may also be a treatment option for patients who do not qualify for surgery. While some patients will require general anesthesia, the majority of patients can undergo this procedure with moderate sedation or local anesthesia,” said Dr. Fritz.
REFERENCE
- Joshi DH, Thawait GK, Del Grande F, Fritz J. MRI-guided cryoablation of the posterior femoral cutaneous nerve for the treatment of neuropathy-mediated sitting pain. Skeletal Radiol. Published online March 15, 2017.