MR May Detect Brain Changes Before Symptoms of Dementia Appear
 According to a study in Radiology, an advanced MR technique shows promise in helping understand early structural changes in the brain before symptoms of dementia become apparent. The research indicates the structural integrity of the brain’s white matter, as measured with an advanced MR technique, is lower in cognitively normal people who carry a genetic mutation associated with Alzheimer’s disease than it is in non-carriers. Researchers said the findings show the promise of widely available imaging techniques in helping to understand early structural changes in the brain before symptoms of dementia become apparent.
According to a study in Radiology, an advanced MR technique shows promise in helping understand early structural changes in the brain before symptoms of dementia become apparent. The research indicates the structural integrity of the brain’s white matter, as measured with an advanced MR technique, is lower in cognitively normal people who carry a genetic mutation associated with Alzheimer’s disease than it is in non-carriers. Researchers said the findings show the promise of widely available imaging techniques in helping to understand early structural changes in the brain before symptoms of dementia become apparent.
People who carry the autosomal dominant Alzheimer disease (ADAD) mutation have a higher risk of Alzheimer’s disease. The mutation is linked to a buildup of abnormal protein called amyloid-beta in the brain that affects both the gray matter and the signal-carrying white matter.
“It’s thought that the amyloid deposition in the gray matter could disrupt its function, and as a result the white matter won’t function correctly or could even atrophy,” said study lead author Jeffrey W. Prescott, M.D., Ph.D., neuroradiologist at the MetroHealth Medical Center in Cleveland.
An earlier study by Dr. Prescott and colleagues on patients with sporadic Alzheimer’s disease, which comprises 99% of cases, found that white matter structural connectivity, as measured with the MR technique diffusion tensor imaging (DTI), degraded significantly as patients developed more amyloid burden.
“The current work extends these results by showing that similar findings are detectable in asymptomatic at-risk patients,” said Jeffrey R. Petrella, M.D., professor of radiology at Duke University and senior author on both studies.
In the new study, Dr. Prescott and colleagues used data from the Dominantly Inherited Alzheimer Network (DIAN) to compare ADAD mutation carriers with non-carriers to see if there were changes in structural connectivity that could be related to the mutation.
The study participants included 30 mutation carriers, mean age 34 years, and 38 non-carriers, mean age 37. The participants all had normal cognition when they underwent structural brain MR and DTI.
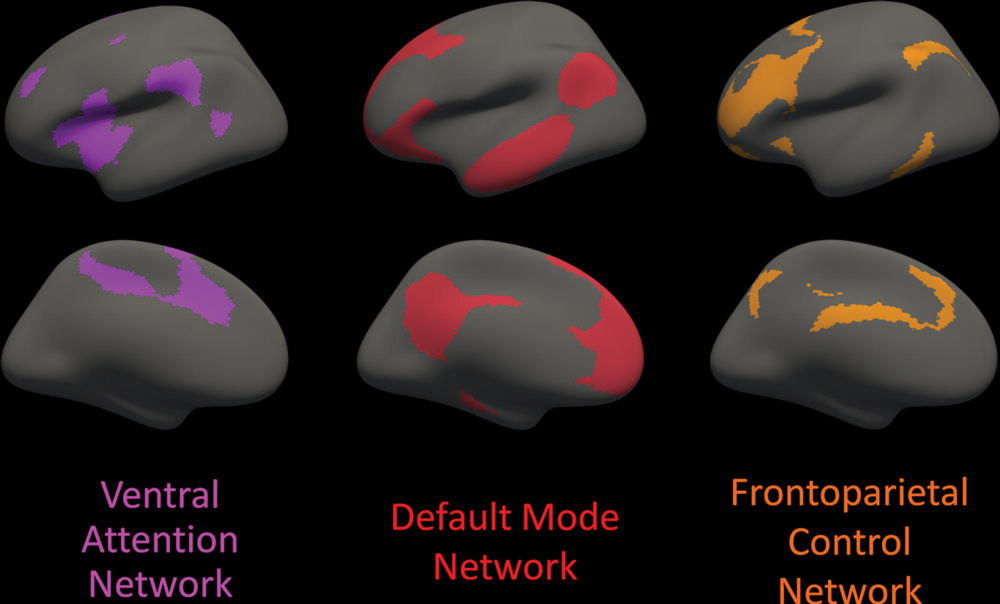
Analysis showed that mutation carriers had lower structural connectivity in the frontoparietal control network, which connects areas mainly in the parietal and frontal lobes, two regions known to be involved with Alzheimer’s disease. Among mutation carriers, there was a correlation between expected years until onset of symptoms and white matter structural connectivity in the frontoparietal control network, even when controlling for amyloid plaque burden.
“This suggests that DTI measures of network integrity may serve as a surrogate for the brain’s resilience to pathologic attack,” Dr. Petrella said.
“We used a network measurement called global efficiency, in which a decreased efficiency can be taken as a breakdown in the organization of the network,” Dr. Prescott added. “The results show that for mutation carriers, global efficiency would decrease significantly as they approach the estimated age of symptom onset.”
The study findings support a potential role for imaging-based identification of structural changes of the brain in people at genetic risk for early-onset Alzheimer’s disease in understanding how genes influence the disease process that leads to dementia.
“This shows the potential of MR as an evaluation tool in patients who are deemed at-risk for Alzheimer’s disease before they develop symptoms,” Dr. Prescott said. “Use of these advanced MR techniques could help further refine identification of at-risk patients and risk measurements.”
The findings also point to a role for imaging in studying therapeutic drugs to treat Alzheimer’s disease. While the majority of trials so far have been performed with patients who already have Alzheimer’s disease or cognitive impairment, earlier identification and treatment of patients at risk represents a more promising avenue for preventing or at least delaying the onset of dementia.”
“One potential clinical use of this study tool would be to add quantitative information to risk factors like family history and use that to help identify patients early, when they may benefit from treatment,” Dr. Prescott said. “But until we have an effective treatment, we will have to wait for that to be implemented.”
The researchers hope to do a follow-up using advanced imaging and updated data from the DIAN network to evaluate the progression of Alzheimer’s disease in the study participants.
Related Articles
Citation
MR May Detect Brain Changes Before Symptoms of Dementia Appear. Appl Radiol.
October 12, 2021